
Am Fam Physician. 2000;61(10):3035-3042
Age-related macular degeneration is the leading cause of severe vision loss among the elderly. In this condition, central vision is lost, but peripheral vision almost always remains intact. Affected persons rarely require canes or guide dogs. The diagnosis of age-related macular degeneration is based on symptoms and ophthalmoscopic findings, and the disease can be classified into atrophic and exudative forms. The two currently proven treatments are laser photocoagulation and photodynamic therapy, but these measures are effective in only a small fraction of eyes with the exudative form of macular degeneration. Vision rehabilitation can help patients maximize their remaining vision and adapt so that they can perform activities of daily living. Families need encouragement in providing support and helping patients adjust to being partially sighted.
Elderly persons are concerned about losing independence and mobility. Studies have shown that loss of central visual acuity leads to a reduction of daily activities and mobility in the elderly.1 Loss of central visual acuity also increases the risks of falls, fractures and depression in this population.2
Age-related macular degeneration is the leading cause of severe vision loss in older Americans.3,4 In this condition, the central portion of the retina (the macula) deteriorates, and central vision can be lost. Central vision is the “high-definition” vision that is required for reading, driving, watching television, recognizing people and performing many other activities of daily of living. Peripheral vision generally remains intact, and elderly persons with age-related macular degeneration rarely require canes or guide dogs. However, they have been found to have lower quality-of-life scores than persons with chronic obstructive pulmonary disease or acquired immunodeficiency syndrome.5–8
With the continued growth of the elderly population in the United States, family physicians are frequently asked about vision and macular degeneration. As life expectancy continues to increase, age-related macular degeneration will become an increasingly important problem.
Epidemiology
Age-related macular degeneration has been examined in many population-based epidemiologic studies.9–12 The Third National Health and Nutrition Examination Survey10 was a population-based survey of a representative sample of the U.S. population 40 years of age and older. For this survey, the presence of age-related macular degeneration was based on the grading of fundus photographs. The estimated prevalence of the disease was 9.2 percent among civilian, noninstitutionalized persons 40 years of age and older. Macular degeneration was noted to be more prevalent in non-Hispanic whites (9.3 percent) than in blacks (7.4 percent) or Mexican Americans (7.1 percent). The survey also included other Hispanic groups, as well as Asian Americans and Native Americans, but their numbers were too small for meaningful comparisons. Early age-related macular degeneration was found to be more prevalent in persons 60 years of age and older than in persons 40 to 59 years of age. Late disease was only found in persons 60 years of age and older.
Few studies have evaluated the incidence of age-related macular degeneration. In the Beaver Dam Eye Study,13 pure geographic atrophy (late age-related macular degeneration) was 16.6 times more likely to develop in persons 75 years of age than in persons who were younger at baseline. The incidence of exudative changes increased from zero percent in persons less than 55 years of age to 1.8 percent in persons 75 years or older at baseline.
Pathophysiology
The pathophysiology of age-related macular degeneration is still under investigation. The location of the disease also remains a subject of debate. Some investigators believe that the disease resides in the neural retina (rods and cones), whereas others are studying the retinal pigment epithelium (the layer of cells that provide nutrition to the rods and cones).
| Risk factor | Comments |
|---|---|
| Age | The prevalence of macular degeneration increases with age.10–13 |
| Cardiovascular disease | Age-related macular degeneration has a weak association with cardiovascular disease.14 |
| Laser photocoagulation as a treatment for the disease is less likely to be successful in patients who also have hypertension.15 | |
| The risk of developing exudative macular degeneration is three times higher in cigarette smokers than in nonsmokers.16 | |
| Ethnicity | The Third National Health and Nutrition Examination Survey indicated that age-related macular degeneration is more prevalent in non-Hispanic whites than in blacks or Mexican Americans.10 |
| Gender | Exudative disease is probably more common in women than in men.12 |
| Genetics | Genetic predisposition has been investigated, but its role is not defined.17–19 Genetic factors appear to be more directly related to early-onset macular degenerations (entities that are different from age-related macular degeneration). |
Vision Screening
The American Academy of Family Physicians recommends Snellen acuity testing in asymptomatic elderly patients.20 The U.S. Preventive Services Task Force also recommends Snellen acuity testing for the elderly but notes that insufficient evidence is available to recommend a specific frequency of screening, specific screening questions or routine use of screening ophthalmoscopy.21 The American Academy of Ophthalmology recommends comprehensive eye examinations every one to two years in patients more than 65 years of age who do not have conditions requiring intervention.22
Diagnosis
Patients with age-related macular degeneration may complain of acute loss of vision, blurred vision, scotomas (areas of lost vision) or chronic distortion of vision. All patients with vision loss should be referred to an ophthalmologist; those with acute loss of vision should be referred urgently.
Age-related macular degeneration is a clinical diagnosis that is usually based on the presence of visual disturbances and characteristic findings on dilated examination of the macula. The disease is usually classified as early or late. Late disease can be divided into atrophic (dry) and exudative (wet) forms.23
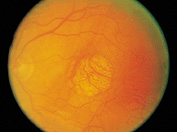
In early disease, the macula shows yellowish-colored subretinal deposits called “drusen” (Figure 1) and/or increased pigment. Drusen are thought to be byproducts of retinal pigment epithelium dysfunction. In most eyes with early disease, visual acuity remains stable for many years, and loss of vision is usually gradual.

Late disease (atrophic and exudative) can lead to significant loss of vision. Exudative disease occurs in only 10 percent of patients with age-related macular degeneration, but it is responsible for 80 to 90 percent of cases of severe vision loss related to the disease.24
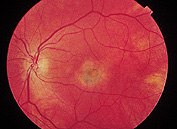
Fluorescein angiography can be used to confirm the diagnosis and to help determine whether a patient has the atrophic or exudative form of the disease (Figure 4). In most instances, this modality is employed to determine whether an eye with exudative disease is eligible for laser treatment.

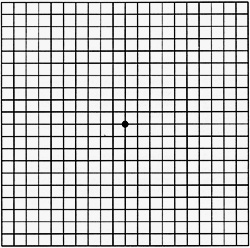
The Amsler's grid (Figure 5) is an effective tool for detecting the progression of age-related macular degeneration. The patient is given a copy of the grid and is instructed to focus one eye on the center dot in the grid from a distance of 35 cm (12 in) with the other eye covered; the procedure is then repeated for evaluation of the other eye. The patient performs this test daily at home and is instructed to call the physician if line distortions or scotomas are detected and persist for one or two days.
Treatments with Proven Effectiveness
LASER PHOTOCOAGULATION
Laser photocoagulation has been shown to be effective in the treatment of eyes with exudative disease and well-defined, or “classic,” subretinal neovascularization.25–27 Unfortunately, well-defined subretinal neovascularization is present in only about 15 percent of eyes with exudative disease. Most patients have sub-retinal neovascularization that is “occult” (i.e., covered by blood or thick subretinal fluid).28
Fluorescein angiography is performed to image the neovascular vessels for the purpose of differentiating between classic and occult subretinal neovascularization.
In eligible eyes, laser photocoagulation can reduce the risk of further vision loss, but it does not usually restore lost vision. Even after successful treatment of the bleeding vessels, choroidal neovascularization can recur and cause further vision loss.
Laser treatment is an outpatient procedure that requires only topical anesthetic drops. Patients have no restrictions before or after treatment.
PHOTODYNAMIC THERAPY
Photodynamic therapy is a new treatment that takes advantage of certain unique properties of subretinal neovascular vessels. Compared with normal blood vessels, neovascular tissue appears to differentially retain the dye used in photodynamic therapy.
After dye has been injected in a peripheral vein, it is “excited” with laser light. This activated dye then forms reactive free radicals that close down the leaky subretinal vessels. Because normal retinal vessels retain very little dye, the abnormal subretinal vessels are selectively “damaged.”
Clinical trials of one dye (verteporfin) showed that patients who underwent photodynamic therapy had a lower rate of vision loss than those treated with placebo (39 versus 67 percent).29 However, recurrences of sub-retinal neovascularization and loss of vision were common, and patients had to be retreated three or more times during the first year of follow-up. After each injection, patients had to avoid exposure to the sun and other sources of bright light. Side effects reported during the first year included injection-site problems, photosensitivity and infusion-related back pain.
Unfortunately, photodynamic therapy is effective only in patients with well-defined neovascularization. In addition, data on retreatments and follow-up are limited to one year, and the long-term risks of treatment are still unknown.
Experimental Treatments
PHARMACOLOGIC THERAPIES
Clinical trials have not proved any drugs to be effective in preventing or treating atrophic or exudative age-related macular degeneration. Because hypertension and smoking are associated with a poorer response to laser photocoagulation, as well as with more advanced disease, blood pressure control and smoking cessation should be recommended.
A number of drugs have been or are being investigated for use in the treatment of sub-retinal neovascularization (exudative form). However, patients and physicians should remember that experimental treatments can be harmful.
RADIATION THERAPY
Radiation therapy for exudative macular degeneration has also been attempted. Reports on external-beam irradiation are equivocal at best, and no data on charged-particle (proton-beam) therapy have been published.
NUTRITION
Numerous observational studies have suggested that nutrition plays an important role in age-related macular degeneration. In one observational study,30 patients who ate a diet high in fruits and vegetables, especially green leafy vegetables such as spinach and kale, were shown to have a lower risk of exudative disease.
Although observational studies have supported the value of eating foods that are high in antioxidants, clinical trials have provided no evidence for antioxidant supplementation in pill form. Furthermore, results from clinical trials of β-carotene prophylaxis in Finnish smokers and U.S. asbestos workers suggested that caution should be exercised in taking pharmacologic dosages of any antioxidant.31,32 In these trials, the risks of lung cancer and death were greater in patients taking β-carotene than in those who received placebo.
Researchers now believe that supplementing carotenoids in pill form may be potentially harmful. Increasing evidence indicates that supplementation with one carotenoid may lead to reduced serum levels of other carotenoids.33 Because there are more than 50 naturally occurring carotenoids, family physicians need to be confident about choosing the “right” nutrient for supplementation: supplementing with the “wrong” carotenoid may lead to lower levels of a needed nutrient.
The National Eye Institute is currently sponsoring the Age-Related Eye Disease Study, an ongoing clinical trial that is investigating the effect of oral antioxidant supplements. Pending the results of this trial, which are expected in late 2001, family physicians might advise patients with age-related macular degeneration to eat a diet high in fruits and leafy, green vegetables and to take a daily multivitamin pill if they are still concerned about their antioxidant status. Sources of dietary carotenoids are listed in Table 2.34
SURGERY
Subretinal surgery and macular translocation are two experimental surgical procedures currently being investigated for the treatment of age-related macular degeneration.
Subretinal surgery is performed to remove abnormal subretinal neovascularization in patients with exudative disease. This procedure is currently under investigation in the Submacular Surgery Trials, which are being sponsored by the National Institutes of Health.
In macular translocation surgery, the macula is surgically detached and moved from a more diseased area of retinal pigment epithelium to a less diseased area. Only a few reports on this procedure have appeared in the literature. Clinical observations by ophthalmologists indicate that the procedure is difficult to perform and is associated with significant ocular morbidity, such as retinal detachment and vision loss.
Psychosocial Impact of Age-Related Macular Degeneration
With increasing loss of central vision, patients lose their ability to read and to conduct certain activities of daily living. Working elderly patients may worry about losing their income or their ability to achieve life goals. Patients may also find that their self-image changes from that of a responsible, active person to that of a person who must depend on others for help. With changes in their ability to function independently, elderly patients may have additional expenses for help with daily activities and travel.
Along with the ophthalmologist, the family physician will need to monitor the mental health of the patient with age-related macular degeneration. Partially sighted persons may have difficulty adjusting to their decreased vision and may experience higher levels of anxiety and loneliness than those who are totally blind.14 With progression of the macular degeneration, patients may experience many episodes of mourning. These repeated episodes of grief may also be stressful for family and friends.
In addition to giving needed emotional comfort, families will probably be asked to provide physical and financial assistance. Elderly persons with macular degeneration will require help with simple tasks such as cooking (e.g., reading recipes and finding ingredients), paying bills and taking medications. As they become unable to drive, they will need help getting to medical appointments and visits with friends and family, contacts that are crucial in preventing isolation and subsequent depression.
Vision Rehabilitation
Patients should be encouraged to consider ways to maximize their remaining vision so that they can master some daily activities (Table 3).35 Low-vision professionals can be of great service in assessing residual vision, recommending optical aids and devices, and providing training in the optimal use of these aids (Table 4).
| Vision devices | Type | Comments |
|---|---|---|
| Near-vision devices | Direct illumination (e.g., gooseneck or other adjustable lamp) | Enhanced lighting can sharpen images. |
| Magnifiers | Magnifiers are available as hand-held instruments or as devices that can be attached to table or floor stands. | |
| High-power reading glasses | These glasses provide additional magnification to assist with reading. | |
| Telescope focused for near vision | In miniaturized form, telescopes can be mounted in glasses | |
| Closed-circuit television | Letter size can be magnified, and letter color and background can be changed. | |
| Distant-vision devices | Telescope | Telescopes can be mounted on glasses or held in the hand. |
| Protective filters, sun lenses | Special filters and lenses can improve contrast and reduce glare | |
| Nonoptical aids | Bold-lined paper, guides for writing checks and addressing envelopes | Bold-lined paper helps with writing. For check writing, special cut-out stencils identify where information needs to be written (payee, date, amount, etc.). Stencils for envelopes can be used to correctly place mailing and return addresses. |
| Reading stands | These stands allow material to be positioned to facilitate reading. | |
| Colored acetate filters | Clear sheets of colored plastic enhance contrast and thereby improve vision. | |
| Large-print publications | Publications with large font sizes are available at most public libraries. | |
| Special dials for television and stove | Dials with large lettering can be attached to certain televisions and stoves to help in selecting desired settings. |
| Use contrasting colors for cup, soap and soap dish. |
| Install a wall-mounted soap dispenser. |
| Install a wall-mounted mirror with an extension arm (for use while shaving or applying makeup). |
| Organize and alphabetize contents of the medicine cabinet. |
| Keep all bathroom cabinets closed. |
| Mark the positions of the hot and cold faucet handles on the wall or sink so that the same temperature setting can be selected each time. |
| Mark the desired water level on the bathtub with black tape to assist with checking the water level and preventing overfilling. |
| Keep shampoo and other items in easily identified bottles of different shapes so that confusion is minimized if bottle locations are changed. |
Social workers should be contacted to help patients and families find and use community, state and federal resources for the partially sighted. Support groups can provide ongoing help and a forum for sharing feelings, frustrations and solutions.
Final Comment
Age-related macular degeneration is the leading cause of severe vision loss in the elderly. Central vision is lost, but peripheral (ambulatory) vision almost always remains intact. The disease is diagnosed by ophthalmoscopy and can be classified into atrophic and exudative forms. The two currently proven treatments (laser photocoagulation and photodynamic therapy) are effective in only a fraction of eyes with exudative disease. Vision rehabilitation can help patients maximize remaining vision and adapt activities of daily living. Families will need encouragement in providing support and assistance as patients adjust to being partially sighted.