
Am Fam Physician. 2000;61(9):2749-2756
See related patient information handout on preventing noise-induced hearing loss, written by the author of this article.
Hearing loss caused by exposure to recreational and occupational noise results in devastating disability that is virtually 100 percent preventable. Noise-induced hearing loss is the second most common form of sensorineural hearing deficit, after presbycusis (age-related hearing loss). Shearing forces caused by any sound have an impact on the stereocilia of the hair cells of the basilar membrane of the cochlea; when excessive, these forces can cause cell death. Avoiding noise exposure stops further progression of the damage. Noise-induced hearing loss can be prevented by avoiding excessive noise and using hearing protection such as earplugs and earmuffs. Patients who have been exposed to excessive noise should be screened. When hearing loss is suspected, a thorough history, physical examination and audiometry should be performed. If these examinations disclose evidence of hearing loss, referral for full audiologic evaluation is recommended.
Noise-induced hearing loss is a sensorineural hearing deficit that begins at the higher frequencies (3,000 to 6,000 Hz) and develops gradually as a result of chronic exposure to excessive sound levels.1 Although the loss is typically symmetric, noise from such sources as firearms or sirens may produce an asymmetric loss. Acoustic trauma, a related condition, results from an acute exposure to short-term impulsive noise.2
Noise Exposure
Noise is perhaps the most common occupational and environmental hazard. As many as 30 million Americans are exposed to potentially harmful sound levels in their workplaces.3 Outside of work, many persons pursue recreational activities that can produce harmful noise. Sixty million Americans own firearms, and many use them without adequate hearing protection.4 Other nonoccupational sources of noise include chain saws and other power tools, amplified music,5 and recreational vehicles such as snowmobiles and motorcycles. Some types of toys for children can produce sounds capable of causing permanent hearing damage.6
Noise can be described in terms of intensity (perceived as loudness) and frequency (perceived as pitch). Both the intensity and the duration of noise exposure determine the potential for damage to the hair cells of the inner ear. Even sounds perceived as “comfortably” loud can be harmful.
Sound intensity is measured as sound pressure level (SPL) in a logarithmic decibel (dB) scale (Table 1). Noise exposure measurements are often expressed as dB(A), a scale weighted toward sounds at higher frequencies, to which the human ear is more sensitive. Noise can cause permanent hearing loss at chronic exposures equal to an average SPL of 85 dB(A) or higher for an eight-hour period.7 Based on the logarithmic scale, a 3-dB increase in SPL represents a doubling of the sound intensity. Therefore, four hours of noise exposure at 88 dB(A) is considered to provide the same noise “dose” as eight hours at 85 dB(A), and a single gunshot, which is approximately 140 to 170 dB(A), has the same sound energy as 40 hours of 90-dB(A) noise.8
| Sound | Loudness (dB) |
|---|---|
| Gunshot (peak level) | 140 to 170 |
| Jet takeoff | 140 |
| Rock concert, chain saw | 110 to 120 |
| Diesel locomotive, stereo headphones | 100 |
| Motorcycle, lawnmower | 90 |
| OSHA level for hearing conservation program | 85* (8-hour time-weighted average) |
| Conversation | 60 |
| Quiet room | 50 |
| Whisper | 30 to 40 |
Epidemiology
Noise-induced hearing loss is the second most common sensorineural hearing loss, after age-related hearing loss (presbycusis). Of the more than 28 million Americans with some degree of hearing impairment, as many as 10 million have hearing loss caused in part by excessive noise exposure in the workplace or during recreational activities.9 The economic costs of occupational hearing loss have been estimated to be in the billions of dollars.10 Noise-induced hearing loss has been well recognized since the industrial revolution. An early term for the condition was “boilermakers' disease,” because so many workers who made steam boilers developed hearing loss.11 In today's noisy society, even children and young adults are at risk. A recent study found evidence of high-frequency hearing loss in nearly one third of a cohort of college students.12
Pathophysiology
To be perceived, sounds must exert a shearing force on the stereocilia of the hair cells lining the basilar membrane of the cochlea. When excessive, this force can lead to cellular metabolic overload, cell damage and cell death. Noise-induced hearing loss therefore represents excessive “wear and tear” on the delicate inner ear structures. Concurrent exposure to ototoxic substances, such as solvents and heavy metals, may increase the damage potential of noise.7 Once exposure to damaging noise levels is discontinued, further significant progression of hearing loss stops. Individual susceptibility to noise-induced hearing loss varies greatly, but the reason that some persons are more resistant to it while others are more susceptible is not well understood.13
Recent animal experiments suggest that free oxygen radicals may mediate noise damage to hair cells.14 In the future, use of chemoprotective agents such as antioxidants as well as identification of host risk factors for susceptibility to noise-induced hearing loss, may enhance prevention and treatment efforts.
Illustrative Cases
CASE 1
A teenaged girl was seen for a school physical examination. Screening audiometry performed in the office revealed a 30-dB (mild) elevation of hearing thresholds at 4,000 Hz. A confirmatory audiogram taken by an audiologist showed a sensorineural loss in a “notch” pattern at 4,000 Hz (Figure 1). In response to questioning, the girl reported spending several hours a day listening to music through head-phones. The previous night, she had spent several hours at a rock concert without wearing hearing protection. Afterward, she noticed that her ears were ringing and “felt like there was cotton in them.” Several days later, her hearing had returned to normal.
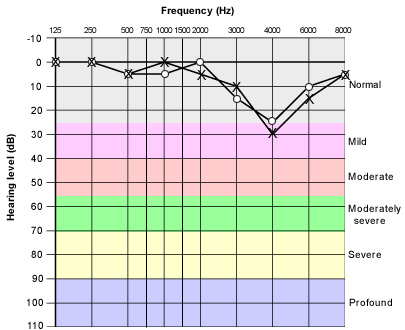
This patient is an example of a person who has experienced a “temporary threshold shift.” Temporary threshold shifts are common in persons exposed to excessive noise, and they represent transient hair cell dysfunction. Although complete recovery from a given episode can occur, repeated episodes of such shifts occurring after noise exposures give way to permanent threshold shifts because hair cells in the cochlea are progressively lost.
CASE 2
A 55-year-old factory worker consulted his family physician because of ringing in his ears and depression that began soon after the onset of the tinnitus. He had seldom worn hearing protection at work, where he had to shout to communicate with co-workers. Away from work, he had difficulty understanding conversations in crowded rooms, and he said he often argued with his wife about the volume of the television set. His physical findings were normal. An office audiogram showed a high-frequency hearing loss (Figure 2). The patient was referred to an audiologist, who confirmed a sensorineural hearing loss that was probably caused by excessive noise exposure, with superimposed age-related changes. A hearing aid was prescribed.
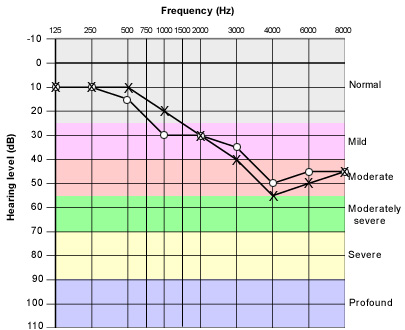
This case shows that noise-induced hearing loss can interfere with speech discrimination and social functioning. The high-frequency deficit causes difficulty in perceiving and differentiating consonant sounds; patients often report that words “run together.” High-pitched sounds, such as a baby crying or a distant telephone ringing, may not be perceived at all. Tinnitus is a common symptom of noise overexposure, and it further interferes with hearing acuity, sleep and concentration. These impairments have been associated with social isolation, depression and an increased risk of accidents.15,16
Primary Prevention
Although no studies have evaluated the efficacy of educating patients about noise-induced hearing loss, family physicians can easily screen for excessive noise exposure during health maintenance visits (Table 2). An example of a screening question is: “Are you exposed to excessive noise in your workplace or through music or hobbies?” During well-child visits, parents can be asked whether the child plays with noisy toys. Adolescents and their parents should be counseled about exposure to amplified music. Adults should be asked about firearms, noisy hobbies and noise exposure at work. A positive response to the “shout” test—that is, if a person gives an affirmative answer when asked whether it is necessary to shout to converse with someone at arm's length in the workplace—indicates a potentially hazardous noise level.
| Condition | Screening techniques | Preventive strategies | |
|---|---|---|---|
| Excessive noise exposure | History: “Are you exposed to excessive noise in your workplace or through music or hobbies?” “Shout” test: “Do you often have to shout to talk to someone at arm's length because it's so noisy around you?” Specific sources of noise: firearms, loud music, motorcycles, snowmobiles, power tools Hearing protection: “How often do you use earplugs, earmuffs, etc.?” | Educate and motivate patient. Point out that: | |
| “Hearing health” is part of a healthy lifestyle. | |||
| Noise-induced hearing loss is permanent and only partially treatable, yet virtually 100 percent preventable. | |||
| Excessive noise should be avoided when possible. | |||
| Hearing protection should be used correctly and consistently during exposure to excessive noise. | |||
| Patients should be made aware of the availability of hearing protection and ways to use it correctly. | |||
| Hearing impairment | History: “Do you have any difficulty with understanding speech in noisy environments? Do you need to turn up the television volume? Do you ask people to repeat sentences?” “Is your hearing not as good as it was 10 years ago?” “Have family members noticed a problem with your hearing?” Physical examination: otoscopic examination, Rinne and Weber tuning fork tests Other: office audiometry, tympanometry | Refer patient to audiologist/otolaryngologist if hearing loss is strongly suspected. Encourage patient to seek treatment. | |
| Assist patient and family in coping with hearing deficit. | |||
| Advise patient to use hearing protection and avoid excessive noise (lifelong) to limit further hearing loss. | |||
A patient who reports significant exposure to noise should be informed that noise-induced hearing loss, although permanent and not fully treatable, is virtually 100 percent preventable. The clinician can motivate patients to maintain their hearing health and thereby reduce the risk of hearing disability as they grow older (Tables 2 and 3). Key factors in this effort are learning to avoid excessive noise when possible and correctly using hearing protection when necessary. Hearing protectors, including earmuffs, disposable earplugs and custom-fitted earplugs, can provide 20 to 40 dB of attenuation when used correctly. Physicians can obtain samples from manufacturers and keep them in the office for distribution and demonstration of techniques for proper use. Counseling about hearing protection is effective, although there is no evidence in favor of physician counseling.17
| The Council for Accreditation in Occupational Hearing Conservation conducts courses in audiometry and hearing conservation for audiologists, audiometric technicians and medical professionals. | |
| Council for Accreditation in Occupational Hearing Conservation | |
| 611 E. Wells St., Milwaukee, WI 53202 | |
| Telephone: 414-276-5338. | |
| Web address: http://www.caohc.org | |
| The National Institute for Occupational Safety and Health (NIOSH) and the National Institute on Deafness and Other Communication Disorders (NIDCD) are conducting a public awareness campaign on the causes and prevention of noise-induced hearing loss. | |
| NIOSH information: 800-35-NIOSH | |
| Web address: http://www.cdc.gov/niosh | |
| The National Hearing Conservation Association is a membership organization of professionals engaged in hearing conservation; the group also produces educational materials. | |
| National Hearing Conservation Association | |
| 9101 E. Kenyon Ave., Ste. 3000, Denver, CO 80237 | |
| Telephone: 303-224-9022 | |
| Web address: http://www.hearingconservation.org | |
| The League for the Hard of Hearing produces educational materials and programs about the noise hazards of toys and other common noise sources. | |
| League for the Hard of Hearing | |
| 71 W. 23rd St., New York, NY 10010-4162 | |
| Telephone: 917-305-7700 (voice) or 917-305-7999 (TTY). | |
| Web address: http://www.lhh.org/noise | |
| The Sight and Hearing Association distributes “Know Noise,” a curriculum for third- to sixth-grade students on prevention of noise-induced hearing loss | |
| Sight and Hearing Association | |
| 674 Transfer Rd., St. Paul, MN 55114-1402 | |
| Telephone: 651-645-2546 or 800-992-0424 | |
| Web address: http://www.sightandhearing.org | |
Occupational Hearing Conservation
The Occupational Safety and Health Administration (OSHA) mandates that employers provide hearing conservation programs for their employees in workplaces where noise levels equal or exceed 85 dB(A) for an eight-hour time-weighted average. An occupational hearing conservation program includes engineering and administrative controls to reduce noise exposures, employee training in the use of hearing protection and annual audiometry for all workers who are exposed to noise.
Physicians providing occupational health services to a company may supervise the hearing conservation program, review abnormal audiograms and advise the program administrator. A worker whose audiogram shows a “standard threshold shift” (worsening of 10 dB on average at 2,000, 3,000 and 4,000 Hz when compared with the employee's baseline test) must be notified and receive additional training and evaluation.
Screening for Hearing Impairment
The U.S. Preventive Services Task Force recommends periodic screening of older adults for hearing impairment.17 Other authorities have advocated similar screening for all patients who report significant noise exposure.17 The clinician can ask patients if they have difficulty understanding speech in noisy environments, if they need to turn up the television volume or if they frequently have to ask people to repeat sentences. Standardized questionnaires for hearing handicap are available (Figure 3).18,19 Some patients may be reluctant to admit hearing loss, and family members may be the first to report a problem.
If the clinician suspects hearing loss, a careful history of symptoms such as hearing loss, discharge, tinnitus and vertigo should be obtained; the ears should then be examined, and audiometry performed. The physical examination of the ears should assess presence of cerumen impaction or evidence of middle ear disease. The Weber and Rinne tests, performed with a 512-Hz or 1,024-Hz tuning fork can provide clues to whether the loss is conductive or sensorineural. In the Weber test (Figure 4), sound will lateralize to the side away from a sensorineural loss and toward a conductive deficit. The Rinne test (Figure 5) will demonstrate air conduction better than bone conduction if the loss is sensorineural. If available, office tympanometry can also help detect conductive hearing problems.
Audiometry is necessary to confirm a hearing deficit because physical tests of hearing, such as the whispered voice and the finger-rub test, are not as reliable.20 Office audiometry is sufficiently sensitive and specific to serve as a screening method.21 Screening audiometers for office use generally test at several frequencies in the speech range between 500 and 4,000 Hz. Audiometers must be calibrated regularly (at least annually) and used in a quiet room. An audiogram hearing threshold level above 20 dB is considered abnormal.
If the loss appears to be sensorineural, etiologies other than noise should be excluded. While this type of loss in early childhood is often caused by congenital factors,22 presbycusis becomes the most common sensorineural condition after midlife. The differential diagnosis of sensorineural hearing loss is listed in Table 4.
| Condition | Causative agents | Features | Typical audiogram pattern |
|---|---|---|---|
| Age-related hearing loss (presbycusis) | Unknown | Gradual onset | Bilateral high-frequency loss, “downsloping” |
| Congenital hearing loss | Genetic factors, prenatal infections/toxic exposures, birth trauma | Present at birth | Variable |
| Noise-induced hearing loss | Noise exposure | Gradual onset, tinnitus common | Bilateral high-frequency loss, “notch” at 3,000 to 4,000 Hz |
| Sudden hearing loss | Viral infections, trauma, vascular, drugs | Sudden onset, otologic emergency | Variable; may be unilateral or bilateral |
| Neoplastic | Acoustic neuroma (vestibular schwannoma), other tumors | Usually gradual onset; tinnitus may be present | Unilateral loss |
| Meniere's disease | Unknown (may be endolymphatic hydrops) | Fluctuating, progressive hearing loss, tinnitus, vertigo | Low-frequency loss, “upsloping” or flat |
| Ototoxicity | Chemotherapeutic agents (cisplatin [Platinol], nitrogen mustard), aminoglycosides, furosemide (Lasix), salicylates, quinine | May be accompanied by tinnitus, vertigo, nystagmus | Usually bilateral, symmetric, highfrequency (may be very high frequency) |
| Other | Infections: herpes, meningitis, mumps, syphilis, tuberculosis | Often gradual onset, associated disease | Variable |
| Systemic disease: vasculitis, renal failure, head injury | |||
| Genetic factors, idiopathic |
Referral
A patient whose screening shows evidence of hearing loss should be referred for a full audiologic evaluation. Audiologists can test a greater number of frequencies and can measure air and bone conduction to confirm whether the loss is sensorineural, conductive or mixed. They can also perform tests for speech discrimination and speech reception threshold.
If a unilateral or asymmetric sensorineural loss, tinnitus, vertigo or other significant ear pathology is found, referral to an otolaryngologist is warranted. Patients with sudden sensorineural hearing loss (hearing loss developing in minutes or hours) should be referred immediately, because treatment initiated within the first 24 hours can improve outcomes.23
Management
Currently, the treatment of noise-induced hearing loss is limited to hearing amplification and counseling. Initially, patients may be reluctant to consider using hearing aids, associating them with the stigma of “old age.” The family physician can encourage a patient with significant hearing loss to seek treatment and can work with the patient and family to help them cope with a hearing disability. Hearing aids can amplify sounds but, despite technologic advances, often cannot fully correct problems of speech discrimination. An aid should be carefully matched to the person's hearing deficit and lifestyle by a trained audiologist. Vocational rehabilitation may be necessary to ensure that patients can function safely and effectively with their hearing impairment.
Final Comment
Noise exposure, whether occupational or recreational, is the leading preventable cause of hearing loss. By preventing noise-induced hearing loss, patients can reduce the impact of age-related changes on their hearing. Family physicians should educate and motivate patients of all ages to avoid potentially damaging noise, use hearing protection when necessary and seek treatment for an existing hearing deficit.