
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2000;61(9):2719-2726
See related patient information handout on using the pessary, written by the authors of this article.
The pessary is an effective tool in the management of a number of gynecologic problems. The pessary is most commonly used in the management of pelvic support defects such as cystocele and rectocele. Pessaries can also be used in the treatment of stress urinary incontinence. The wide variety of pessary styles may cause confusion for physicians during the initial selection of the pessary. However, an understanding of the different styles and their uses will enable physicians to make an appropriate choice. Complications can be minimized with simple vaginal hygiene and regular follow-up visits.
The pessary is one of the oldest medical devices available (Figure 1). The type of pessary that is appropriate for each patient depends on the condition being treated. Although many physicians are unfamiliar with the pessary, it remains a useful device for the nonsurgical management of a number of gynecologic conditions (Table 11–4). Physicians who are familiar with the use of a pessary will be equipped to manage a variety of pelvic support defects, including genuine stress urinary incontinence.

| Stress urinary incontinence |
| Vaginal vault prolapse |
| Cystocele |
| Enterocele |
| Rectocele |
| Uterine prolapse |
| Preoperative preparation |
Uses of the Pessary
PELVIC SUPPORT DEFECTS
The pessary is most commonly used in the nonsurgical management of pelvic support defects. Multiple vaginal deliveries can weaken the musculature of the pelvic floor. Hysterectomy or other pelvic surgery can predispose a woman to weakness of the pelvic floor, as can conditions that involve repetitive bearing down, such as chronic constipation, chronic coughing or repetitive heavy lifting.1
Although surgical repair of certain pelvic support defects offers a more permanent solution, some patients may elect to use a pessary as a temporary management option. As the geriatric population continues to increase, more patients are presenting with pelvic floor defects. While many of these patients are poor candidates for surgery, most of them can safely use a pessary.
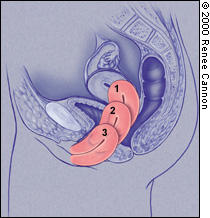
CLASSIFICATION OF UTERINE PROLAPSE
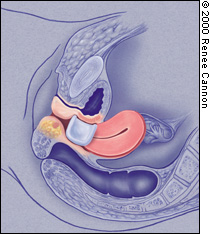
Uterine prolapse is classified by degree (Figure 2). In first-degree uterine prolapse, the cervix is visible when the perineum is depressed. In second-degree prolapse, the cervix is visible outside of the vaginal introitus, while the uterine fundus remains inside. In third-degree prolapse, or procidentia, the entire uterus is outside of the vaginal introitus. Uterine prolapse is associated with incontinence, vaginitis, cystitis and, possibly, uterine malignancy.5
TYPES OF VAGINAL PROLAPSE
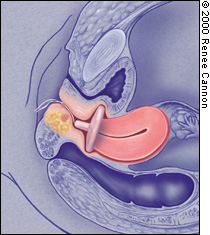
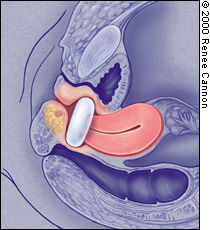
Variants of vaginal prolapse include rectocele, enterocele, cystocele and vault prolapse. A rectocele (Figure 3) occurs when the fascial layers between the rectum and the vagina become weak. This weakening allows the rectum to herniate, causing a bulging of the posterior vagina. The patient may report having to manually reduce the rectocele before defecation. An enterocele is the herniation of the sigmoid colon into the upper posterior vaginal wall. An enterocele differs from a rectocele in that it is a true hernia, lined by peritoneum and usually containing small bowel.
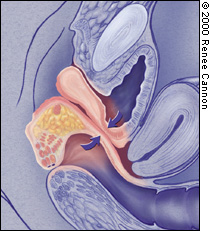
A cystocele (Figure 3) occurs when the tissues between the bladder and the vagina weaken, leading to a herniation of the bladder. This herniation causes a bulge in the anterior vaginal wall. Other portions of the vaginal vault may prolapse as well. Such vault prolapse may or may not cause symptoms.
TREATMENT OF UTERINE PROLAPSE
First- and second-degree uterine prolapse are usually managed with a ring pessary. The donut and inflatable pessaries are also useful in the treatment of mild to moderate uterine prolapse. If the uterine prolapse is associated with a cystocele, a ring pessary with support is useful.
The cube pessary is designed to manage third-degree uterine prolapse. Because the cube is held in place by suction, removal can be somewhat difficult for some patients. This type of pessary can support the uterus even with a lack of vaginal tone. The cube pessary should be removed and cleaned daily, because it has no drainage capability.5
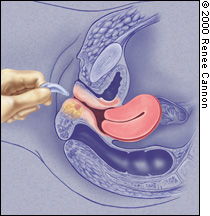
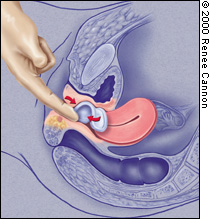
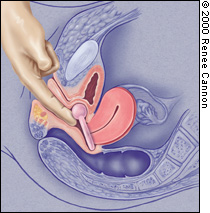
A donut, inflatable or Gellhorn pessary can also be used in patients with third-degree uterine prolapse. The Gellhorn pessary is designed to manage severe uterine or vaginal prolapse. While the Gellhorn offers strong support, it can also be difficult for the patient to remove. If a cystocele or rectocele accompanies the third-degree uterine prolapse, a Gehrung pessary may be the most helpful. However, the Gehrung can be difficult to insert (Figures 4a, 4b and 4c).
TREATMENT OF VAGINAL PROLAPSE
In patients with a mild cystocele, treatment using a ring with support, a dish with support, a Hodge with support or a donut pessary will suffice. To manage a large prolapse of the anterior vaginal wall, the Gellhorn pessary may be the best choice, although insertion and removal can be difficult. Inflatable and cube pessaries are also useful in patients with a larger cystocele. In patients with rectoceles and enteroceles, the use of a Gellhorn, donut, inflatable or cube pessary is usually required to provide the necessary support.
STRESS URINARY INCONTINENCE
Stress urinary incontinence, which is the involuntary loss of urine during exertion, is a common problem that affects many women. In one survey of women older than 18 years, 22 percent complained of symptoms associated with stress urinary incontinence.6
Pessaries should be used by patients for whom conservative management is appropriate. Good candidates for a pessary trial might include a pregnant patient, an elderly woman in whom surgery would be risky and a woman whose previous operation for stress incontinence failed. A pessary can also be used by women who only have stress urinary incontinence with strenuous exercise. The prevalence of stress urinary incontinence with strenuous exercise may be as high as 27 percent.2
INCONTINENCE PESSARIES
The pessary compresses the urethra against the upper posterior portion of the symphysis pubis and elevates the bladder neck. This causes an increase in outflow resistance and corrects the angle between the bladder and the urethra so that Valsalva's maneuvers alone are not strong enough to cause leakage of urine. Any style of pessary that can accomplish this will help with the management of stress urinary incontinence.
The incontinence ring and incontinence dish pessaries are most commonly used in patients with stress urinary incontinence. A Hodge pessary with or without support, depending on the presence of a cystocele, can also be used. Introl, a bladder neck support prosthesis that is marketed by Uromed, is also available (Figure 5). The prosthesis has two prongs that support the urethrovesical junction and bladder neck. This device was found to be effective in 83 percent of adult women with stress urinary incontinence.7

For women who have urinary incontinence during strenuous activities such as jogging, aerobics or tennis, a cube pessary that is inserted before exercise may be all that is needed. A Hodge pessary with support is also effective in the prevention of exercise incontinence.3
The pessary can be used to differentiate between patients with stress urinary incontinence that is secondary to a correctable anatomic defect and those with bladder instability. A properly fitted pessary can simulate the result of surgical correction of incontinence, thereby yielding diagnostic and prognostic information.8
Management
SELECTION AND FITTING
Selection of an appropriate pessary depends primarily on the condition for which the patient is being treated. [ corrected] Pessaries are available from Milex, the largest manufacturer, at a cost of $31.00 to $51.50 per pessary. Of the pessaries that are indicated for a particular condition (Table 21–4,7), the style that works the best for the particular patient should be chosen. For example, a Gellhorn pessary can offer excellent support for uterine prolapse as long as the perineal body is intact. If the perineal body is weak, a cube or donut pessary will be more effective.4 An incontinence ring pessary usually helps with stress urinary incontinence, but if the patient has some degree of cystocele, a Hodge with support or a Gehrung pessary may be more effective.
| Type | Uses | Most common sizes | Ease of insertion and removal |
|---|---|---|---|
| Ring* | Mild uterine prolapse | 3 to 5 | Easy |
| Incontinence ring* | Stress urinary incontinence | 2 to 7 | Easy |
| Ring with support* | Mild uterine prolapse | 3 to 5 | Easy |
| Mild cystocele | |||
| Incontinence dish* | Stress urinary incontinence | 3 to 5 | Medium |
| Mild uterine prolapse | |||
| Dish with support* | Mild cystocele | 3 to 5 | Medium |
| Stress urinary incontinence | |||
| Mild uterine prolapse | |||
| Donut* | Moderate uterine prolapse | 2 1/2 to 3 inches | Medium |
| Mild cystocele | |||
| Gellhorn* | Moderate uterine prolapse | 2 1/4 to 2 3/4 inches | Difficult |
| Mild cystocele | |||
| Inflatable* | Moderate uterine prolapse | Medium and large | Easy |
| Cube* | Moderate to severe uterine prolapse | 2 to 4 | Medium |
| Mild cystocele | |||
| Mild rectocele | |||
| Other vaginal vault prolapse | |||
| Gehrung* | Moderate to severe cystocele | 3 to 5 | Difficult |
| Mild rectocele | |||
| Moderate to severe uterine prolapse | |||
| Gehrung with knob* | Same uses as Gehrung | 3 to 5 | Difficult |
| Stress urinary incontinence | |||
| Hodge* | Mild cystocele | 2 to 4 | Medium |
| Hodge with support* | Mild cystocele | 2 to 4 | Medium |
| Stress urinary incontinence | |||
| Smith, Risser* | Mild cystocele | 2 to 4 | Medium |
| Stress urinary incontinence | |||
| Introl† | Stress urinary incontinence | Call manufacturer | Easy |
Pessaries are fit by trial and error. In patients who use a diaphragm, the size of the diaphragm does not correlate with the size of the pessary. Proper fitting of the pessary often requires the patient to try several sizes and/or styles. A variety of styles and sizes should be made available during the patient's fitting session. The manufacturer of the pessary can provide pessaries in the most common sizes that will fit the majority of patients. The manufacturer can also provide detailed instructions on how to fit each particular style of pessary.
After a complete pelvic examination has been performed, the physician should start with an average-sized pessary in the simplest style. When the pessary has been put into place, the fit and effectiveness should be checked (Figures 6 through 8). The largest pessary that the patient can wear comfortably is generally the most effective. The examiner's finger should pass easily between the pessary and the vaginal wall. The physician should check the pessary to be sure that the intended function is met. When the indication of the pessary is for stress urinary incontinence, the patient should cough to test for any leakage of urine.
Finally, the examiner should ask the patient to stand, sit, squat and perform Valsalva's maneuvers to be sure that the device will not become dislodged. It is also recommended that the patient void before leaving the office. If the patient is unable to void with the pessary in position, the device should be removed and the patient should be fitted with the next smaller size. The patient should be instructed to immediately report any discomfort or difficulty with urination or defecation while wearing the pessary.
CONTRAINDICATIONS
There are few contraindications to the use of a pessary. Active infections of the pelvis or vagina, such as vaginitis or pelvic inflammatory disease, preclude the use of a pessary until the infection has been resolved. Patients who are noncompliant or unlikely to follow up should not be fitted for a pessary. Most pessaries are made of silicone; some are made of latex. An allergy to the product would also be a contraindication.
FOLLOW-UP
After the initial fitting of the pessary, the patient should be followed-up within a few days so that the physician can recheck the fit. The pessary should be removed so that the vagina can be examined for irritation, pressure sores or allergic reaction. Having to change the size of the pessary at least once after the initial fitting is not uncommon. The patient should then be instructed to follow-up within one to two weeks for another examination, after which time the examinations can be spaced to every two to three months. In the motivated patient who is able to demonstrate effective removal, insertion and care of the pessary, these examinations may be spaced further at the discretion of the physician.9
At each follow-up examination, the pessary should be removed and cleaned with soap and water while the vagina is inspected for erosions, pressure necrosis or allergic reaction. If inspection of the pessary reveals cracking or other defects, it should be replaced. The patient who is using a pessary should be considered to be under the care of the person who placed it for the duration of its use. Pessaries should never be placed in elderly, debilitated patients without excellent follow-up.
COMPLICATIONS
Although the pessary is an extremely safe device, it is still a foreign body in the vagina. Because of this, the most common side effect of the pessary is increased vaginal discharge and odor.4 This side effect can be minimized with the use of an acidic vaginal gel such as Trimo-San, which also helps to relieve minor irritation and itching. Some physicians recommend that patients douche with dilute vinegar or hydrogen peroxide for relief.4,10
A pessary that is neglected can become embedded in vaginal mucosa and may be difficult to remove. In some cases, the use of estrogen cream may enable easier removal of the pessary by decreasing inflammation and promoting epithelial maturation.11 In extreme and rare cases, the pessary must be removed surgically.4 Even with a neglected, embedded pessary, the development of a fistula is extremely rare.4
In the patient with an improperly fitted ring pessary, the cervix and lower uterus can herniate through the open center of the ring and become incarcerated. If not recognized, this incarceration could lead to strangulation and necrosis of the cervix and uterus.4
While vaginal cytology may reveal inflammatory changes, the presence of a pessary does not increase the patient's risk of developing vaginal cancer.4
Final Comment
Although many physicians are unfamiliar with the pessary, this useful gynecologic device has stood the test of time. Currently, family practice and obstetrics–gynecology residencies include little education and training on the use of the pessary.11 Incorporating the use of the pessary into a physician's practice requires minimal investment; however, it may significantly improve the lifestyle of patients who have limited therapeutic alternatives. The pessary is clearly a safe and useful treatment alternative for a number of gynecologic conditions that are seen by family physicians every day.