
Am Fam Physician. 2000;62(6):1257-1258
to the editor: Dermatofibrosarcoma protuberans (DFSP) is an uncommon, but not rare, aggressive soft tissue sarcoma arising in the dermis, with a high recurrence rate and a low metastatic potential. The tumor usually presents in young to middle-aged adults (20 to 50 years of age) and is rare in childhood or at birth. Men are affected slightly more frequently than women (57 percent versus 43 percent).1
My interest in this subject was initiated after seeing two cases in my office within the past year. Accurate recognition and referral for appropriate initial treatment is essential to increase the patient's chance of a successful excision and avoidance of recurrence.
Clinically, patients with DFSP present initially with an asymptomatic nodule or plaque ranging in size from a few millimeters to more than 20 cm, most commonly located on the trunk and proximal extremities.2 The tumors may be bluish, red-brown or flesh-colored and slowly infiltrate the surrounding tissues, eventually forming protuberant nodules and causing discomfort. If left untreated, the tumor will enlarge, protrude through the skin and ulcerate. The differential diagnoses include dermatofibroma, keloid, Kaposi's sarcoma and metastatic carcinoma.
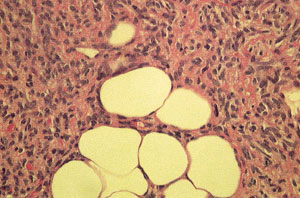
Diagnosis is confirmed through clinical evaluation in conjunction with histopathologic assessment of the lesion. Histologically, DFSP is a dermal tumor composed mainly of spindle cells that are radially oriented in a storiform or cartwheel pattern. Microscopic extension into subcutaneous fat with “honeycomb” entrapment of fat is characteristic. Mitoses are rare.3 A punch biopsy of the patient's lesion shows the dermal spindle cell tumor that infiltrates the subcutaneous fat causing “honeycomb” entrapment (see the accompanying figure). The dermal and subcutaneous infiltrates can extend well away from the primary mass and are responsible for the high recurrence rates following inadequate primary resection.
Surgical excision using wide margin resection or Mohs micrographic surgery (MMS) is the mainstay of treatment for patients with DFSP. Radiotherapy and chemotherapy have a limited role and are usually reserved for metastatic and recurrent disease. Referring the patient for the appropriate initial operative procedure is the main prognostic factor. Patients who underwent primary DFSP excision with undefined or conservative margins had an average recurrence rate of 43 percent; in another study, patients who underwent surgical excision with a wide 5 cm resection margin had a recurrence rate of zero percent.4,5 The literature reports that DFSP lesions treated with MMS had an average recurrence rate of 1.6 percent.4 The consensus is that DFSP can be treated by MMS or surgical resection using at least 3 cm excisional margins. The location of the lesion and cosmetic outcome can best determine the procedure to use.
DFSP is an entity that most family physicians will see during their career. The clinical findings can be easily confused with other skin disorders, contributing to delayed and inappropriate management. Early and accurate recognition, along with appropriate initial treatment, ensures the best outcome and prognosis for the patient.