
Am Fam Physician. 1999;60(7):2027-2034
Appendicitis is common, with a lifetime occurrence of 7 percent. Abdominal pain and anorexia are the predominant symptoms. The most important physical examination finding is right lower quadrant tenderness to palpation. A complete blood count and urinalysis are sometimes helpful in determining the diagnosis and supporting the presence or absence of appendicitis, while appendiceal computed tomographic scans and ultrasonography can be helpful in equivocal cases. Delay in diagnosing appendicitis increases the risk of perforation and complications. Complication and mortality rates are much higher in children and the elderly.
Despite technologic advances, the diagnosis of appendicitis is still based primarily on the patient's history and the physical examination. Prompt diagnosis and surgical referral may reduce the risk of perforation and prevent complications.4 The mortality rate in nonperforated appendicitis is less than 1 percent, but it may be as high as 5 percent or more in young and elderly patients, in whom diagnosis may often be delayed, thus making perforation more likely.1
Pathogenesis
The appendix is a long diverticulum that extends from the inferior tip of the cecum.5 Its lining is interspersed with lymphoid follicles.3 Most of the time, the appendix has an intraperitoneal location (either anterior or retrocecal) and, thus, may come in contact with the anterior parietal peritoneum when it is inflamed. Up to 30 percent of the time, the appendix may be “hidden” from the anterior peritoneum by being in a pelvic, retroileal or retrocolic (retroperitoneal retrocecal) position.6 The “hidden” position of the appendix notably changes the clinical manifestations of appendicitis.
Obstruction of the narrow appendiceal lumen initiates the clinical illness of acute appendicitis. Obstruction has multiple causes, including lymphoid hyperplasia (related to viral illnesses, including upper respiratory infection, mononucleosis, gastroenteritis), fecaliths, parasites, foreign bodies, Crohn's disease, primary or metastatic cancer and carcinoid syndrome. Lymphoid hyperplasia is more common in children and young adults, accounting for the increased incidence of appendicitis in these age groups.1,5
History and Physical Examination
Abdominal pain is the most common symptom of appendicitis.3 In multiple studies,3–5 specific characteristics of the abdominal pain and other associated symptoms have proved to be reliable indicators of acute appendicitis (Table 1). A thorough review of the history of the abdominal pain and of the patient's recent genitourinary, gynecologic and pulmonary history should be obtained.
| Common symptoms* | Frequency (%) |
|---|---|
| Abdominal pain | ~100 |
| Anorexia | ~100 |
| Nausea | 90 |
| Vomiting | 75 |
| Pain migration | 50 |
| Classic symptom sequence (vague periumbilical pain to anorexia/nausea/unsustained vomiting to migration of pain to right lower quadrant to low-grade fever) | 50 |
Anorexia, nausea and vomiting are symptoms that are commonly associated with acute appendicitis. The classic history of pain beginning in the periumbilical region and migrating to the right lower quadrant occurs in only 50 percent of patients.1 Duration of symptoms exceeding 24 to 36 hours is uncommon in nonperforated appendicitis.1
In a recent meta-analysis,7 likelihood ratios were calculated for many of these symptoms (Table 2). A likelihood ratio is the amount by which the odds of a disease change with new information (e.g., physical examination findings, laboratory results).8 This change can be positive or negative. Symptoms such as anorexia, nausea and vomiting commonly occur in acute appendicitis; however, the presence of these symptoms does not necessarily increase the likelihood of appendicitis nor does their absence decrease the likelihood of the diagnosis. Moreover, other symptoms have more notable positive and negative likelihood ratios (Table 2).
| Symptom/sign | Positive likelihood ratio (LR+) |
|---|---|
| Right lower quadrant (RLQ) pain | 8.0 |
| Pain migration | 3.2 |
| Pain before vomiting | 2.8 |
| Anorexia, nausea and vomiting* | Much lower LR+ than RLQ pain, pain migration and pain before vomiting |
| Psoas sign | 2.38 |
| Rebound tenderness | 1.1 to 6.3† |
| Fever | 1.9‡ |
| Guarding and rectal tenderness* | Much lower LR+ than rigidity, psoas sign and rebound tenderness |
| Symptom/sign | Negative likelihood ratio (LR−) |
| RLQ pain§ | 0 to 0.28† |
| No similar pain previously∥ | 0.3 |
| Pain migration | 0.5 |
| Guarding | 0 to 0.54† |
| Rebound tenderness | 0 to 0.86† |
| Fever, rigidity and psoas sign¶ | |
| note: LR is the amount by which the odds of a disease change with new information, as follows: | |
A careful, systematic examination of the abdomen is essential. While right lower quadrant tenderness to palpation is the most important physical examination finding, other signs may help confirm the diagnosis (Table 3). The abdominal examination should begin with inspection followed by auscultation, gentle palpation (beginning at a site distant from the pain) and, finally, abdominal percussion. The rebound tenderness that is associated with peritoneal irritation has been shown to be more accurately identified by percussion of the abdomen than by palpation with quick release.1
| Right lower quadrant pain on palpation (the single most important sign) | |
| Low-grade fever (38°C [or 100.4°F])—absence of fever or high fever can occur | |
| Peritoneal signs | |
| Localized tenderness to percussion | |
| Guarding | |
| Other confirmatory peritoneal signs (absence of these signs does not exclude appendicitis) | |
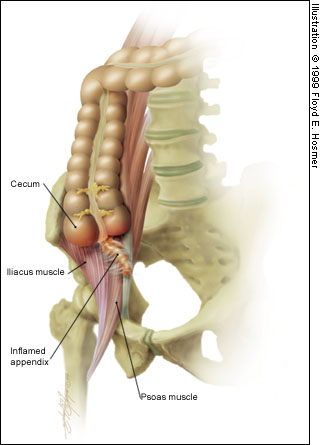
| Psoas sign—pain on extension of right thigh (retroperitoneal retrocecal appendix) | |
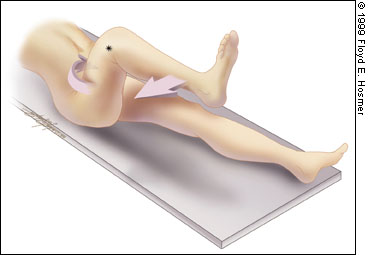
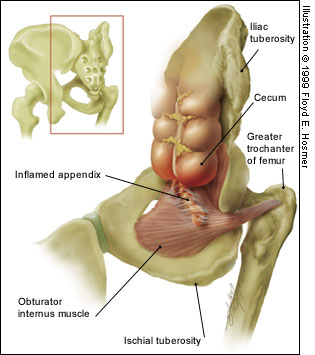
| Obturator sign—pain on internal rotation of right thigh (pelvic appendix) | |
| Rovsing's sign—pain in right lower quadrant with palpation of left lower quadrant | |
| Dunphy's sign—increased pain with coughing | |
| Flank tenderness in right lower quadrant (retroperitoneal retrocecal appendix) | |
| Patient maintains hip flexion with knees drawn up for comfort | |
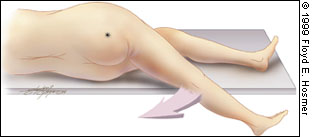
As previously noted, the location of the appendix varies. When the appendix is hidden from the anterior peritoneum, the usual symptoms and signs of acute appendicitis may not be present. Pain and tenderness can occur in a location other than the right lower quadrant.6 A retrocecal appendix in a retroperitoneal location may cause flank pain. In this case, stretching the iliopsoas muscle can elicit pain. The psoas sign is elicited in this manner: the patient lies on the left side while the examiner extends the patient's right thigh (Figures 1a and 1b). In contrast, a patient with a pelvic appendix may show no abdominal signs, but the rectal examination may elicit tenderness in the cul-de-sac. In addition, an obturator sign (pain on passive internal rotation of the flexed right thigh) may be present in a patient with a pelvic appendix3 (Figures 2a and 2b).
The differential diagnosis of appendicitis is broad, but the patient's history and the remainder of the physical examination may clarify the diagnosis (Table 4). Because many gynecologic conditions can mimic appendicitis, a pelvic examination should be performed on all women with abdominal pain. Given the breadth of the differential diagnosis, the pulmonary, genitourinary and rectal examinations are equally important. Studies have shown, however, that the rectal examination provides useful information only when the diagnosis is unclear and, thus, can be reserved for use in such cases.5
Laboratory and Radiologic Evaluation
If the patient's history and the physical examination do not clarify the diagnosis, laboratory and radiologic evaluations may be helpful. A clear diagnosis of appendicitis obviates the need for further testing and should prompt immediate surgical referral.
LABORATORY TESTS
The white blood cell (WBC) count is elevated (greater than 10,000 per mm3 [100 × 109 per L]) in 80 percent of all cases of acute appendicitis.9 Unfortunately, the WBC is elevated in up to 70 percent of patients with other causes of right lower quadrant pain.10 Thus, an elevated WBC has a low predictive value. Serial WBC measurements (over 4 to 8 hours) in suspected cases may increase the specificity, as the WBC count often increases in acute appendicitis (except in cases of perforation, in which it may initially fall).5
In addition, 95 percent of patients have neutrophilia1 and, in the elderly, an elevated band count greater than 6 percent has been shown to have a high predictive value for appendicitis.9 In general, however, the WBC count and differential are only moderately helpful in confirming the diagnosis of appendicitis because of their low specificities.
A more recently suggested laboratory evaluation is determination of the C-reactive protein level. An elevated C-reactive protein level (greater than 0.8 mg per dL) is common in appendicitis, but studies disagree on its sensitivity and specificity.4,5 An elevated C-reactive protein level in combination with an elevated WBC count and neutrophilia are highly sensitive (97 to 100 percent). Therefore, if all three of these findings are absent, the chance of appendicitis is low.5
In patients with appendicitis, a urinalysis may demonstrate changes such as mild pyuria, proteinuria and hematuria,1 but the test serves more to exclude urinary tract causes of abdominal pain than to diagnose appendicitis.
RADIOLOGIC EVALUATION
The options for radiologic evaluation of patients with suspected appendicitis have expanded in recent years, enhancing and sometimes replacing previously used radiologic studies.
Plain radiographs, while often revealing abnormalities in acute appendicitis, lack specificity and are more helpful in diagnosing other causes of abdominal pain. Likewise, barium enema is now used infrequently because of the advances in abdominal imaging.5
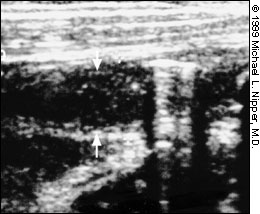
Ultrasonography and computed tomographic (CT) scans are helpful in evaluating patients with suspected appendicitis.11 Ultrasonography is appropriate in patients in which the diagnosis is equivocal by history and physical examination. It is especially well suited in evaluating right lower quadrant or pelvic pain in pediatric and female patients. A normal appendix (6 mm or less in diameter) must be identified to rule out appendicitis. An inflamed appendix usually measures greater than 6 mm in diameter (Figure 3), is noncompressible and tender with focal compression. Other right lower quadrant conditions such as inflammatory bowel disease, cecal diverticulitis, Meckel's diverticulum, endometriosis and pelvic inflammatory disease can cause false-positive ultrasonography results.12
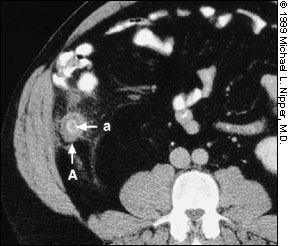
CT, specifically the technique of appendiceal CT, is more accurate than ultrasonography (Table 5). Appendiceal CT consists of a focused, helical, appendiceal CT after a Gastrografin-saline enema (with or without oral contrast) and can be performed and interpreted within one hour. Intravenous contrast is unnecessary.12 The accuracy of CT is due in part to its ability to identify a normal appendix better than ultrasonography.13 An inflamed appendix is greater than 6 mm in diameter, but the CT also demonstrates periappendiceal inflammatory changes14 (Figures 4 and 5). If appendiceal CT is not available, standard abdominal/pelvic CT with contrast remains highly useful and may be more accurate than ultrasonography.12
| Comparison graded ultrasound | Appendiceal computed tomographic scan | |
|---|---|---|
| Sensitivity | 85% | 90 to 100% |
| Specificity | 92% | 95 to 97% |
| Use | Evaluate patients with equivocal diagnosis of appendicitis | Evaluate patients with equivocal diagnosis of appendicitis |
| Advantages | Safe | More accurate |
| Relatively inexpensive | Better identifies phlegmon and abscess | |
| Can rule out pelvic disease in females | Better identifies normal appendix | |
| Better for children | ||
| Disadvantages | Operator dependent | Cost |
| Technically inadequate studies due to gas | Ionizing radiation | |
| Pain | Contrast |

Treatment
The standard for management of nonperforated appendicitis remains appendectomy. Because prompt treatment of appendicitis is important in preventing further morbidity and mortality, a margin of error in over-diagnosis is acceptable. Currently, the national rate of negative appendectomies is approximately 20 percent.15 Some studies have investigated nonoperative management with parenteral antibiotic treatment, but 40 percent of these patients eventually required appendectomy.3
Appendectomy may be performed by laparotomy (usually through a limited right lower quadrant incision) or laparoscopy. Diagnostic laparoscopy may be helpful in equivocal cases or in women of childbearing age, while therapeutic laparoscopy may be preferred in certain subsets of patients (e.g., women, obese patients, athletes).16
While laparoscopic intervention has the advantages of decreased postoperative pain, earlier return to normal activity and better cosmetic results, its disadvantages include greater cost and longer operative time.4 Open appendectomy may remain the primary approach to treatment until further cost and benefit analyses are conducted.
Complications
Appendiceal rupture accounts for a majority of the complications of appendicitis. Factors that increase the rate of perforation are delayed presentation to medical care,17 age extremes (young and old)18 and hidden location of appendix.6 A brief period of in-hospital observation (less than six hours) in equivocal cases does not increase the perforation rate and may improve diagnostic accuracy.18
Diagnosis of a perforated appendix is usually easier (although immediately after rupture, the patient's symptoms may temporarily subside). The physical examination findings are more obvious if peritonitis generalizes, with a more generalized right lower quadrant tenderness progressing to complete abdominal tenderness. An ill-defined mass may be felt in the right lower quadrant. Fever is more common with rupture, and the WBC count may elevate to 20,000 to 30,000 per mm3 (200 to 300 × 109 per L) with a prominent left shift.3
Special Considerations
While appendicitis is uncommon in young children, it poses special difficulties in this age group. Young children are unable to relate a history, often have abdominal pain from other causes and may have more nonspecific signs and symptoms. These factors contribute to a perforation rate as high as 50 percent in this group.1
In pregnancy, the location of the appendix begins to shift significantly by the fourth to fifth months of gestation. Common symptoms of pregnancy may mimic appendicitis, and the leukocytosis of pregnancy renders the WBC count less useful. While the maternal mortality rate is low, the overall fetal mortality rate is 2 to 8.5 percent, rising to as high as 35 percent in perforation with generalized peritonitis. As in nonpregnant patients, appendectomy is the standard for treatment.3
Elderly patients have the highest mortality rates. The usual signs and symptoms of appendicitis may be diminished, atypical or absent in the elderly, which leads to a higher rate of perforation. More frequent perforation combined with a higher incidence of other medical problems and less reserve to fight infection contribute to a mortality rate of up to 5 percent or more.1
Final Comment
Prompt diagnosis of appendicitis ensures timely treatment and prevents complications. Because abdominal pain is a common presenting symptom in outpatient care, family physicians serve an important role in the diagnosis of appendicitis. Obvious cases of appendicitis require urgent referral, while equivocal cases warrant further evaluation and, many times, surgical consultation.