
Am Fam Physician. 1998;57(11):2695-2702
Eyelid problems range from benign, self-resolving processes to malignant, possibly metastatic, tumors. Inflammation, infection, benign and malignant tumors, and structural problems such as ectropion, entropion and blepharoptosis may occur. Fortunately, most eyelid disorders are not vision-threatening or life-threatening; however, many cause irritative symptoms such as burning, foreign-body sensation or pain. Blepharitis, or eyelid inflammation, one of the most common problems, is characterized by erythematous eyelids with accumulation of debris along the eyelid margin. Malignant eyelid tumors may be associated with lash loss and erosion of normal eyelid structures. Recognition and diagnosis of these problems are crucial to their proper management. Warm compresses and antibiotics suffice for many conditions, while excision, cryotherapy or laser treatment are required for some.
Eyelids are crucial to the health of the underlying eye. They provide coverage of the cornea and aid in the distribution and elimination of tears. An exposed cornea will develop epithelial defects, scarring, vascularization or infection. Resulting symptoms include ocular irritation, pain and loss of vision. Eyelid closure distributes tears over the surface of the eye and pumps them through the lacrimal puncta into the tear duct (Figure 1). Thus, tearing or epiphora may result from various eyelid disorders.
Anatomically complex, the eyelids consist of an anterior layer of skin and orbicularis oculi muscle, and a posterior layer of tarsus and conjunctiva (Figure 2). Contraction of the orbicularis muscle, innervated by the seventh cranial nerve, closes the eyelids. The levator muscle, innervated by the third cranial nerve, and the sympathetically innervated Müller's muscle raise the upper lid. The orbital septum, originating from the orbital rim, inserts into the upper lid just above the tarsal border and into the lower lid just below the tarsal border. The orbital septum limits the spread of infection and hemorrhage from the eyelid to the posterior orbital structures.
Several glands along the eyelid margin contribute to the lipid component of the tear film. These glands commonly become inflamed. The meibomian glands, approximately 30 per lid, are present within the tarsus. The pilosebaceous glands of Zeiss and the apocrine glands of Moll are located anterior to the meibomian glands within the distal eyelid margin.
In evaluating an eyelid problem, the physician should obtain focused but complete information from the patient. Recognition of possible malignant lesions is essential. It is important to ask questions about the duration of the problem, a change in size or appearance of an eyelid lesion or the recurrence of a tumor that has been previously treated. In general, lesions that have not changed for a long time are benign. A previous history of skin cancers should also be noted.
Examination of the eyelids should be systematic, beginning with the upper lid. A ptotic upper lid may droop below the normal resting lid position of 2 mm below the superior corneoscleral junction. Redundant upper lid tissue may hang into the visual axis. Eyelid retraction or inability to close the lid should be assessed. Eyelid lesions should be examined for size, location, pigmentation and associated lash loss or ulceration.
Inspection of the lower lid may reveal lower lid malpositions such as entropion (inward turning) or ectropion (outward turning). Ectropion of the inferior punctum, through which tears flow to the lacrimal sac, may result in tearing. Misdirected eyelashes may rub on the globe.
Benign Inflammatory Eyelid Processes
Blepharitis
One of the most common eyelid problems is blepharitis, or inflammation of the eyelid margin. Patients typically experience itching, burning, mild foreign-body sensation, tearing and crusting around the eyes on awakening. On examination, the eyelid margins are erythematous, and thickened with crusts and debris within the lashes (Figure 3). Conjunctival injection or a mild mucus discharge may be present. Blepharitis occurs with chronic bacterial lid infection, meibomian gland dysfunction, seborrhea and acne rosacea that affects the eye, known as ocular rosacea.1 The diagnosis of rosacea is supported by the presence of dilated telangiectatic blood vessels on the lid margins, cheeks, nose and chin.

Treatment of blepharitis consists initially of warm compresses, eyelid scrubs and application of antibiotic ointment. Warm compresses should be applied for 15 minutes twice a day. This step loosens irritating crusts in the eyelashes and melts the oil produced by the meibomian glands, which can occlude the gland orifices. The eyelids should be scrubbed after the warm compress is removed. Baby shampoo mixed with water produces a soapy solution. With the eyelids closed, the eyelid margin region should be gently scrubbed with this solution, using a cotton-tipped applicator, wash cloth or finger. Erythromycin or another antibiotic ointment should then be applied to the lid margin. The ointment should be applied only at bedtime, because it may temporarily blur vision. If an obvious infection is present, antibiotic eye-drops may also be used.
If the condition is unresponsive to treatment, eyelid cultures should be obtained to rule out the possibility of resistant organisms. Oral antibiotics may be used in such cases, or in patients with the diagnosis of ocular rosacea. If severe, blepharitis may result in corneal infiltrates or ulcers. Rarely, sebaceous cell carcinoma may masquerade as unilateral or bilateral intractable blepharitis.
Patients must be cautioned that blepharitis is a chronic disease and that eyelid hygiene may need to be continued indefinitely. When the process is brought under better control, once-daily eyelid scrubs may be sufficient to keep the problem in check.
Chalazion
Chalazia appear most commonly as chronic subcutaneous nodules within the eyelid (Figure 4). Initially, a chalazion may be tender and erythematous before evolving into a non-tender lump. Blepharitis is frequently associated with chalazia.

A chalazion results from the obstruction of the meibomian gland. The blockage of the gland's duct at the eyelid margin results in release of the contents of the gland into the surrounding eyelid soft tissue. A lipogranulomatous reaction ensues. Occasionally, chalazia become secondarily infected.
Management includes warm compresses applied for 15 minutes four times a day. Blepharitis, if present, should be treated. A topical antibiotic may be used if signs of infection are present. If the lesion persists after four weeks of medical therapy, it may be incised and drained. Rarely, the chalazion is injected with steroids; however, this may result in hypopigmentation of the overlying skin.2
Hordeolum
A hordeolum, also known as a stye, is an acutely presenting, erythematous, tender lump within the eyelid (Figure 5). An internal hordeolum involves infection of the meibomian gland and may evolve into a chalazion. An external hordeolum occurs with infection of the more anteriorly located glands of Zeiss or Moll, present just anterior to the lash line. Hordeola usually drain spontaneously after one week of treatment with warm compresses four times a day and topical antibiotic ointment twice daily. Incision and drainage are required for nonresolving lesions.

Benign Noninflammatory Eyelid Lesions
Seborrheic Keratosis
Seborrheic keratoses are pigmented, greasy hyperkeratotic lesions that appear to be stuck on the skin (Figure 6). Commonly occurring in the elderly, these lesions may occasionally become irritated. Surgical excision is curative.

Actinic Keratosis
This flat, flaky, white, scaly lesion occurs in sun-exposed areas. Unlike seborrheic keratosis, actinic keratosis is a premalignant condition. Excisional biopsy should be performed to discover dysplasia or carcinoma-in-situ.
Nevus
Nevi are well-demarcated, flat or elevated, pigmented or nonpigmented congenital lesions (Figures 7 and 8). They may become more pigmented, more elevated or cystic during adolescence or young adulthood. Junctional nevi, occurring at the junction between epidermis and dermis, have some malignant potential. Because of the risk for malignant transformation, pigmented lesions that have changed in appearance should be excised.

Xanthelasma

Molluscum Contagiosum
Found commonly in immunosuppressed as well as immunocompetent patients, these waxy nodules have a central umbilication4 (Figure 10). If present on the eyelids, they may produce a follicular conjunctivitis. These viral lesions may be treated with excision, cryotherapy or curettage, although in many cases they are self-limited and resolve with time.

Hydrocystoma
A hydrocystoma is a translucent cyst located near the lid margin, usually resulting from blockage of the sweat glands of the eyelid. Complete excision may be performed.
Malignant Eyelid Lesions
Basal Cell Carcinoma
Basal cell carcinoma, the most common eyelid malignancy, usually appears in the lower lid and medial canthal region as a firm, pearly nodule5 (Figure 11). Telangiectasia may overlie the nodule, or central ulceration may be present. If located along the lid margin, eyelashes may be missing in the region of the tumor. Extension to the posterior eyelid surface may be detected by everting the eyelid. Although basal cell carcinoma does not tend to metastasize, it may be locally invasive.
Treatment is complete surgical resection with histologic control of margins. Radiation and cryotherapy, which have higher recurrence rates than surgical resection, are used when surgery is not appropriate or possible.
Squamous Cell Carcinoma
Squamous cell carcinoma, although much less common than basal cell carcinoma, behaves more aggressively.6 Erythematous, raised, scaly and centrally ulcerated, these lesions occur frequently on the upper lid. They may arise de novo or from areas of actinic keratosis. Palpation of preauricular and submandibular lymph nodes is crucial to detect potential metastatic spread. Treatment is similar to that for basal cell carcinoma.
Sebaceous Carcinoma
Sebaceous carcinoma occurs in middle-aged to elderly patients and may mimic a chalazion or chronic unilateral or bilateral blepharitis7 (Figure 12). It invades locally and spreads to regional preauricular or submandibular lymph nodes. Distant sites of metastasis include lungs, liver and bone. Mortality increases with increasing tumor size.8 Because of the aggressive nature of these tumors, large or recurrent tumors may require surgical removal of the orbital contents.

Melanoma
Melanoma is a rare pigmented eyelid tumor that must be differentiated from nevi and basal cell carcinoma. During examination of the eye, the physician should always evert the eyelid to look for conjunctival involvement. Change in the appearance of a pigmented lesion warrants excisional biopsy of the lesion. Systemic evaluation for regional or distant metastasis is necessary with the diagnosis of melanoma.
Mechanical Eyelid Disorders
Entropion
Entropion, or inward turning of the eyelid margin (Figure 13), causes irritation, redness and stringy white mucoid discharge.9 Usually occurring in the lower lid, entropion causes eyelashes to rub on the cornea and conjunctiva. Most commonly, entropion occurs in the elderly as a result of age-related changes. Treatment is artificial tear drops and lubricating eye ointment until surgical repair can be performed.

Ectropion
Ectropion, or outward turning of the eyelid margin, causes tearing, ocular irritation and redness10 (Figure 14). The lower eyelid is most commonly involved. Treatment is lubricating tear drops and ointment before surgery. If the skin of the lower lid appears to pull the margin inferiorly in a cicatricial fashion, massage of the lower lid skin with a mild steroid cream once daily for two weeks may be beneficial.
Trichiasis
Trichiasis is a condition of misdirected eyelashes that rub on the cornea, resulting in ocular pain, tearing and redness. Epilation or removal of the misdirected eyelashes ameliorates the symptoms. If the offending eyelashes regrow aberrantly, they may be reepilated or treated permanently with electrolysis or cryotherapy.
Dermatochalasis
Dermatochalasis, or redundant eyelid skin and fat, may result in functional loss of superior vision if the tissue hangs over the eyelid margin into the visual axis. Surgical repair of this age-related problem is termed blepharoplasty.
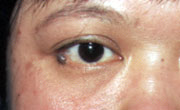
Blepharoptosis
Drooping of the margin of the eyelid, or blepharoptosis, may also cause functional vision loss, depending on the severity of the condition (Figure 15). Etiology includes age-related dehiscence of the levator muscle, Horner's syndrome, third cranial nerve palsy, myasthenia gravis and trauma.11 Treatment is usually surgical, depending on the etiology.

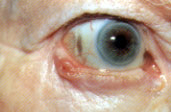
Eyelid Retraction
The normal resting position of the upper lid is 2 mm below the junction of the superior cornea with the sclera, and that of the lower lid is at the junction of the inferior cornea with the sclera (Figure 1). Because the most common cause of eyelid retraction is thyroid ophthalmopathy (Figure 16), the thyroid status of the patient should be evaluated.12 Other causes include midbrain disease, such as tumors or infarcts, or blepharoptosis with compensatory contralateral eyelid retraction. Treatment depends on the underlying etiology.

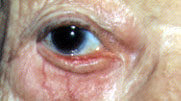
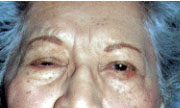
Facial Palsy
Facial palsy results in an inability to close the upper lid and laxity of the lower lid. A frank paralytic ectropion may occur as well (Figure 17, top and bottom). A thorough work-up for the etiology of the facial palsy must be performed.

Treatment of the eyelid problems includes vigorous lubrication of the eye with artificial tear drops and lubricating ointment.13 Plastic wrap, fixed to the skin with ointment, may be placed over the orbital region during the night to create a moisture chamber for the eye. For temporary facial palsies such as Bell's palsy, small external tantalum eyelid weights (manufactured by MedDev, Palo Alto, Calif.; telephone: 650-494-1153) may be easily fixed to the skin with double-sided tape (Figure 18, top and bottom). The weight passively closes the upper lid, protecting the cornea.14 Surgical procedures are performed in patients with permanent palsies.

Blepharospasm
Spasm of the eyelids may be unilateral or bilateral. Unilateral lid spasm may occur in conjunction with unilateral or hemifacial spasm. Hemifacial spasm results most commonly from irritation of the seventh nerve roots by a dilated or tortuous vascular structure (Figure 19). Because tumor is the etiology in up to 1 percent of patients, all patients with hemifacial spasm should receive a magnetic resonance imaging scan of the brain.15
Bilateral blepharospasm is most commonly the result of dry eyes, corneal irritation or benign essential blepharospasm. Brain imaging is not required. Benign essential blepharospasm may be caused by an overexcitatory drive of the basal ganglia. Initial treatment is artificial tear drops and injections of botulinum toxin to weaken the affected muscles.16