
Am Fam Physician. 2000;61(3):691-700
The evaluation of elbow pain can be challenging because of the complexity of the joint and its central location in the upper extremity. Diagnosing the injury correctly requires an understanding of the anatomy of the elbow, which includes three articulations, two ligament complexes, four muscle groups and three major nerves. The history should be directed at pinpointing the location of symptoms and the activities that cause the patient's pain. It is important to identify the specific musculotendinous structures that are at risk for overuse or have been injured through overuse. Mechanical symptoms are indicative of intra-articular pathology, whereas neurologic symptoms are characteristic of nerve entrapment syndromes. Physical examination of the elbow and related structures should confirm the diagnosis. Only a minority of patients require diagnostic studies. Basic treatment principles are described by the acronym PRICEMM: protection, rest, ice, compression, elevation, medication and modalities (physical therapy). Surgical consultation is warranted in selected patients.
Family physicians frequently encounter overuse injuries involving the elbow. The spectrum of injuries involving the elbow is well described in athletes, and such injuries are becoming increasingly common in occupational areas.
Patient complaints about elbow pain can be vexing because the intricate anatomy of the upper extremity provides a myriad of potential sources of dysfunction. A knowledge of the anatomy of the elbow can help the family physician construct a differential diagnosis. Armed with this knowledge, along with good history-taking and physical examination skills, the physician can correctly identify common overuse injuries.
Anatomy of the Elbow
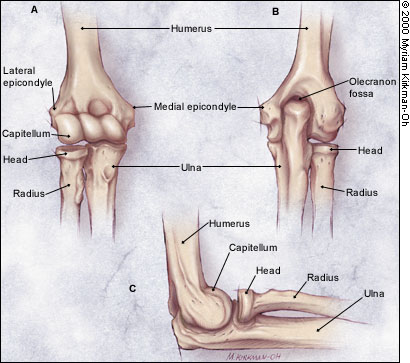
The elbow contains three separate articulations. The humeroulnar joint is a modified hinge joint that allows flexion and extension. The humeroradial joint is a combined hinge and pivot joint that permits flexion and extension as well as rotation of the head of the radius on the capitellum of the humerus. The proximal radioulnar joint facilitates rotation during supination and pronation. The bones that comprise the elbow joints are shown in Figure 1.
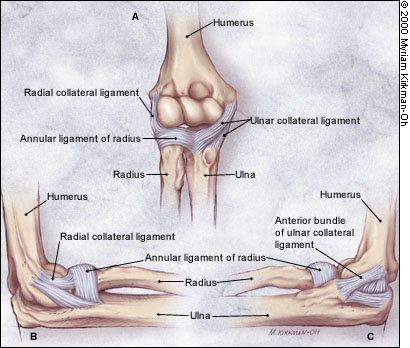
Osseous stability is reinforced by the medial and lateral ligament complexes (Figure 2). The medial ligament complex, or ulnar collateral ligament complex, provides valgus stability. The medial complex has anterior, posterior and transverse bundles. The anterior bundle provides the greatest stability.1,2 The lateral ligament complex provides rotational and varus stability. The annular ligament encircles the head of the radius, stabilizing it in the radial notch. The radial collateral ligament provides varus stability. The accessory lateral collateral ligament assists the annular ligament during varus stress, and the lateral ulnar collateral ligament provides inferior rotatory stability for the humeroulnar joint.
Four muscle groups act on the elbow. Major flexors include the biceps brachii (which also supinates the forearm when the elbow is flexed), brachioradialis and brachialis muscles. The extensors are the triceps and anconeus muscles. The supinators include the supinator and biceps brachii muscles. Pronation is accomplished by the pronator quadratus, pronator teres and flexor carpi radialis muscles.
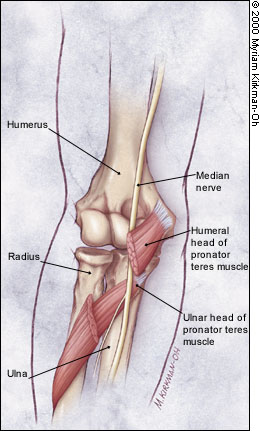
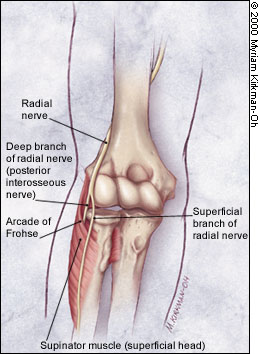
The elbow also has complex innervation. The median nerve crosses the elbow medially and passes through the two heads of the pronator teres, a potential site of entrapment3 (Figure 3). The ulnar nerve passes along the medial arm and posterior to the medial epicondyle through the cubital tunnel, a likely site of compression4 (Figure 4). The radial nerve descends the arm laterally. It divides into the superficial (sensory) branch and the deep (motor, or posterior interosseous) branch. The deep branch must then pass through the arcade of Frohse, a fibrous arch formed by the proximal margin of the superficial head of the supinator muscle, where it is most susceptible to injury.5
History
When a patient presents with elbow pain, the family physician should seek information about occupational and recreational activities involving a repetitive load that could initiate a cycle of microtrauma, chronic inflammation, tissue degeneration, necrosis and, ultimately, tendon rupture (Table 1).
| Activity | Injuries |
|---|---|
| Bowling | Biceps tendinosis, radial tunnel syndrome |
| Boxing | Triceps tendinosis |
| Friction in football, wrestling or basketball | Olecranon bursitis |
| Golf | Golfer's elbow (trailing arm), radial tunnel syndrome |
| Gymnastics | Biceps tendinosis, triceps tendinosis |
| Posterior dislocation | Posterolateral rotatory instability |
| Racquet sports | Pronator syndrome, triceps tendinosis, olecranon stress fracture, lateral tennis elbow, radial tunnel syndrome, golfer's elbow, ulnar nerve entrapment |
| Rowing | Radial tunnel syndrome |
| Skiing | Ulnar nerve entrapment |
| Swimming | Radial tunnel syndrome |
| Throwing | Pronator syndrome, triceps tendinosis, olecranon impingement, olecranon stress fracture, radiocapitellar chondromalacia, ulnar collateral ligament sprain, golfer's elbow, ulnar nerve entrapment |
| Weight lifting | Biceps tendinosis, triceps tendinosis, anterior capsule strain, radial tunnel syndrome, ulnar nerve entrapment |
The timing of the onset of symptoms can be helpful in identifying the offending activity and thus the tissues at risk for overuse. The severity of symptoms can be judged by whether they occur only after activity, with activity or at rest. It is important to determine the location of the pain and whether the pain is radiating in character. Alleviating or aggravating factors should also be identified.
It is particularly important to identify neurologic and mechanical symptoms. Weakness or paresthesias are clues to peripheral nerve entrapment syndromes or cervical radiculopathies.4 Mechanical symptoms, such as clicking with motion, locking in extension and catching, may indicate intra-articular pathology.5
The history allows the physician to proceed with a symptom-oriented approach to the differential diagnosis (Table 2).
| Anterior elbow |
| Biceps tendinosis |
| Pronator syndrome |
| Anterior capsule strain |
| Posterior elbow |
| Triceps tendinosis |
| Olecranon impingement |
| Olecranon stress fracture |
| Olecranon bursitis |
| Lateral elbow |
| Lateral tennis elbow |
| Radial tunnel syndrome |
| Radiocapitellar chondromalacia |
| Posterolateral rotatory instability |
| Medial elbow |
| Medial tennis elbow (golfer's elbow) |
| Ulnar collateral ligament sprain |
| Ulnar nerve entrapment |
Physical Examination
A systematic evaluation of the elbow includes inspection, palpation, range of motion testing, neurologic assessment, examination of related areas and various special tests. A complete review of the elbow examination is beyond the scope of this article but is available in a number of texts.6,7 However, several special tests warrant description because they should be used routinely to assess patients for tennis elbow and ligamentous instability.
The tennis elbow test is performed with the patient's extended elbow stabilized in the physician's hand and the thumb of that hand positioned on the patient's lateral epicondyle (Figure 5). The patient makes a fist, pronates the forearm and radially deviates and extends the wrist while the physician applies a resisting force at the fist.6 The test is positive if pain is elicited in the area of the lateral epicondyle. In the patient with more advanced tennis elbow, pain is elicited when the same maneuver is performed with the elbow flexed to 90 degrees.7

Flexion force applied against long finger (third digit) extension distal to the proximal interphalangeal joint may provoke pain over the extensor muscle mass in the proximal forearm. This finding is suggestive of radial tunnel syndrome, which is often misdiagnosed as resistant lateral tennis elbow.8
Ulnar and radial ligamentous stabilities are assessed with the patient's forearm flexed at 20 degrees to unlock the olecranon from its fossa. The physician alternately applies valgus force (Figure 6) and varus force (Figure 7) to evaluate the area for medial or lateral laxity, pain, decreased mobility or apprehension (i.e., sensation of impending dislocation).


The posterolateral rotatory-instability test, or lateral pivot-shift test, assesses laxity of the ulnar part of the lateral collateral ligament.9 If present, this instability allows the humeroulnar joint to sublux, with secondary dislocation of the humeroradial joint. This test is best performed with the patient supine. The arm to be tested is extended back over the patient's head, and the shoulder is rotated externally (Figure 8). While standing at the head of the table, the physician supinates the patient's forearm and simultaneously applies valgus stress, axial compression and flexion of the elbow (Figure 9). Apprehension in the awake patient indicates a positive test. Displacement of the ulna from the trochlea, with humeroradial joint dislocation, is usually achieved only in a patient who has received general anesthesia.


The neck, shoulder and wrist should be examined carefully in the patient with elbow pain. This examination excludes elbow symptoms secondary to referred pain resulting from the body's attempts to compensate for dysfunction elsewhere (e.g., tennis elbow secondary to rotator cuff dysfunction).
Diagnostic Tests
Standard radiographs of the elbow include the straight anteroposterior view and the true lateral view. The radial head normally articulates with the capitellum, and a line bisecting the proximal radial shaft should always pass through the capitellum on any radiographic view. Special views include axial projections to evaluate the olecranon fossa, oblique views to assess the radial head and stress views to evaluate joint stability.10
Bone scanning is sensitive but not specific for detecting stress fractures, healing fractures, infections and tumors. Computed tomographic scanning is useful for delineating complex osseous anatomy. Magnetic resonance imaging (MRI) can be helpful in identifying soft tissue masses, articular cartilage anatomy, ligament ruptures and chondral defects. Arthrography may be useful for defining articular surfaces and identifying loose bodies or capsular defects.11
Electromyography and nerve conduction studies are used to evaluate suspected nerve compression syndromes. Although these studies can be helpful in confirming a diagnosis, they are somewhat insensitive.12 Thus, clinical judgment should prevail in making treatment decisions.
Elbow Disorders
ANTERIOR ELBOW DISORDERS
Biceps Tendinosis. Anterior elbow pain in a patient who has engaged in activities involving repetitive elbow flexion and forearm supination may indicate the presence of biceps tendinosis. Weak elbow flexion may be an additional complaint.
With biceps tendinosis, the physical examination reveals tenderness of the distal biceps tendon that increases with resisted flexion and supination. The patient with advanced biceps tendinosis may develop elbow flexion contractures and thus may be unable to fully extend the elbow.
The history and physical examination are usually sufficient to identify this disorder. Further testing is generally unnecessary.
Pronator Syndrome. This disorder occurs because of median nerve entrapment distal to the elbow. The pronator syndrome often occurs in patients who present with elbow pain subsequent to participation in racquet or throwing sports. Anterior pain and distal paresthesias are characteristic symptoms.
The physical examination frequently reveals a hypertrophied pronator muscle distal to the antecubital fossa, often with a positive Tinel's sign. The patient may or may not have distal numbness. The pain worsens when pronation is performed against resistance. Tingling or paresthesias in the distribution of the median nerve is a sign of pronator syndrome. The patient may also have a positive papal sign (i.e., weak active flexion of the index finger [second digit] and long finger, resulting in finger extension in the resting attitude).
Nerve conduction studies may be helpful in making the diagnosis and may also help rule out carpal tunnel syndrome. However, false-negative nerve conduction study results are possible. Radiographs are usually normal.
Anterior Capsule Strain. Activities requiring repetitive hyperextension of the elbow may strain the anterior capsule. The strain results in anterior pain that becomes worse with passive extension or hyperextension stress testing. The antecubital fossa is tender.
A possible related injury is a torn brachialis muscle with associated myositis. Therefore, radiographs should be obtained to rule out myositis ossificans.13
POSTERIOR ELBOW DISORDERS
Triceps Tendinosis. Posterior elbow pain in the setting of repetitive elbow extension suggests the diagnosis of triceps tendinosis. Forceful extension worsens the pain. Tenderness of the triceps tendon is present at or just superior to the attachment on the olecranon and increases with extension performed under resistance.
Radiographs are usually normal. If osteoarthritis is present, however, the radiographs may show calcifications within the tendon, traction spurs, hypertrophy of the ulna or loose bodies.
Olecranon Impingement. This injury, which typically occurs in throwing activities, is characterized by clicking or locking of the elbow with terminal extension. Crepitus and a mechanical extension block are often present. The elbow pain worsens with extension. Subtle valgus instability may be noted, in that ulnar collateral ligament deficiency may occur because of the repetitive valgus stress of throwing.
Radiographs may show osteophytes of the olecranon tip and the medial wall of the olecranon fossa, hypertrophy of the olecranon and loose bodies.
Olecranon Stress Fracture. This fracture produces pain that gradually increases with extension in throwing. The olecranon process is tender, and pain is increased with extension performed against resistance.
Radiographs may be negative, but two possible findings are important. First, the lesion may show a transverse radiolucency extending from the posterior nonarticular surface to the articular surface. Second, a lucent region surrounded by a sclerotic margin may indicate nonunion of a stress fracture.14 If the radiographic findings are in question, bone scanning may be required to confirm the diagnosis.
Olecranon Bursitis. Painless swelling of the posterior elbow at the outer tip of the olecranon in a patient complaining of repetitive friction to the elbow indicates olecranon bursitis. The pertinent physical findings are localized, nontender swelling without decreased range of motion.
Radiographs are usually normal. Septic arthritis should be ruled out in the patient with any associated pain or erythematous tissue.
LATERAL ELBOW DISORDERS
Lateral Tennis Elbow. The most common overuse elbow injury, lateral tennis elbow is the result of degenerative tendinosis of the extensor carpi radialis brevis muscle. The injury typically occurs because of overuse of the wrist extensors (e.g., in racquet sports).
In lateral tennis elbow, the pain is aching, worsens with activity and frequently radiates down the lateral forearm. The patient may also have night pain. Tenderness is present over the extensor carpi radialis brevis and is generally localized immediately anterior, medial and distal to the lateral epicondyle. The pain increases with resisted dorsiflexion of the wrist, especially with the elbow in extension.
The tennis elbow test reproduces the pain. Radiographs may show calcific deposits in the extensor aponeurosis or spurring but are frequently normal.
Radial Tunnel Syndrome. In this relatively uncommon disorder, compression of the deep branch of the radial nerve at the radial tunnel causes pain that radiates into the dorsal forearm. The pain increases with activities involving repetitive pronation and supination. Night pain may be present.
On physical examination, tenderness is present where the radial nerve crosses the head of the radius. The patient may or may not have finger and wrist extensor weakness. The Tinel's sign may be positive over the radial nerve distal and anterior to the lateral epicondyle. Pain on resisted supination of the extended forearm, especially with wrist flexion, is often present.
A lidocaine (Xylocaine) block can be helpful in diagnosing radial tunnel syndrome. The technique may confirm the diagnosis when 1 mL of 1 percent lidocaine injected four finger-breadths distal to the lateral epicondyle relieves pain and is accompanied by a temporary deep radial palsy and when an injection given at another time but more proximally in the region of the lateral epicondyle does not relieve the patient's symptoms.15
Radiographs are usually unremarkable, but electrodiagnostic studies may be positive. Radial tunnel syndrome should be considered in the patient with refractory tennis elbow, as the clinical presentation can be notably similar.
Radiocapitellar Chondromalacia. This condition occurs because of repetitive valgus stress. Compression of the radiocapitellar articulation sometimes results in damage to the radial head, the capitellum, or both. Frank osteochondral fracture and loose bodies may occur.
The typical presenting symptoms are catching, locking and lateral elbow pain with active use of the elbow. Swelling and localized tenderness are noted at the affected site.
An axial load applied with passive supination and pronation often provokes pain and can be helpful in differentiating radiocapitellar chondromalacia from lateral tennis elbow.12 Radiographs may show a loss of joint space, marginal osteophytes and, possibly, loose bodies.
Posterolateral Rotatory Instability. This rare complication of posterior dislocation may present with mechanical symptoms or recurrent dislocation. The lateral pivot-shift test is positive. Radiographs are typically negative.
MEDIAL ELBOW DISORDERS
Medial Tennis Elbow (Golfer's Elbow). In this condition, pain in the medial elbow and proximal forearm occurs with activities that require rapid wrist flexion (wrist snapping) and forearm pronation. The pain worsens with activity.
On physical examination, pain is present from the tip of the medial epicondyle to the pronator teres and flexor carpi radialis muscles. Pain is increased with wrist flexion and forearm supination performed under resistance.
Radiographs are usually normal but may show extra-articular calcifications.
Ulnar Collateral Ligament Sprain. This type of sprain most commonly occurs in throwing activities. The injury is characterized by the insidious onset of vague medial elbow pain that becomes worse with activity. The pain is typically relieved with rest but returns on resumption of throwing at over 70 percent of normal velocity.
An ulnar collateral ligament sprain can be demonstrated by pain or instability on valgus stress testing. Radiographs may show loose bodies, traction spurs or heterotropic ossification of the ligament itself. MRI can identify partial and complete tears, but this study is not usually necessary.
Ulnar Nerve Entrapment. The presenting symptom of ulnar nerve entrapment is medial elbow pain, but the disorder is also characterized by distal paresthesias along the ulnar aspect of the forearm and into the ring and little fingers (fourth and fifth digits). The patient may complain of a weak grip, hand fatigue and clumsiness. Ulnar nerve entrapment often occurs in throwing sports, as well as racquet sports, weight lifting and skiing.
Tenderness or a positive Tinel's sign is present over the ulnar nerve within the groove of the medial epicondyle. Other possible physical findings include hypothenar atrophy and index pinch weakness.
Electrodiagnostic tests may be positive, but false-negative test results are common. Radiographs are often normal but may show olecranon hypertrophy, osteophytes, medial calcifications or loose bodies.
The ulnar nerve can also be compressed at the wrist (Guyon's canal). Similar symptoms can be caused by cervical radiculopathy and thoracic outlet syndrome. Attention to these related areas is necessary to make the correct diagnosis.
Treatment
Overuse injuries that cause elbow pain are generally treated using the acronym PRICEMM: protection, rest, ice, compression, elevation, medication and modalities (physical therapy). Initial control of inflammation, appropriate short-term activity modification and a rehabilitation exercise program are successful in most patients with these injuries.15 Referral for surgical consultation may be necessary for some patients, especially those with nerve entrapment, intra-articular pathology or refractory lesions.