
A more recent article on food allergies is available.
Am Fam Physician. 1999;59(2):415-424
See related patient information handout on food allergy, written by the author of this article.
The term “food allergy” refers to adverse immunologic reactions to food. Food allergy is usually mediated by IgE antibody directed to specific food proteins, but other immunologic mechanisms can also play a role. The primary target organs for food allergic reactions are the skin, the gastrointestinal tract and the respiratory system. Both acute reactions (hives and anaphylaxis) and chronic disease (asthma, atopic dermatitis and gastrointestinal disorders) may be caused or exacerbated by food allergy. The foods most commonly causing these reactions in children are milk, egg, peanuts, soy, wheat, tree nuts, fish and shellfish; in adults, they are peanuts, tree nuts, shellfish and fish. The diagnosis of food allergy requires a careful search for possible causes, confirmation of the cause(s) with supporting tests, including specific tests for IgE (i.e., prick skin tests, radioallergosorbent tests) and, in some cases, oral food challenges. Treatment consists of elimination of the causal food(s) along with medical treatment, including the prompt self-administration of epinephrine in the event of a serious reaction.
Adverse reactions to foods may be toxic or nontoxic.1 Toxic reactions are not related to individual sensitivity but occur in anyone who ingests a sufficient quantity of tainted food. Examples of toxic reactions include reactions to histamine in scombroid fish poisoning or to bacterial toxins in food poisoning. In contrast, non-toxic adverse reactions to food depend on individual susceptibility and are either non–immune-mediated—i.e., food intolerance (Table 1), or immune-mediated—i.e., food allergy. This article focuses on the clinical manifestations of food allergy.
| Gastrointestinal disorders |
| Structural abnormalities: hiatal hernia, pyloric stenosis, Hirschsprung's disease, tracheoesophageal fistula |
| Disaccharidase deficiencies: lactase, sucrase-isomaltase complex, glucose-galactose complex |
| Pancreatic insufficiency: cystic fibrosis |
| Gallbladder disease |
| Peptic ulcer disease |
| Malignancy |
| Metabolic disorders |
| Galactosemia |
| Phenylketonuria |
| Pharmacologic-related conditions |
| Jitteriness (caffeine) |
| Pruritus (histamine) |
| Headache (tyramine) |
| Disorientation (alcohol) |
| Psychologic disorders |
| Neurologic disorders |
| Gustatory rhinitis |
| Auriculotemporal syndrome (facial flush from tart food) |
Allergic Reactions
Allergic reactions to food are either IgE-mediated or non–IgE-mediated (Table 2). The role of IgE-mediated reactions in food allergy is well established. Persons who are genetically predisposed to atopy produce specific IgE antibodies to certain proteins to which they are exposed.2 These antibodies bind to mast cells and other cells in body tissues and to basophils circulating in the blood stream. When a food protein is ingested, the IgE recognizes it on the surface of these cells; mediators (e.g., histamine) are released, and symptoms occur. The symptoms of IgE-mediated reactions typically involve the skin, respiratory system and gastrointestinal tract.3 The pathogenesis of non–IgE-mediated reactions in food allergy is not as clearly defined, but T cells and macrophages most likely play a role. Illnesses caused by these non–IgE-mediated immunologic responses to food affect the same organ systems that the IgE-mediated forms affect.
| Target organ | IgE-mediated disorder | Non–IgE-mediated disorder |
|---|---|---|
| Skin | Urticaria and angioedema | Atopic dermatitis |
| Atopic dermatitis | Dermatitis herpetiformis | |
| Gastrointestinal tract | Oral allergy syndrome | Proctocolitis |
| Gastrointestinal “anaphylaxis” | Enterocolitis | |
| Allergic eosinophilic gastroenteritis | Allergic eosinophilic gastroenteritis | |
| Enteropathy syndrome | ||
| Celiac disease | ||
| Respiratory tract | Asthma | Heiner syndrome |
| Allergic rhinitis | ||
| Multisystem | Food-induced anaphylaxis | |
| Food-associated, exercise-induced anaphylaxis |
Skin
URTICARIA
The skin is a common target organ for allergic responses to food. Acute urticaria is characterized by pruritic, transient, erythematous raised lesions, sometimes accompanied by localized swelling (angioedema). Food allergy accounts for up to 20 percent of cases of acute urticaria4 and is mediated by IgE specific to food protein. Lesions usually occur within one hour after ingestion of or contact with the causal food. Because only 1.4 percent of cases of chronic or persistent urticaria (i.e., lasting more than six weeks) are caused by food allergy,5 a search for a causative food in the initial evaluation of this condition is not generally warranted.
ATOPIC DERMATITIS
Atopic dermatitis usually begins in early infancy and is characterized by a typical distribution (face, scalp and extremities), extreme pruritus and a chronic and relapsing course. This inflammatory skin condition is frequently associated with allergic disorders (e.g., asthma and allergic rhinitis) and with a family history of allergy.6 Evidence suggests that IgE-mediated food allergy plays a pathogenic role in atopic dermatitis, particularly in children,6 although non–IgE-mediated food allergy has also been implicated.7 Clinical studies using double-blind, placebo-controlled food challenges have shown that 37 percent of children with moderate atopic dermatitis have food allergy.8 By contrast, 6 to 8 percent of infants and children in the general population are allergic to some type of food.9
DERMATITIS HERPETIFORMIS
Dermatitis herpetiformis is a chronic papulovesicular skin disorder in which lesions are distributed over the extensor surfaces of the elbows, knees and buttocks.10 The disorder is associated with a specific non–IgE-mediated immune sensitivity to gluten (a protein found in wheat, barley, oat and rye). Although dermatitis herpetiformis is related to celiac disease, patients often appear to have no associated gastrointestinal problems. The rash abates with the elimination of gluten from the diet.
Gastrointestinal Tract
The gastrointestinal tract is another common target organ for IgE-mediated reactions to foods. Symptoms of gastrointestinal “anaphylaxis” occur shortly after the ingestion of an implicated food and include nausea, vomiting, abdominal pain and diarrhea.
ORAL ALLERGY SYNDROME
The oral allergy syndrome is characterized by pruritus and edema of the oral mucosa occurring after the ingestion of certain fresh fruits and vegetables.11 The symptoms rarely progress beyond the mouth. The reaction occurs primarily in patients with allergic sensitivity to pollens and is caused by IgE antibodies directed toward cross-reacting proteins found in pollens, fruits and vegetables.11 Patients with birch-pollen hay fever may have symptoms of oral allergy syndrome after ingesting hazelnut, apple, carrot and celery, whereas patients with IgE sensitivity to ragweed pollen may react to melons (e.g., water-melon or cantaloupe) and banana. Interestingly, patients are usually able to ingest cooked forms of the foods without symptoms because the responsible allergens are destroyed in the heating process. It is crucial to differentiate the symptoms of oral allergy syndrome from the early symptoms of a systemic reaction to food.
CELIAC DISEASE
A number of immunologic reactions to food proteins are not mediated by IgE. Celiac disease presents over a period of months with steatorrhea, flatulence and weight loss. Hypersensitivity to gluten causes the disease, and the characteristic diagnostic feature is extensive flattening of villi in a biopsy specimen taken from the jejunal mucosa.
ALLERGIC EOSINOPHILIC GASTROENTERITIS
Although allergic eosinophilic gastroenteritis is an IgE-mediated disease in some patients, about one half of patients do not exhibit specific IgE antibody to foods. Patients with allergic eosinophilic gastroenteritis have severe reflux, postprandial abdominal pain, vomiting, early satiety and diarrhea. The diagnosis is suggested by the presence of inflammation and significant eosinophilic infiltration of the esophagus, stomach or small intestine. Treatment with a strict avoidance diet using an elemental formula is efficacious in some patients.12
INFANTILE PROCTOCOLITIS
The symptoms of infantile proctocolitis are limited to the lower gastrointestinal tract and are of short duration. The ingestion of the responsible food (usually cow's-milk protein or breast milk from mothers who are consuming cow's milk) provokes diarrhea with blood in the stool, but anemia rarely occurs.
FOOD PROTEIN–INDUCED ENTEROCOLITIS AND ENTEROPATHY
Patients with enterocolitis induced by food protein are often diagnosed in infancy and present with profuse vomiting and diarrhea. When severe, these symptoms may lead to lethargy, dehydration and hypotension (often mimicking bacterial sepsis). The symptoms may be complicated by acidosis. The enterocolitis resolves with elimination of the responsible protein, most often cow's milk or soy.13,14
Patients may also have more indolent food protein–induced gastrointestinal symptoms that are induced by milk, soy, egg, wheat, rice, chicken or fish. These patients, classified as having food protein–induced enteropathy, do not typically experience colitis, and they have a lower incidence of emesis (30 percent) than patients with enterocolitis (90 percent).15
The role of IgE-mediated or non–IgE-mediated food protein sensitivity in cases of infantile colic16 and inflammatory bowel disease17 remains controversial. Although failure to thrive in infants may be associated with malabsorption resulting from food allergy, a restrictive diet imposed by the family can also result in poor growth. This factitious food allergy was diagnosed in 5 percent of children with failure to thrive who were referred to an academic allergy program.18
Respiratory Tract
RHINITIS
The upper respiratory tract can be a target of IgE-mediated food allergy. Symptoms may include nasal congestion, rhinorrhea, sneezing and pruritus. The prevalence of food-induced allergic rhinitis, even among patients referred to allergy clinics, appears to be less than 1 percent, although 25 to 80 percent of patients with documented IgE-mediated food allergy have nasal symptoms during oral food challenges.19
Gustatory rhinitis is rhinorrhea caused by spicy foods. This is not an immunologic reaction; it is mediated by neurologic mechanisms.20
ASTHMA
Food-induced asthma is an IgE-mediated illness that may result from the ingestion of a causative food or from the inhalation of vapors released during cooking or in occupational settings. The prevalence of food-related asthma in the general population is unknown, but this illness has been found to occur in 5.7 percent of children with asthma, 11 percent of children with atopic dermatitis and 24 percent of children with a history of food-induced wheezing.21 The prevalence of food-induced wheezing in adults with asthma is less than 2 percent.22
HEINER SYNDROME
An example of a non–IgE-mediated adverse pulmonary response to food is Heiner syndrome. This uncommon syndrome of infancy is characterized by an immune reaction to cow's-milk proteins with precipitating antibody (IgG) to cow's-milk protein resulting in pulmonary infiltrates, pulmonary hemosiderosis, anemia, recurrent pneumonia and failure to thrive.
Anaphylaxis
Anaphylaxis refers to a dramatic multiorgan reaction associated with IgE-mediated hypersensitivity. Fatal food-related anaphylaxis appears to be more common in patients with underlying asthma.23 Patients who experienced fatal or nearly fatal food-induced anaphylaxis were unaware that they had ingested the incriminated food, had almost immediate symptoms and experienced a delay in receiving adrenaline therapy. In about one half of the patients, a period of quiescence preceded the respiratory decompensation. The foods most often responsible for food-induced anaphylaxis are peanuts, tree nuts (walnut, almond, pecan, cashew, hazel nut, Brazil nut, etc.) and shellfish.23
Food-associated, exercise-induced anaphylaxis occurs in two forms.24 Anaphylaxis may occur when exercise follows the ingestion of a particular food to which IgE-mediated sensitivity is usually demonstrable (e.g., celery) or, less commonly, may occur after the ingestion of any food. Ingestion of the incriminated food with exercise or exercise without ingestion of the food does not result in symptoms.
Controversies and Food Allergies
The relationship of food allergy to a number of clinical entities remains controversial. Food allergy may play a role in a minority of patients with migraine headaches,25 although the pharmacologic activity of chemicals found in some foods (i.e., tyramine in cheeses) is more often responsible.
The role of food allergy in childhood behavior disorders is also controversial. A small subset of children with behavior disorders may be affected by food dyes, but no convincing evidence shows that food allergy plays a direct role in these disorders.26 Unfortunately, unreliable information in the lay press and the use of unconventional and unproven methods, such as “provocation-neutralization,”27 for diagnosing and treating behavior disorders can divert the patient's family from more useful treatments. On the other hand, in children with behavior disorder who also have bona fide allergies, treatment to relieve the symptoms of asthma, atopic dermatitis and hay fever should be pursued.
Diagnosis
INITIAL EVALUATION
An evaluation is warranted in patients who have the common clinical manifestations of food allergy. The initial evaluation, beginning with a thorough history and physical examination, must consider a broad differential diagnosis, including metabolic disorders, anatomic abnormalities, malignancy, pancreatic insufficiency, nonimmunologic adverse reactions to foods and many other disorders that could lead to similar symptoms. Allergic reactions to substances other than foods (e.g., animal dander, molds, dust) must also be considered. Once food allergy is identified as a likely cause of symptoms, confirmation of the diagnosis and identification of the implicated food(s) can proceed.
In patients with acute reactions such as acute urticaria or anaphylaxis, the history may clearly implicate a particular food. In patients with chronic disorders such as atopic dermatitis or asthma, it is more difficult to pinpoint causal food(s). Virtually any food protein can cause a reaction; however, only a small number of foods account for more than 90 percent of adverse food reactions, and most patients are sensitive to fewer than three foods.3,28 In children, the most common foods causing reactions are egg, milk, peanuts, soy, wheat, tree nuts and fish.3,28 Adults most often react to peanuts, tree nuts, fish and shellfish.29
PRICK-PUNCTURE SKIN TESTING
In the evaluation of IgE-mediated food allergy, specific tests can help to identify or exclude responsible foods. One method of determining the presence of specific IgE antibody is prick-puncture skin testing. While the patient is not taking antihistamines, a device such as a bifurcated needle or a lancet is used to puncture the skin through glycerinated extract of a food and also through appropriate positive (histamine) and negative (saline-glycerin) control substances. A local wheal-and-flare response indicates the presence of food-specific IgE antibody, with a wheal diameter of more than 3 mm indicating a positive response.
Prick skin tests are most valuable when they are negative because the negative predictive value of these tests is very high (over 95 percent).30,31 Unfortunately, the positive predictive value is on the order of only 50 percent.30,31 Thus, a positive skin test in isolation cannot be considered proof of clinically relevant hypersensitivity, whereas a negative test virtually rules out IgE-mediated food allergy to the food in question.
IN VITRO TESTING (RAST)
In vitro tests for specific IgE (radioaller-gosorbent tests [RAST]) are more practical than prick skin tests for food allergy screening in the primary care office setting. As with skin tests, a negative result on RAST testing is very reliable in ruling out an IgE-mediated reaction to a particular food, but a positive result has a low positive predictive value. In vitro tests for IgE are generally less sensitive than skin tests; however, when highly sensitive assays are used, the levels of food-specific IgE antibody correlate with clinical reactivity to certain foods (e.g., milk, egg, peanuts, fish).33 Because most patients with food allergy are sensitive to only a few foods3,28 and a small number of foods are responsible for most reactions,3,28 it is usually inappropriate to test for allergies to an extensive number of foods. In the context of a detailed history, selective testing is more likely to reveal causal foods. Measurement of immunoglobulin G4 (IgG4) antibody, provocation-neutralization, cytotoxicity, applied kinesiology and other unproved methods are not useful.34
When patients have a history suggestive of food-related illness and tests for IgE antibody to the food are positive, the first course of action is to eliminate the food from the diet. Further testing is usually not needed in patients with severe, acute reactions. However, if symptoms are chronic (atopic dermatitis, asthma) and/or many foods are implicated, diagnostic oral food challenges may be necessary.
ORAL FOOD CHALLENGES
Double-blind, placebo-controlled food challenges are considered the gold standard for diagnosing food allergy.3,30,35 The procedure is labor intensive but can be modified for an office setting.35 Patients avoid the suspected food(s) for at least two weeks, antihistamine therapy is discontinued according to the elimination half-life of the specific medication, and doses of asthma medications are reduced as much as possible. After intravenous access is obtained, graded doses of either a challenge food or a placebo food are administered. The food is hidden either in another food or in opaque capsules.
Medical supervision and immediate access to emergency medications, including epinephrine, antihistamines, steroids and inhaled beta agonists, and equipment for cardiopulmonary resuscitation are required because reactions can be severe. During the challenge, patients are assessed frequently for changes in the skin, gastrointestinal tract and respiratory system. Challenges are terminated when a reaction becomes apparent, and emergency medications are given as needed. Patients are also observed for delayed reactions. If allergy to only a few foods is suspected, single-blind or open challenges may be used to screen for reactivity.
Negative challenges are always confirmed with open feeding of a larger, meal-sized portion of the food. Oral challenges should usually not be performed in patients with a clear history of reactivity or a severe reaction. A general approach to the diagnosis of food allergy is shown in Table 3.
| I. Obtain a detailed history and perform a complete physical examination | |||||
| A. Formulate suspicion of food allergy based on history and physical findings | |||||
| B. Rule out other causes of symptoms | |||||
| II. Evaluate for IgE-mediated food allergy with skin prick-puncture tests or radioallergosorbent tests | |||||
| A. Test are negative | |||||
| 1. Reintroduce the food to the diet | |||||
| 2. If the patient has a history of significant reaction or a non–IgE-mediated reaction is suspected, reintroduce the food to the diet in a physician-supervised or challenge setting | |||||
| B. Tests are positive | |||||
| 1. Eliminate food | |||||
| 2. If the patient has multiple sensitivities or an unclear history, perform open or single-blind food challenges | |||||
| a. If the challenge test is negative, reintroduce food | |||||
| b. If the challenge test is positive, challenge | |||||
| (1) Eliminate foods (if only a few foods) | |||||
| (2) If multiple foods are implicated, consider double-blind, placebo-controlled food challenges | |||||
| (a) If the challenge is positive, eliminate food | |||||
| (b) If the challenge is negative, reintroduce food | |||||
| III. Diagnosis established | |||||
| A. Educate patient about treatment and avoidance | |||||
| B. Re-evaluate at appropriate intervals if tolerance is likely | |||||
CHALLENGES IN NON–IGE-MEDIATED ALLERGY
It is more difficult to diagnose non–IgE-mediated reactions (e.g., allergic eosinophilic gastroenteritis, enterocolitis) and to pinpoint specific causative foods because no specific laboratory tests are used to identify these illnesses. In some situations (e.g., allergic eosinophilic gastroenteritis), a biopsy may be required to establish the diagnosis. Elimination diets with gradual reintroduction of foods and supervised oral food challenges are often necessary to identify the causal foods. Care must be taken because symptoms from, for example, enterocolitis syndrome, can be severe and even shock can ensue.13
Another diagnostic difficulty occurs when food additives (coloring and flavoring agents and preservatives) are implicated in reactions. Certain additives have been documented to cause the same types of reactions as those caused by IgE-mediated responses (i.e., asthma, urticaria, atopic dermatitis) but with a much lower prevalence.36,37 Because these reactions generally are not mediated by IgE, diagnosis requires trials of food elimination and oral challenge tests.
Treatment
In addition to medical management of the manifestations of food allergy (e.g., topical therapy for atopic dermatitis, inhaled medication for asthma), food allergy is treated by dietary elimination of the offending food(s). Immunotherapy (“allergy shots”) has not proved practical,38 except when pollens are responsible for the symptoms of oral allergy syndrome.39
The elimination of food proteins is a difficult task. In a milk-free diet, for example, patients must be instructed not only to avoid all obvious milk products but also to read food product ingredient labels for key words that may indicate the presence of cow's-milk protein, including “casein,” “whey,” “lactalbumin,” “caramel color” and “nougat.” When vague terms such as “high protein flavor” or “natural flavorings” are used, it may be necessary to call the manufacturer to determine if the offending protein, such as milk protein, is an ingredient.
Patients and parents must also be made aware that the food protein, as opposed to sugar or fat, is the ingredient being eliminated. For example, lactose-free milk contains cow's milk-protein, and many egg substitutes contain chicken-egg proteins. Conversely, peanut oil and soy oil generally do not contain the food protein unless the processing method is one in which the protein is not completely eliminated (as with cold-pressed or “extruded” oil).
Elimination of a particular food can be tricky. For example, a spatula used to serve cookies both with and without peanut butter can contaminate the peanut-free cookie with enough protein to cause a reaction. Similarly, contamination can occur when chocolate candies without peanuts are processed on the same equipment used for making peanut-containing candy. Hidden ingredients can also cause a problem. For example, egg white may be used to glaze pretzels, or peanut butter may be used to seal the ends of egg rolls.
The Food Allergy Network (telephone: 1-800-929-4040) is a lay organization that provides educational materials to assist families, physicians and schools in the difficult task of eliminating allergenic foods and in approaching the treatment of accidental ingestions. When multiple foods are eliminated from the diet, it is prudent to enlist the aid of a dietitian in formulating a nutritionally balanced diet.
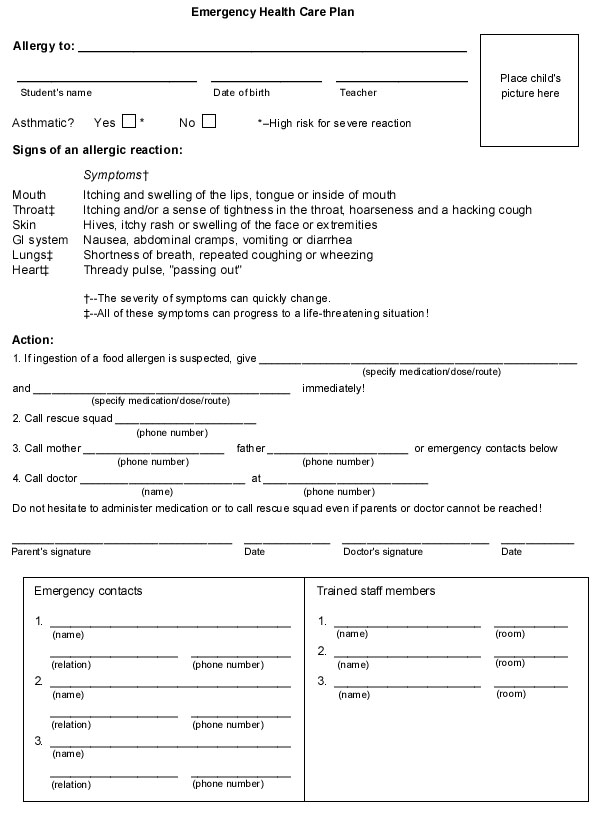
In addition to eliminating the offending food, an emergency plan must be in place for the treatment of reactions caused by accidental ingestion (Figure 1). Injectable epinephrine and an oral antihistamine should always be readily available to treat patients at risk for severe reactions. Prompt administration of epinephrine at the first signs of a severe reaction must be emphasized because delayed administration has reportedly been associated with fatal and near-fatal food allergic reactions.23 Caregivers must be taught the indications for the use and administration of epinephrine and antihistamine medications.
Final Comment
Fortunately, young children often lose their sensitivity to most of the common allergenic foods (egg, milk, wheat, soy) in a few years, particularly with avoidance of the foods.40 However, positive skin tests may persist despite the development of clinical tolerance. Serial diagnostic food challenges over time are often helpful in managing these food-allergic children. Unfortunately, sensitivity to certain foods, such as peanuts, tree nuts, fish and shellfish, is rarely lost, and sensitivity persists into adulthood.