
Am Fam Physician. 1998;58(1):199-200
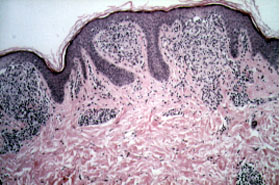
A four-year-old child presented to the office for evaluation of a nonpruritic generalized cutaneous eruption that had been present for six months. Physical examination revealed multiple flesh-colored and tannish-brown papules, from 1 to 2 mm in diameter, on the child's torso, extremities and face (Figure 1). There was no evidence of mucocutaneous or palmoplantar involvement. The child did not have any associated systemic complaints, and a review of systems was normal. A skin biopsy was performed. Histologic examination revealed multiple foci of lymphohistiocytic infiltrates with elongation of the rete ridges around each infiltrate (Figure 2).

Question
Discussion
The correct answer is D: Generalized lichen nitidus. Lichen nitidus is a chronic papular eruption of the skin that most commonly affects children and young adults but has been reported in the elderly.1 The eruption is usually asymptomatic and limited to the chest, abdomen, forearms, buttocks and penis.2 However, multiple clinical variants of lichen nitidus have been described, including generalized, perforating, vesicular, hemorrhagic, spinous, palmoplantar and familial.1–8 The etiology of lichen nitidus is unknown.3
Generalized lichen nitidus is a rare form of the disease with similar lesions that cover a greater body surface area. The clinical diagnosis of localized lichen nitidus is straightforward, but when the lesions disseminate, the diagnosis may become more elusive because of concern over a more aggressive dermatitis. Because of the expanded cutaneous involvement, the differential diagnosis includes pityriasis rubra pilaris, keratosis pilaris, lichen planus, phrynoderma (vitamin A deficiency) and papular mucinosis.
Diagnosis is confirmed by skin biopsy, which demonstrates well-demarcated lymphohistiocytic infiltrates with occasional giant cell formation and elongation of the rete ridges around the lateral margins of the infiltrate.3 These histologic characteristics distinguish lichen nitidus from lichen planus. Lichen planus is characterized by an intense, dermal band-like infiltrate with focal hypergranulosis in the epidermis.
The clinical course of generalized lichen nitidus is variable and often unpredictable; even so, the prognosis is good.1 Often the disease is asymptomatic and the eruption resolves spontaneously, without therapy, after several years.3 Parents of children with generalized lichen nitidus are often more concerned about the child's cosmetic appearance and often request treatment, especially if the face becomes involved. Various treatment recommendations are available for generalized lichen nitidus, but they are usually anecdotal and usually have not been studied in randomized, placebo-controlled clinical trials. Treatment methods include topical steroids, a short course of oral steroids, phototherapy and antihistamines.1–3,9,10 Obviously, some of these treatments may be toxic to children; therefore, treatment should be tailored to the individual patient. The patient described here responded to a short course of topical hydrocortisone valerate cream.