
Am Fam Physician. 1999;59(4):817-824
Testicular torsion must be considered in any patient who complains of acute scrotal pain and swelling. Torsion of the testis is a surgical emergency because the likelihood of testicular salvage decreases as the duration of torsion increases. Conditions that may mimic testicular torsion, such as torsion of a testicular appendage, epididymitis, trauma, hernia, hydrocele, varicocele and Schönlein-Henoch purpura, generally do not require immediate surgical intervention. The cause of an acute scrotum can usually be established based on a careful history, a thorough physical examination and appropriate diagnostic tests. The onset, character and severity of symptoms must be determined. The physical examination should include inspection and palpation of the abdomen, testis, epididymis, scrotum and inguinal region. Urinalysis should always be performed, but scrotal imaging is necessary only when the diagnosis remains unclear. Once the correct diagnosis is established, treatment is usually straightforward.
Testicular pain or swelling, often referred to as the acute scrotum, can have a number of causes. Testicular torsion represents a surgical emergency because the likelihood of testicular salvage diminishes with the duration of torsion. Therefore, the family physician must act quickly to identify or exclude this condition in any patient who presents with an acute scrotum. This article reviews an approach to the diagnosis and treatment of the acute scrotum (Figure 1).
History
The history and physical examination can significantly narrow the differential diagnosis of an acute scrotum, if not establish the exact cause. None of the conditions responsible for acute scrotal pain or swelling has a single pathognomonic finding, but the combined background information and physical findings frequently suggest the correct diagnosis (Table 1).
| Condition | Onset of symptoms | Age | Tenderness | Urinalysis | Cremasteric reflex | Treatment |
|---|---|---|---|---|---|---|
| Testicular torsion | Acute | Early puberty | Diffuse | Negative | Negative | Surgical exploration |
| Appendiceal torsion | Subacute | Prepubertal | Localized to upper pole | Negative | Positive | Bed rest and scrotal elevation |
| Epididymitis | Insidious | Adolescence | Epididymal | Positive or negative | Positive | Antibiotics |
The age of the patient is important. Testicular torsion is most common in neonates and postpubertal boys, although it can occur in males of any age. Schönlein-Henoch purpura and torsion of a testicular appendage typically occur in prepubertal boys, whereas epididymitis most often develops in postpubertal boys.
The onset and duration of pain must be carefully determined. Testicular torsion usually begins abruptly, as if a switch has been flipped. The pain is severe, and the patient often appears uncomfortable. Moderate pain developing gradually over a few days is more suggestive of epididymitis or appendiceal torsion. With either of these conditions, the patient may appear relatively comfortable except when examined.
The physician needs to be aware that an embarrassed child may state that he has lower abdominal or inguinal pain rather than scrotal pain. A child may also minimize his symptoms out of fear. Therefore, the history should be corroborated with the parents' observation of the child's behavior.
A history of trauma does not exclude the diagnosis of testicular torsion. Scrotal trauma incurred during sports activities or rough, boisterous play often causes severe pain of short duration. Pain that persists for more than one hour after scrotal trauma is not normal and merits investigation to rule out testicular rupture or acute torsion. Pain that resolves promptly after scrotal trauma only to recur gradually a few days later suggests traumatic epididymitis.
Information should always be obtained about prior occurrence of pain. When asked, many patients with torsion describe previous episodes of similar pain that lasted only a short time and resolved spontaneously. Acute on-and-off pain suggests intermittent torsion with spontaneous detorsion.
Finally, a general urologic and surgical history should be obtained. Neurologic problems, congenital genitourinary anomalies and urethral instrumentation can predispose patients to urinary tract infections and thus epididymitis.
Physical Examination
The physician can often assess the severity of pain by observing the patient before beginning the physical examination. Is the patient writhing in pain or lying comfortably? Does he talk with friends or family? Is he able to ambulate without discomfort?
A general abdominal examination should be performed, with particular attention given to flank tenderness and bladder distention. Next the inguinal regions should be examined for obvious hernias and any swelling or erythema. The spermatic cord in the groin may be tender in a patient with epididymitis but typically is not tender in a patient with testicular torsion.
The genital examination begins with inspection of the scrotum. The two sides should be assessed for discrepancies in size, degree of swelling, presence and location of erythema, thickening of the skin and position of the testis. Unilateral swelling without skin changes suggests the presence of a hernia or hydrocele.
The duration of symptoms is also relevant. A high-riding testis with an abnormal (transverse) lie may suggest torsion, but this diagnosis is unlikely if pain has been present for over 12 hours and the scrotum has a normal appearance. In both epididymitis and testicular torsion, the affected hemiscrotum typically displays significant erythema and swelling after 24 hours.
The cremasteric reflex should always be assessed. This reflex is elicited by stroking or gently pinching the skin of the upper inner thigh while observing the scrotum. A normal response is contraction of the cremasteric muscles on the ipsilateral side with unilateral elevation of the testis. One study1 found that the cremasteric reflex was intact in 100 percent of boys 30 months to 12 years of age but was not consistently normal in infants and teenagers. The cremasteric reflex is rarely intact in patients with testicular torsion but is usually present in patients with torsion of a testicular appendix.2
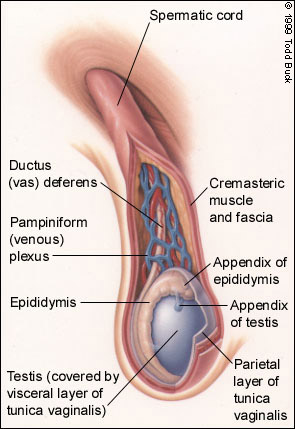
A thorough testicular examination requires a knowledge of testicular landmarks. An illustration of normal anatomy of the testis is presented in Figure 2. The testis is best examined by grasping it between the thumb and the first two digits. The epididymis should be palpable as a soft, smooth ridge posterolateral to the testis. The testes are normally the same size.
In early torsion, the entire testis is swollen and tender, and is larger than the unaffected testis (Figure 3). Tenderness limited to the upper pole suggests torsion of a testicular appendage, especially when a hard, tender nodule is palpable in this region. A small bluish discoloration, known as the “blue dot sign,” may be visible through the skin in the upper pole. This sign is virtually pathognomonic for appendiceal torsion when tenderness is also present.
In early epididymitis, the epididymis exhibits tenderness and induration, but the testis itself is not tender. Swelling to the degree that the epididymis is no longer palpable can indicate torsion if the symptoms have been present for only a few hours. With both appendiceal torsion and epididymitis, loss of testicular landmarks occurs later in the clinical course.
The testis may be elevated to elicit Prehn's sign. Lack of pain relief (negative sign) may contribute to the diagnosis of testicular torsion.
If torsion is suspected, manual detorsion can be attempted by rotating the testis away from the midline. Dramatic resolution of pain as a result of this maneuver confirms the diagnosis of torsion and eliminates the need for urgent surgical exploration. However, the patient should still be referred for elective orchiopexy.
Diagnostic Studies
Urinalysis should be performed to rule out urinary tract infection in any patient with an acute scrotum. Pyuria with or without bacteria suggests infection and is consistent with epididymitis. Based on our experience, a white blood cell count is not helpful and should not be routinely obtained.
Until recently, no imaging studies were useful in confirming the cause of an acute scrotum. Immediate surgical exploration was thus the standard approach when torsion was suspected. However, studies3–5 conducted in the past few years have shown that only 16 to 42 percent of boys with an acute scrotum have testicular torsion.
In an effort to improve diagnostic accuracy and avoid needless surgery, both nuclear medicine imaging and sonography have been performed in patients with an acute scrotum. Unfortunately, Doppler stethoscopes and conventional gray-scale ultrasonography have not been useful and therefore should not be used.6 Nuclear testicular flow studies can be helpful; however, they often require too much time and thus have fallen into disfavor.
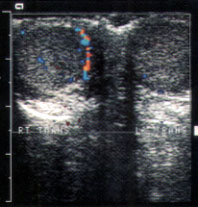
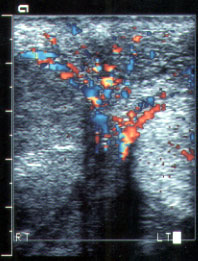

Color Doppler ultrasonography is noninvasive and has a diagnostic accuracy at least equal to that of nuclear scanning. It can semi quantitatively characterize blood flow, and it can distinguish intratesticular and scrotal wall flow.7–9 It can also be used to assess other pathologic conditions involving the scrotum.
Proper technique is essential. When color Doppler examinations are not performed correctly, studies can be false positive or false negative. The color Doppler equipment should be calibrated to demonstrate blood flow in the normal testis first. Then the abnormal testis should be examined without altering the settings on the machine. For flow measurements, the Doppler cursor must be be positioned within the testis. When normal or increased flow is demonstrated, torsion is excluded.
We recommend surgical exploration when a technically adequate color Doppler ultrasonogram cannot be obtained or when blood flow to the testis is found to be diminished or absent.10 It may not be possible to demonstrate a Doppler signal in the small testes of some young boys. In this situation, the clinical findings alone are used in deciding whether surgical exploration is required.
We recently reviewed a series of 243 boys who presented to our institution with an acute scrotum. Immediate surgical exploration was performed in 14 patients, and screening ultrasound examination was used in 229 patients. The overall incidence of testicular torsion was 19 percent. On color Doppler examination, blood flow was absent in 45 patients. Surgical exploration confirmed testicular torsion in these patients. One of the two patients with decreased blood flow had testicular torsion; the other had torsion of the appendix testis. The color Doppler examination showed increased or normal blood flow in 182 patients. None of these patients later developed testicular atrophy, which would have indicated misdiagnosed torsion. Color Doppler ultrasonography also correctly diagnosed incarcerated hernias, varicoceles, hematomas and testicular ruptures.
Treatment
SPERMATIC CORD TORSION
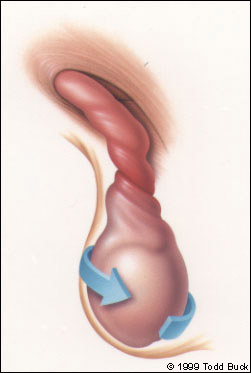
The “bell clapper” deformity is one underlying cause of testicular torsion in older children. In this deformity, the testicle lacks a normal attachment to the tunica vaginalis and therefore hangs freely. As a result, the spermatic cord can twist within the tunica vaginalis (intravaginal torsion).
When the history and physical examination strongly suggest that testicular torsion is present and the duration of pain is less than 12 hours, urgent surgical intervention is indicated. No imaging studies are required because they may delay treatment and thereby jeopardize testicular survival. When pain has been present for more than 12 hours or the diagnosis is unclear, color Doppler ultrasound examination can be helpful in making clinical decisions. It is important to remember that most patients with an acute scrotum do not have testicular torsion.
Surgery is performed to correct torsion in the affected testis and to anchor the other testis (orchiopexy) to prevent future torsion, which otherwise occurs in most patients with contralateral torsion. Surgical exploration can usually be accomplished through a single, small midline incision in the scrotal raphe. Clearly necrotic testes must be removed. Viable testes should be fixed with nonabsorbable sutures.
Testicular torsion can also occur perinatally if the entire testis complex has not yet fused to the scrotum. In this type of torsion, the testis, spermatic cord and tunica vaginalis twist en bloc (extravaginal torsion). Clinically, extra-vaginal torsion appears as an asymptomatic swelling of the scrotum. Erythema or a bluish discoloration of the scrotum is also frequently seen.
The management of perinatal torsion remains controversial. Some surgeons advocate a nonoperative approach because of the poor potential for testicular salvage. Others, ourselves included, argue that leaving a neonatal testis in place may have adverse effects on the contralateral testis and note that cases of bilateral neonatal torsion have been reported.11 However, we do not perform surgery urgently unless the neonate has clear documentation of a normal examination at birth and subsequently experiences testicular torsion.
TORSION OF TESTICULAR APPENDAGES
The appendix testis, a müllerian duct remnant located at the superior pole of the testicle, is the most common appendage to undergo torsion. The epididymal appendix, located on the head of the epididymis, is a wolffian duct remnant and may also become twisted. Torsion of either appendage produces pain similar to that experienced with testicular torsion, but the onset is more gradual. Color Doppler ultrasonography demonstrates increased blood flow.
Torsion of a testicular appendage may be misinterpreted as epididymitis. However if the urinalysis is normal, no antibiotic therapy is required. Management entails several days of bed rest and scrotal elevation in an effort to minimize inflammation and edema. Normal activity may both worsen and prolong the symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) and analgesics generally are not helpful and thus are not routinely used. The inflammation usually resolves within a week, although the testicular examination may not be completely normal for several weeks.
EPIDIDYMITIS OR ORCHITIS
Epididymitis in adolescents and young adults is often related to sexual activity and does not present with a urinary tract infection. In prepubertal boys, however, epididymitis is almost always associated with a urinary tract anomaly.12 Any episode of epididymitis and urinary tract infection should be investigated with a renal/bladder sonogram and a voiding cystourethrogram to rule out structural problems.
Treatment includes empiric antibiotic therapy until the results of a urine culture are known. If the culture is negative, the symptoms are most likely due to abacterial epididymitis caused by urine reflux. Bed rest and scrotal elevation are often helpful. NSAIDs and analgesics can be used to alleviate symptoms. As with appendiceal torsion, the pain and swelling generally resolve within a week. Resolution of epididymal induration may require several weeks.
SCROTAL TRAUMA
Severe testicular injury is uncommon and usually results from either a direct blow to the scrotum or a straddle injury. Damage occurs when the testis is forcefully compressed against the pubic bones. A spectrum of injuries may occur.
Traumatic epididymitis is a noninfectious inflammatory condition that usually occurs within a few days after a blow to the testis. Treatment is similar to that for nontraumatic epididymitis.
Scrotal trauma can also result in intratesticular hematoma, hematocele or laceration of the tunica albuginea (testicular rupture). Color Doppler ultrasonography is the imaging technique of choice.13 Surgical referral is required because testicular rupture requires immediate drainage and repair. Hematomas and hematoceles are managed on an individual basis.
OTHER CAUSES
Acute idiopathic scrotal edema is another possible cause of an acute scrotum. This condition is characterized by the rapid onset of significant edema without tenderness. Erythema may be present. The patient is usually afebrile, and all diagnostic tests are negative. The etiology of this condition remains unclear. Treatment consists of bed rest and scrotal elevation. Analgesics are rarely needed.
Schönlein-Henoch purpura, a systemic vasculitic syndrome of uncertain etiology, is characterized by nonthrombocytopenic purpura, arthralgia, renal disease, abdominal pain, gastrointestinal bleeding and, occasionally, scrotal pain.14 The onset can be acute or insidious. Hematuria may be present. The syndrome has no specific treatment.
Inguinal hernia should be suspected in a child who has a history of intermittent groin swelling. If the diagnosis is unclear, ultrasound examination can be helpful. An incarcerated or strangulated hernia requires urgent surgical intervention, whereas a reducible hernia should be repaired electively.
A hydrocele occurs because of a patent processus vaginalis. The hydrocele can seal off, trapping peritoneal fluid around the testis, or it can persist and dilate, possibly causing bowel herniation. Most hydroceles resolve spontaneously. Therefore, an infant with a hydrocele and no evidence of a hernia is usually just observed for the first one or two years of life. If the hydrocele persists beyond this time, surgical repair through the groin is recommended.
Occasionally, a varicocele causes mild to moderate scrotal discomfort. No changes in the scrotal skin occur, but the affected hemi-scrotum may have a full appearance. On physical examination, a varix is palpable as a “bag of worms” above a palpably normal testis and epididymis. Referral to a urologist is prudent because varicoceles can affect both testicular growth and fertility.15