Integration of Primary Care and Public Health (Position Paper)
Introduction
The United States health care system has been consistently ranked as one of the worst in terms of cost and health outcomes when compared to other industrialized nations.1,2 This has occurred despite spending nearly twice as much on health care as a share of its economy when compared to many other industrialized nations. In one study comparing the United States to 13 other high-income countries, Americans had among the shortest life expectancy, the highest infant mortality rates, the highest obesity rates, the greatest prevalence of at least two chronic conditions, and a higher rate of mortality as a result of ischemic heart disease than all but one other country in the study.1
While these health outcomes are staggering, there have been efforts to reinvigorate the health system by focusing on creating integrated, high-value health care that positions family physicians at the front line of primary care. Family physicians are “the first contact with health services, [and] facilitates entry to the rest of the health system.”3 This role comes with family physicians’ ability to recognize individual risk factors of patients and intervene, paralleled with their growing awareness of the social, environmental, and community determinants of health.4,5,6,7
Health equity scholars use a metaphor of a “stream” of causation to illustrate how social factors impact health (Figure 1). The “downstream” factors include issues that medicine and public health typically deal with—morbidity and mortality, access to health care, behavioral risk factors, and living conditions. The questions raised from this illustration are: “Why are so many people sick?” and “Why are there such great differences among groups?” The answers lie in the “upstream” factors, which include governance, culture, and societal values. These, as well as economic, social, and public policies, are the factors that lead to long-held social inequities.8,9 To understand how social factors impact health, it is important to understand how risk factors are shaped upstream and how differences in living conditions and exposures are physically embodied by individuals downstream.7
Figure 1: Conceptual Framework for How Social Factors Influence Health
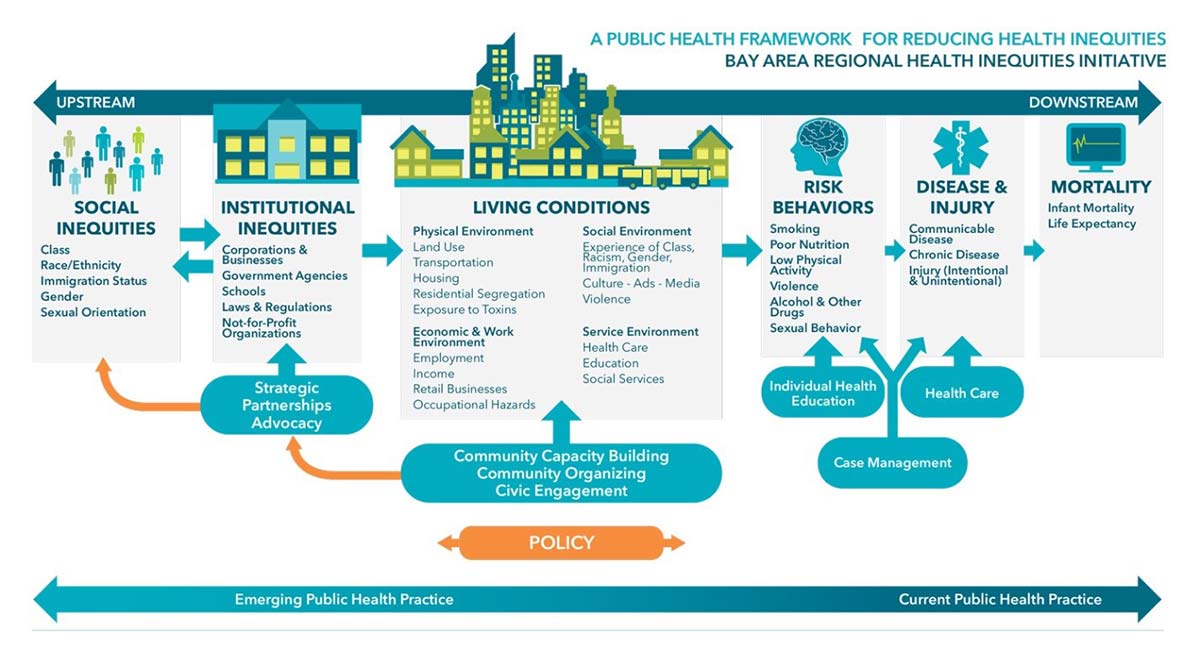
Used with permission from the Bay Area Regional Health Inequities Initiative (BARHII). For broad system change to succeed, family medicine must align with the public health sector to promote community-oriented primary care (COPC)—focused on “upstream,” as well as “downstream” factors—to create a whole-person concept of health.
Call to Action
The American Academy of Family Physicians (AAFP) urges its members to become informed about the importance, value, and movement toward integrating primary care with public health. Family physicians play a critical role in this integration and can continue to contribute through inclusion of local, regional, state, and national public health partners within the medical neighborhood.
The AAFP also urges all national, state, federal, and private sector institutions to partner with primary care and public health entities to ensure a more integrated care delivery system that improves population health. Bold initiatives throughout the health sector are necessary for successful integration.
In order to meet these needs, the AAFP calls for action in the following areas:
Physician Level
- Understand the role public health has to play for you, your patients, and the community you serve
- Demonstrate awareness of integration efforts between primary care and public health
Practice Level
- Redefining population based on the public health definition as geographic, as opposed to a practice patient panel
- Identify critical social factors that impact patient health, leveraging the EveryONE Project and data collection on social determinants of health (SDoH) in electronic health records (EHRs)
- Ensure community voices in practice planning and decisions using community health needs assessments, community boards, and patient and family advisory councils
- Continuous collaboration and communication to with the public health infrastructure to operate as a continuous unit with a common goal
Community-Leadership Level
- Facilitate collaboration and communication amongst health systems and public health organizations
- Drive change within hospitals or health systems to partner with public health organization
- Work with local organizations and community groups to foster discussions and solutions around historic and current structural racism and biases that lead to inequity in the community
- Educate local government, private industries, and other entities about how social factors impact health
Educational Level
- Drive change within undergraduate and graduate medical education to ensure physicians of tomorrow are prepared for a more integrated system
- Prepare the physicians of the future for population health-based roles within the private sector, where business, public health, and health equity increasingly align
Advocacy Level
- Work for adjustments in payment models (e.g., advanced primary care) and increases in primary care spending to facilitate integration work at the practice and community level
- Work with local, state, and national governments to adopt a Health in All Policies approach as a means to ensure governmental infrastructure and policies foster integration
- Work with local, state, and national partners to improve functionality and utility of EHRs that support data infrastructure and interoperability between primary care and public health, including community benefit organizations
- Advocate for regulatory frameworks and economic incentives that increasingly ensure that public health and population health are critical to private sector health care efforts, as opposed to “orphaned efforts”
Through these and other actions, the AAFP, its constituent chapters, and its individual members will be the bold champions of the integration of primary care and public health to meet the goals of promoting population health, which results in improving the health of the nation.
Population Health
Population health is a term frequently used in both health care and public health. It has been used to mean different things, depending on context and perspective. In order to assist AAFP members to understand population health, the definition below defines population health from the perspective of the family physician.
Population health is “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.”10 The population being considered may vary based on an individual’s perspective and goals. For family physicians, the most obvious “group of individuals” is their patient panel. This is where most AAFP members focus their energies and where they often have the greatest impact. Population health also includes the health status and outcomes of the larger communities in which the physician and patient belong. It is essential when caring for their patients that family physicians consider the factors beyond the walls of their practice that influence their patients’ health. The family physician must consider the social and physical environments in which their patients live and work in order to effectively improve health outcomes.
As the health care system works to integrate primary care and public health, family physicians will have more opportunities to partner with community groups and advocate for policies, resources, and interventions in their communities that influence SDoH and improve health outcomes. Evaluating and measuring how primary care and public health work together may assist physicians, practices, and policymakers as they align local resources to improve population health.
A recent community population health index combines local primary care, public health, and the SDoH to provide a county-level understanding of population health.11 While fairly new, the idea of measuring the combined efforts of primary care and public health to positively impact medical and social outcomes of health will be crucial to ongoing population health services and activities.
A push for the integration of primary care and public health arises from the realignment in care design to focus on population health. Population health, as currently described throughout the literature, is defined as health outcomes of a group of individuals, including the distribution of outcomes within the defined group.10,12 However, some question whether this definition represents what we mean when we focus on population health, and confusion arises due to the disjointed definitions of what we mean by a population.
Public health agencies define populations based on residential location, stratified by demographic factors, such as race, ethnicity, gender, age, language, disability, or disease status.10,13 When considering the appropriate delivery of COPC and delivering the promise of a community of solutions, this definition stands out as the most reasonable, given that the social, environmental, and community determinants of health are based on geographic neighborhoods.12 A shift to such a definition requires a large professional culture framework shift from the current medical definition of population as an aggregate of individuals for whom an individual health care entity has provided care to over a period of time.14 This definition has guided the medical profession to its current thinking, which aligns with many of the quality standards (e.g., National Council on Quality Assurance’s Healthcare Effectiveness Data and Information Set (HEDIS), Centers for Medicare & Medicaid Services (CMS), accountable care organization [ACOs], etc.).
The distinction in definition and the difficulty in making this leap to the public health sector's definition is made more difficult by the occasionally reductionist viewpoint of medicine as a business—a viewpoint that often further perpetuates health inequities. With large scale changes in insurance coverage and changes in access to care, it will be that much more important to define geographically where the population lives and provide for much greater opportunities to align with public health on initiatives.
Public health competencies and tools are crucial for this realignment to facilitate a better understanding of the needs of the population, and to prioritize activities according to the epidemiological, organizational, and economic trends.15 Furthermore, like nephrons, each contributing to a piece of renal function, each medical home unit with its medical neighborhood within the same community can lead to improved health and wellness regionally and so on up to a national level. However, until our definition of population aligns, we will never align the individual and community forces that can best foster health for all.
Community-oriented Primary Care (COPC)
The inclusion of public health in the medical neighborhood is an essential component of integration. However, it is critical that it be viewed as a seamless unit in care delivery and not as an entity fully outside of the medical home unit, as this continues the legacy of silos of care delivery that has been ongoing. It was this notion and concern about care delivery “turf” that led to the schism of the two fields at the turn of the 20th century. This also further perpetuates the importance of aligning population definitions amongst primary care and public health to ensure our goals are congruous.
To deliver the promise of a “community of solution” and commitment to deliver community care, we must emphasize COPC. COPC is based on the principles of epidemiology, primary care, preventive medicine, and health promotion that sustains the goal of integration, as well as the goal of population health. COPC can positively impact the unique health needs of communities by utilizing and encouraging a coordinated, collaborative approach to primary care.16,17,18,19
Role of the Family Physician
The current role of family physicians within the health care system inherently holds many of the characteristics needed for a public health-primary care collaboration. Primary care activities, such as clinical preventive services, early diagnosis and intervention, quality-driven and evidence-based care, health promotion, and health advocacy, reinforce public health activities. Likewise, public health activities, such as population surveillance, disease control, health promotion and interventions based on determinants of health, injury prevention, and policy formation facilitate primary care’s ability to function within the health care system. Indeed, despite operating independently for decades, the overlap and contribution of each with a common goal of both individual and population health is substantial.
Many family physicians are already working with their local, regional, and state health departments and public health offices. Care of the individual, the importance of the physician-patient relationship, and that personal connection remains a central focus for the family physician. The practice transformations that come with COPC and payment models based on targets and meaningful use are already altering the way we approach care for patient panels and more importantly, communities. Family physicians who are not actively involved with public health activities are encouraged to do so, as these connections can fill in a gap in resources for health educators, community health workers, and outreach services. Successful integration with local public health and community services can free up physician time and practice resources for other aspects of patient-centered care. Additionally, in times of pandemics or disease outbreaks, a strong connection between primary care and public health can aid in effective dissemination of guidance, supplies, testing, contact tracing, and vaccines.
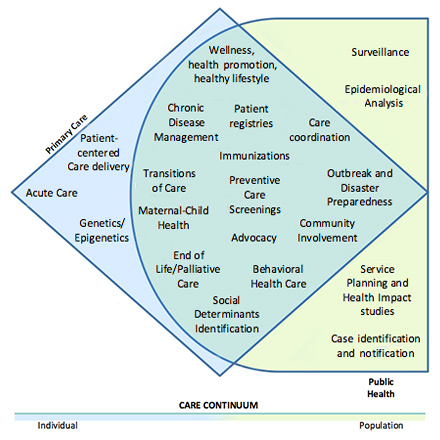
The role of family physicians in the integration of primary care and public health will be significant, as family medicine is poised to be the leader of the new culture of medicine. Health systems, as well as educational institutions, are tasked with providing and promoting community health. They will undoubtedly be looking to the primary care specialty for advice and leadership. These leadership roles must start, however, at the individual physician level and move up through the care continuum to the practice level (Figure 2). Each physician has a part to play at a personal level and being informed about integration, its importance, the value it brings, and the successes it has achieved is the first step. The comprehensive role of the family physician with integration occurs at all levels within the system.
Figure 2: Primary Care and Public Health Care Continuum
Changing Landscape
With a new shared understanding of the definition of population, the integration of primary care and public health can foster an effective collaboration that understands that the health of a population is not simply a product of functionality or funding of health care services. Rather, it includes the conditions in which people are born, grow, live, work, and age, and encompasses inequities in power, money, and resources.20 The emphasis on SDoH supports the important role of primary care. With a greater emphasis on health equity, family physicians stand poised to serve as leaders who understand the role of SDoH and the impact of climate change, seeing its effects in the patients and communities they serve.21 Within this role, family physicians should continue leveraging available technologies, including telehealth, patient portals, and even social media to reduce their carbon footprint and provide multiple access points for patients to meet a variety of needs in their community.
Such technology, and the skills to access it, were necessary to adapt to the challenges of the COVID-19 pandemic, where health systems turned to family physicians to fill multiple roles across many settings. Family physicians have the tools and skills to play a significant role in disaster preparedness and relief efforts.22 Amid this changing and challenging landscape, there exists much opportunity for implementation of changes that will impact the structure of the health care system and support further integration efforts.
Structural Implementation
As system and delivery models change with an emphasis on population health with primary care and public health integration, pipeline and workforce issues must also be adapted. This includes both changes to undergraduate and graduate medical curriculum, as well as faculty development programs to ensure faculty of medical schools and residency programs are able to provide students with the tools needed.
Traditional undergraduate medical education occurs in large, tertiary care academic institutions with the majority of rotations and experiences being hospital based. There are no models in the undergraduate level for what best prepares students for practice with a population health focus—other than those from Canada and Europe whose medical education systems differ from those in the United States.23 As medical schools seek to review and evaluate current population health curricula, departments of family medicine are poised to lead and must play a critical role in this process. Many academic family medicine departments have implemented COPC curricula, population health teaching, preventive care programs, and community outreach within family medicine and ambulatory clerkships that are likely to be the foundation for such educational transformation. Additionally, many large academic medical centers are creating health incubators and start-up companies, actively designing the future of health care and often public health. Family physician faculty and family physician learners must be actively involved in such efforts wherever possible, with curricular integration as a goal.
At the graduate medical education level, with initiation of the Milestones requirements, the Centers for Disease Control and Prevention (CDC) has taken the lead to develop academic partnerships with organizations to facilitate integration, as well as to develop population health milestones to evaluate the feasibility and direction to incorporate these elements into residency education.24,25
The public health educational needs of practicing family physicians must also be emphasized and supported. Indeed, the current proliferation of executive Master of Public Health and Master of Business Administration programs, as well as a range of new certification boards subspecializing in lifestyle medicine, obesity medicine, culinary medicine, and other subjects, points to both a need and a market demand among primary care physicians and others for postgraduate training in public health, health equity, and systems-based care. A number of medical organizations and specialty societies, including the AAFP, have been involved in creating tools for family physicians to understand and leverage population health within their practices. However, development of formal postgraduate education that does not remove practicing family physicians from their communities has lagged somewhat. Such efforts should be encouraged, and family physicians should seek to shape their continued professional development to ensure appropriate continuing population health education throughout their careers.
At the practice level, many of the frustrations that arise as primary care and public health entities attempt to address the “streams” of causation comes from the lack of direct ability to reshape the environments that affect health and behaviors. However, community-based efforts can begin to address some of the inadequacies in the design of systems that lead to the current inequities. Family physicians often serve as a bridge between the community and the public health sector to facilitate conversations around bias and structural racism. This can begin with internal practice-based implicit bias trainings.26 Integration efforts at the community level, working with community and practice-based research can facilitate the development of evidence-based structural frameworks for addressing health disparities. However, this work will require additional partners to make the essential policy changes needed.
Therefore, collaboration must include governmental agencies, businesses, and community-based organizations who are best positioned to create policies and practices that promote healthy environments. This approach, called Health in All Policies, “assists leaders and policymakers to integrate considerations of health, well-being, and equity during the development, implementation, and evaluation of policies and services.”27 Advocacy for approaches at the local, state, and national level are essential to building a governmental infrastructure that sustains integration efforts.
This approach must also facilitate mechanisms to further define the value proposition for integration. Systems must align to support integration, including payment systems that foster primary care, such as primary care spend and advanced primary care payment models.28,29 This includes aligning incentives around factors that improve overall health of communities and patient-centered metrics reflective of advancing health, as opposed to solely advancing health care.
Finally, family physicians must recognize the increasing role of the private sector in creating and maintaining the health of populations. While public health has always relied on private industry as an integral partner, the United States is rapidly entering a period where private industry is playing an increasing role in duties once assigned to the public sector and in shaping the health of communities. Large financial holding corporations are actively purchasing critical segments of health infrastructure, and both established businesses and start-up companies are creating health tools, data infrastructure, and societal conditions that will determine the underlying health of populations and guide public health efforts.
Advocacy efforts, educational reforms, and even the professional culture of family physicians must shift to affirm the board room—and not only the exam room—as an essential place for family physicians to impact public health priorities, anticipate and shape changes in a proactive manner, and support family physicians who choose to lead clinical and public health integration in the business world.
Resources
American Academy of Family Physicians Patient Care Resource
These resources are an up-to-date repository of public health-related information, including clinical recommendations, immunizations, and public health issues in different areas of patient care in the scope of family medicine.
The Practical Playbook II (https://www.practicalplaybook.org/)
This collaborative effort from the de Beaumont Foundation, Duke University, and the CDC provides an overview of the principles of integration, the value of integration, stages and strategies for integration, and success stories and examples of clinical and community settings where integration efforts are already occurring.
Association of State and Territorial Health Officials (ASTHO) Population Health Forum (https://www.astho.org/Programs/Access/Primary-Care-and-Public-Health-Integration)
This national collaborative, whose work is directed at advancing the Strategic Map for Integration of Primary Care and Public Health, was generated through the work of ASTHO, the Institute of Medicine (IOM), and the CDC. Efforts have focused on successes, value proposition, resources, measurements, communications, and workforce issues.
Center for Disease Control Division of Scientific Education and Professional Development
This resource provides information regarding the CDC’s work in integration with educational resources, as well as information on the CDC’s Milestones project for population health education.
Health Resources and Services Administration (HRSA) Public Health Initiative
This resource provides information regarding HRSA’s work in integration with information on integration of oral and behavioral health issues into the effort.
References
- Squires D, Anderson C. U.S. health care from a global perspective: spending, use of services, prices, and health in 13 countries. The Commonwealth Fund. Accessed October 2, 2020. www.commonwealthfund.org/publications/issue-briefs/2015/oct/us-health-care-global-perspective
- Davis K. Stremikis K, Squires D, Schoen C. Mirror, mirror on the wall, 2014 update: how the U.S. health care system compares internationally. The Commonwealth Fund. Accessed October 2, 2020. www.commonwealthfund.org/publications/fund-reports/2014/jun/mirror-mirror-wall-2014-update-how-us-health-care-system
- Starfield B, Shi LY, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502.
- Sherin K, Adebanjo T, Jani A. Social determinants of health: family physicians’ leadership role. Am Fam Physician. 2019;99(8):476-477.
- World Health Organization (WHO). Commission on Social Determinants of Health – final report. Accessed October 2, 2020. www.who.int/social_determinants/final_report/en/index.html
- Kovach KA, Reid K, Grandmont J, et al. How engaged are family physicians in addressing the social determinants of health? A survey supporting the American Academy of Family Physician’s health equity environmental scan. Health Equity. 2019;3(1):449-457.
- American Academy of Family Physicians (AAFP). Advancing health equity by addressing the social determinants of health in family medicine (position paper). Accessed October 2, 2020. www.aafp.org/about/policies/all/social-determinants-health-family-medicine.html
- World Health Organization (WHO). A conceptual framework for action on the social determinants of health. Accessed October 2, 2020. www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf
- Bay Area Regional Health Inequities Initiative (BARHI). A public health framework for reducing health inequities. Accessed October 2, 2020. www.barhii.org/barhii-framework
- Kindig DA, Stoddart G. What is population health? Am J Public Health. 2003;93(3):380-383.
- Health Affairs Blog. A new “PPE” for a thriving community: public health, primary care, health equity. Accessed October 2, 2020.www.healthaffairs.org/do/10.1377/hblog20200922.631966/full/
- Kindig DA. Understanding population health terminology. Milbank Q. 2007;85(1):139-61.
- Centers for Disease Control and Prevention (CDC). Health disparities among youth. Accessed October 2, 2020. https://www.cdc.gov/healthyyouth/disparities/index.htm
- Gourevitch MN, Cannell T, Boufford JI, Summers C. The challenge of attribution: responsibility for population health in the context of accountable care. Am J Prev Med. 2012;42(6S2):S180-3.
- Scutchfield FD, Michener JL, Thacker SB. Are we there yet? Seizing the moment to integrate medicine and public health. Am J Public Health. 2012;102(Suppl 3):S312-S316.
- National Commission on Community Health Services. Health is a Community Affair. Report of the National Commission on Community Health Services. Cambridge, MA: Harvard University Press; 1967.
- American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACOP), American Osteopathic Association (AOA). Joint principles of the patient-centered medical home. Accessed October 5, 2020. www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf
- Longlett SK, Kruse JE, Wesley RM. Community-oriented primary care: critical assessment and implications for resident education. J Am Board Fam Pract. 2001;14(2):141-147.
- O’Connor PJ. Community-oriented primary care in a brave new world. Arch Fam Med. 1994;3(6):493-494.
- Marmot M. Health equity in England: the Marmot review 10 years on. BMJ. 2020;368:m693.
- Wellbery CE. Climate change health impacts: a role for the family physician. Am Fam Physician. 2019;100(10):602-603.
- American Academy of Family Physicians (AAFP). Disaster relief/disaster preparedness. Accessed October 6, 2020. www.aafp.org/family-physician/patient-care/current-hot-topics/health-emergencies/disaster-relief-preparedness.html
- Hirsch DA, Ogur B, Thibault GE, Cox M. “Continuity” as an organizing principle for clinical education reform. N Engl J Med. 2007;356(8):858-866.
- Chappel D, Maudsley G, Bhopal R, Ebrahim S. Public health education for medical students. A guide for medical schools. Accessed October 6, 2020. www.phpc.cam.ac.uk/files/2014/03/PublicHealthEducation.pdf
- Nasca TJ, Philibert I, Brigham T, Flynn TC. The next GME accreditation system – rationale and benefits. N Engl J Med. 2012;366:1051-1056.
- American Academy of Family Physicians (AAFP). Implicit bias resources. The EveryONE Project. Accessed October 6, 2020. www.aafp.org/family-physician/patient-care/the-everyone-project/toolkit/implicit-bias.html?cmpid=everyone_ot_hops_evotool_pdf_trainingmaterials
- World Health Organization (WHO). Adelaide statement on Health in All Policies. Government of South Australia. Accessed October 6, 2020. www.who.int/sdhconference/resources/hiapfinal.pdf
- American Academy of Family Physicians (AAFP). Primary care spend. Accessed October 6, 2020. www.aafp.org/dam/AAFP/documents/advocacy/payment/apms/BKG-PrimaryCareSpend.pdf
- American Academy of Family Physicians (AAFP). Advanced primary care: a foundational alternative payment model. Accessed October 6, 2020. www.aafp.org/dam/AAFP/documents/events/fmas/BKG-APC-APMOverview.pdf
(2015 COD) (January 2022 COD)