
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2001;63(1):93-105
A more recent article on Management of Acute Ankle Sprains is available.
Without adequate care, acute ankle trauma can result in chronic joint instability. Use of a standardized protocol enhances the management of ankle sprains. In patients with grades I or II sprains, emphasis should be placed on accurate diagnosis, early use of RICE (rest, ice, compression and elevation), maintenance of range of motion and use of an ankle support. Sprains with complete ligament tears (grade III) may require surgical intervention. [ corrected] Although early motion and mobility are recommended, ligamentous strength does not return until months after an ankle sprain.
The ankle is one of the most common sites for acute musculoskeletal injuries, and sprains account for 75 percent of ankle injuries.1 Acute ankle trauma is responsible for 10 to 30 percent of sports-related injuries in young athletes.2 Each year, an estimated 1 million persons present to physicians with acute ankle injuries.2 More than 40 percent of ankle sprains have the potential to cause chronic problems.3,4
Classification of Ankle Sprains
Ankle sprains range in severity from grade I to grade III (Table 15 and Figure 1). A simpler approach is to divide these injuries into two groups: complicated and uncomplicated. Uncomplicated ankle sprains are treated without surgery. They include injuries not associated with concomitant problems that contraindicate early motion and rehabilitation. Complicated ankle sprains usually require surgical management. Of note, late instability is as common after surgical treatment as after nonoperative treatment of severe ankle ligament injury. Furthermore, late reconstruction is effective in patients initially treated non-operatively.6
| Grade | Signs and symptoms |
|---|---|
| I: partial tear of a ligament | Mild tenderness and swelling |
| Slight or no functional loss (i.e., patient is able to bear weight and ambulate with minimal pain) | |
| No mechanical instability (negative clinical stress examination) | |
| II: incomplete tear of a ligament, with moderate functional impairment | Moderate pain and swelling |
| Mild to moderate ecchymosis | |
| Tenderness over involved structures | |
| Some loss of motion and function (i.e., patient has pain with weight-bearing and ambulation) | |
| Mild to moderate instability (mild unilateral positivity of clinical stress examination) | |
| III: complete tear and loss of integrity of a ligament | Severe swelling (more than 4 cm about the fibula) |
| Severe ecchymosis | |
| Loss of function and motion (i.e., patient is unable to bear weight or ambulate) | |
| Mechanical instability (moderate to severe positivity of clinical stress examination) |
Pathoanatomy and Mechanisms of Injury
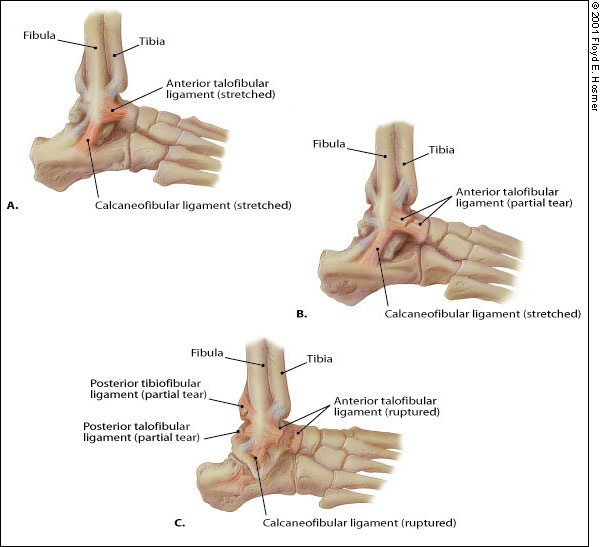
The most common mechanism of injury in ankle sprains is a combination of plantar flexion and inversion. The lateral stabilizing ligaments, which include the anterior talofibular, calcaneofibular and posterior talofibular ligaments, are most often damaged. The anterior talofibular ligament is the most easily injured. Concomitant injury to this ligament and the calcaneofibular ligament can result in appreciable instability.5 The posterior talofibular ligament is the strongest of the lateral complex and is rarely injured in an inversion sprain.5,7


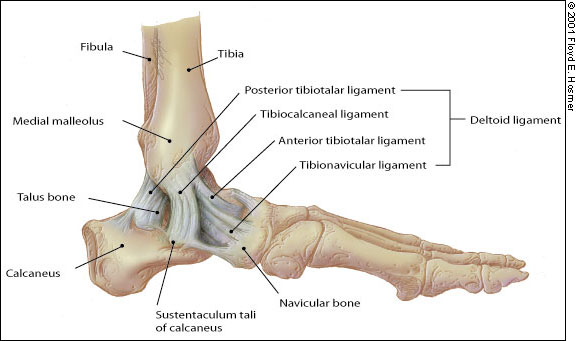
Medial ankle stability is provided by the strong deltoid ligament, the anterior tibiofibular ligament and the bony mortise (Figure 4). Because of the bony articulation between the medial malleolus and the talus, medial ankle sprains are less common than lateral sprains. In medial ankle sprains, the mechanism of injury is excessive eversion and dorsiflexion.
Diagnosis
Ankle trauma is evaluated with a careful history (situation and mechanism of injury, previous injury to the joint, etc.) and a careful physical examination (for example, inspection, palpation, weight-bearing status, special tests).
Gross deformity should not occur with an ankle sprain, although severe swelling can give the impression of deformity. The entire length of the tibia and fibula should be palpated to detect fracture of the proximal fibula (Maisonneuve fracture), which may be associated with syndesmosis injury.
Tenderness along the base of the fifth metatarsal may indicate an avulsion of the peroneal brevis tendon.
Palpable pain and effusion along the talocrural joint line should raise suspicion of an osteochondral talar dome lesion. This lesion results from direct trauma between the talus and fibula (anterolateral lesion) or between the posteromedial talus and tibia (posteromedial lesion). A talar dome lesion may not be apparent on radiographs until two to four weeks after the injury.9
Lack of swelling with an eversion or hyperdorsiflexion mechanism of injury, along with tenderness at the distal tibiofibular joint, may indicate a syndesmosis sprain.6
Special tests are useful to further substantiate the presence of a syndesmosis sprain. A “squeeze test,” performed by compressing the fibula and tibia at the midcalf, is considered positive if pain is elicited distally over the tibia and fibular syndesmosis. An “external rotation test” is also recommended to identify a syndesmosis sprain. This test is performed with the patient's knee resting over the edge of the table. The physician stabilizes the leg proximal to the ankle joint while grasping the plantar aspect of the foot and rotating the foot externally relative to the tibia. If pain occurs with this maneuver, the test is positive.10
RADIOLOGY
The Ottawa ankle rules can be used to determine when radiographic studies are indicated in the patient with ankle trauma (Figure 5).11 According to these rules, radiographs should be obtained to rule out fracture when a patient presents (within 10 days of injury) with bone tenderness in the posterior half of the lower 6 cm (2.5 in) of the fibula or tibia or an inability to bear weight immediately after the injury and in the emergency department (or physician's office). Bone tenderness over the navicular bone or base of the fifth metatarsal is an indication for radiographs to rule out fracture of the foot.
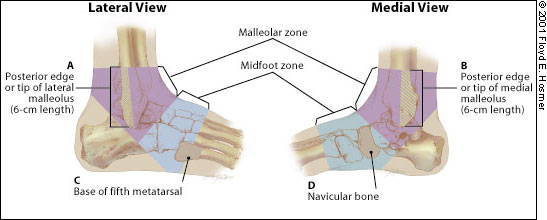
Implementation of the Ottawa rules has reduced unnecessary radiography, decreased waiting time for patients and lowered diagnostic costs. These rules have been reported to have a sensitivity of 100 percent for the detection of malleolar fractures (95 percent confidence interval [CI]; range: 82 to 100 percent) and a sensitivity of 100 percent for the detection of midfoot fractures (95 percent CI; range: 95 to 100 percent).11
If indicated on the basis of the Ottawa ankle rules, anteroposterior, lateral and mortise radiographs should be obtained after the initial physical examination. The mortise projection is an anteroposterior view obtained with the leg internally rotated 15 to 20 degrees so that the x-ray beam is nearly perpendicular to the intermalleolar line. The radiographs of an uncomplicated ankle sprain should appear normal, or they may show some lateral tilt of the talus on the anteroposterior or mortise projection.
Radiographs may reveal malleolar fractures, talar dome fractures or disruption of the ankle syndesmosis. Any of these findings should prompt referral to an orthopedic specialist. Talar dome lesions occur in 6.8 to 22.0 percent of ankle sprains, but they can be missed during the initial assessment.9,12 It may take weeks for these transchondral fractures to manifest the bony changes of osteonecrosis (seen subjacent to the site of injury).
Tarsal navicular stress fractures also present a diagnostic challenge. Instead of localized pain, patients with these fractures may have diffuse, vague pain along the medial longitudinal arch or dorsum of the foot.13 This stress reaction may be misdiagnosed as medial longitudinal arch pain or plantar fasciitis.
For ankle sprains that remain symptomatic for more than six weeks, computed tomographic (CT) scanning or magnetic resonance imaging (MRI) should be considered to rule out talar dome lesions. CT or MRI studies should also be considered for ankle injuries that involve crepitus, catching or locking, because these symptoms may be associated with a displaced osteochondral fragment.
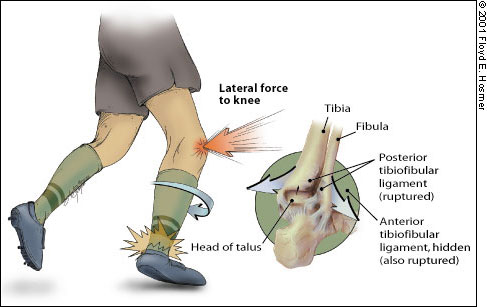
MRI studies may be helpful in identifying syndesmosis sprains and peroneal tendon involvement.13 Injury to the tibiofibular syndesmosis ligaments, which bind together the distal ends of the tibia and fibula, is commonly referred to as a high ankle sprain. Although this injury accounts for only about 10 percent of ankle sprains, it represents a more disabling problem and requires different treatment than common ankle sprains.14 The mechanism of injury is excessive dorsiflexion and eversion of the ankle joint with internal rotation of the tibia (Figure 6). Radiographically, a syndesmosis sprain manifests as widening of the tibiofibular “clear space” to greater than 6 mm15 (Figure 716). Rarely, the syndesmosis is frankly disrupted, and the injury is obvious.

INDICATIONS FOR REFERRAL
The history, physical examination and radiologic evaluation should be adequate for determining whether orthopedic referral is indicated. Specific indications for referral include the following: fracture or dislocation, neurovascular compromise, tendon rupture or subluxation, a wound that penetrates the joint, mechanical “locking” of the joint and injury to the syndesmosis. Patients with symptoms out of proportion to the degree of trauma, or in whom the diagnosis is uncertain, should probably also have at least a diagnostic consultation. Once complicating features have been excluded, initial management and functional rehabilitation of the ankle sprain can be instituted.
Initial Management
The family physician can successfully manage uncomplicated ankle sprains. Because increased swelling is directly associated with loss of range of motion in the ankle joint, the initial goals are to prevent swelling and maintain range of motion.
Early management includes RICE (rest, ice, compression and elevation). Cryotherapy should be used immediately after the injury.17 Heat should not be applied to an acutely injured ankle joint because it encourages swelling and inflammation through hyperemia.
Crushed ice in a plastic bag may be applied to the medial and lateral ankle over a thin layer of cloth. Alternatively, the foot and ankle may be cooled by immersion in water at a temperature of approximately 12.7°C (55°F). The foot and ankle should be cooled for approximately 20 minutes every two to three hours for the first 48 hours, or until edema and inflammation have stabilized. Benefits of cryotherapy include a decrease in metabolism that limits secondary hypoxic injury.17
While cold therapy is being used, exercises should be initiated to maintain range of motion and assist lymphatic drainage.
To milk edema fluid away from the injured tissues, the ankle should be wrapped with an elastic bandage. The bandaging should start just proximal to the toes and extend above the level of maximal calf circumference. A piece of felt cut in the shape of a “U” and applied around the lateral malleolus increases hydrostatic pressure to an area that is prone to increased swelling.
Next, the injured extremity should be elevated 15 to 25 cm (6 to 10 in) above the level of the heart to facilitate venous and lymphatic drainage until the swelling has begun to resolve.17 Nonsteroidal anti-inflammatory drugs are preferable to narcotics for pain relief.
In most patients, the use of two properly fitted crutches should be considered during the initial, most painful period after injury. Weight-bearing should occur as tolerated. Gait should be normal and nonantalgic, and can be advanced as tolerated.
A painful, edematous sprained ankle tends to stiffen in a plantar-flexed, slightly inverted position. Unless this stiffening is prevented, rehabilitation has to be delayed until range of motion is slowly regained. To facilitate early rehabilitation and cryotherapy, an easily removable device, such as a plastic ankle-foot orthosis or simple plaster posterior splint, may be employed for immobilization. Circumferential casting generally is not recommended. Air-filled or gel-filled ankle braces that restrict inversion-eversion and allow limited plantar flexion-dorsiflexion facilitate rehabilitation.18
Functional Rehabilitation
The importance of proper rehabilitation after an ankle sprain cannot be overemphasized, especially when the debilitating consequences of decreased range of motion, persistent pain and swelling, and chronic joint instability are considered. After initial acute treatment, a rehabilitation regimen is pivotal in speeding return to activity and preventing chronic instability. In a recent military series19 it was found that lack of rehabilitation of ankle sprains delayed return to duty for several months.
Prolonged immobilization of ankle sprains is a common treatment error.20,21 Functional stress stimulates the incorporation of stronger replacement collagen.20 Functional rehabilitation begins on the day of injury and continues until pain-free gait and activity are attained. The four components of rehabilitation are range-of-motion rehabilitation, progressive muscle-strengthening exercises, proprioceptive training and activity-specific training.
Ankle joint stability is a prerequisite to the institution of functional rehabilitation. Because grades I and II ankle sprains are considered stable, functional rehabilitation can begin immediately.
RANGE OF MOTION
| Component | Procedure | Duration and frequency | Comments | |
|---|---|---|---|---|
| Range of motion | ||||
| Achilles tendon stretch, nonweight-bearing | Use a towel to pull foot toward face. | Pain-free stretch for 15 to 30 seconds; perform five repetitions; repeat three to five times a day. | Maintain extremity in a nongravity position with compression. | |
| Achilles tendon stretch, weight-bearing | Stand with heel on floor and bend at knees. | Pain-free stretch for 15 to 30 seconds; perform five repetitions; repeat three to five times a day. | ||
| Alphabet exercises performed | Move ankle in multiple planes of motion by drawing letters of alphabet (lower case and upper case). | Repeat four to five times a day. | Exercises can be in conjunction with cold therapy. | |
| Muscle strengthening | ||||
| Isometric exercises | Resistance can be provided by immovable object (wall or floor) or contralateral foot. | For each exercise, hold 5 seconds; do 10 repetitions; repeat three times a day. | Strengthening exercises should only be done in positions that do not cause pain. | |
| Plantar flexion | Push foot downward (away from head). | |||
| Dorsiflexion | Pull foot upward (toward head). | |||
| Inversion | Push foot inward (toward midline of body). | |||
| Eversion | Push foot outward (away from midline of body). | |||
| Isotonic exercises | Resistance can be provided by contralateral foot, rubber tubing or weights. | For each exercise, hold 1 second for concentric component and perform eccentric component over 4 seconds; do three sets of 10 repetitions; repeat two times a day. | Emphasis is placed on the eccentric component; exercises should be performed slowly and under control. | |
| Plantar flexion | Push foot downward (away from head). | |||
| Dorsiflexion | Pull foot upward (toward head). | |||
| Inversion | Push foot inward (toward midline of body). | |||
| Eversion | Push foot outward (away from midline of body). | |||
| Toe curls and marble pickups | Place foot on a towel; then curl toes, moving the towel toward body. | Two sets of 10 repetitions; repeat two times a day. | Toe curls can be done throughout the day, at work or at home. | |
| Use toes to pick up marbles or other small object. | ||||
| Toe raises, heel walks and toe walks | Lift body by rising up on toes. Walk forward and backward on toes and heels. | Three sets of 10 repetitions; repeat two times a day; progress walking as tolerated. | Strengthening can occur from using the body as resistance in weight-bearing position. | |

MUSCLE-STRENGTHENING EXERCISES
Once range of motion is attained, and swelling and pain are controlled, the patient is ready to progress to the strengthening phase of rehabilitation. Strengthening of weakened muscles is essential to rapid recovery and important in preventing reinjury.22 Exercises should focus on the conditioning of peroneal muscles, because insufficient strength in this muscle group has been associated with ankle instability and recurrent injury.23
Strengthening begins with isometric exercises performed against an immovable object in four directions of ankle movement. The patient then progresses to dynamic resistive exercises using ankle weights, resistance bands or elastic tubing (Figure 9).

Resistance exercises should be performed with an emphasis on eccentric contraction.23 The patient is instructed to pause one second between the concentric and eccentric phases of exercise and to perform the eccentric component over a four-second period. “Concentric” contraction refers to the active shortening of muscle with resultant lengthening of the resistance band, whereas “eccentric” contraction involves the passive lengthening of muscle by the elastic pull of the band.
Toe raises (Figure 10), heel walks and toe walks may also be attempted to regain strength and coordination.

PROPRIOCEPTIVE TRAINING
As the patient achieves full weight-bearing without pain, proprioceptive training is initiated for the recovery of balance and postural control (Table 3). Various devices have been specifically designed for this phase of rehabilitation. Use of these devices in concert with a series of progressive drills can effectively return patients to a high functional level.24,25
| Component | Procedure | Duration and frequency | Comments |
|---|---|---|---|
| Proprioceptive training | |||
| Circular wobble board | In sitting position, rotate board clockwise and counterclockwise using one foot and then both feet; in standing position, rotate board using one leg and then both legs. | Do five to 10 repetitions; repeat set two times a day. | Wobble board exercises can be performed with eyes open or closed and with or without resistance. |
| Walking on different surfaces | Walk in normal or heel-to-toe fashion over various surfaces; progress from hard, flat floor to uneven surface. | Walk 50 feet two times a day. | Walking exercises can be performed with eyes open or closed and with or without resistance. |
| Training for return to activity | |||
| Walk-jog | Do 50 percent walking and 50 percent jogging in forward direction and backward direction; progress to jogging; jog in a pattern (e.g., circle, figure-eight). | Increase distance in increments of one-eighth mile. | Increase intensity and incorporate activity-specific training.* |
| Jog-run | Do 50 percent jogging and 50 percent running in forward and backward directions; run in a pattern (e.g., circle, figure-eight). | Increase distance in increments of one-eighth mile. | Increase intensity and incorporate activity-specific training.* |
The simplest device for proprioceptive training is the wobble board, a small discoid platform attached to a hemispheric base.7 The patient is instructed to stand on the wobble board on one foot and shift his or her weight, causing the edge of the wobble board to move in a continuous circular path (Figure 11). Training can be advanced by having the patient perform this maneuver at different heights and with closed eyes.

TRAINING FOR RETURN TO ACTIVITY
When walking a specified distance is no longer limited by pain, the patient may progress to a regimen of 50 percent walking and 50 percent jogging. When this can be done without pain, jogging eventually progresses to forward, backward and pattern running. Circles and figure-eights are commonly employed for pattern running. Although these routines are time-consuming, they represent the final phase of ankle joint rehabilitation, and completion of the program is essential for the recovery of ankle stability.
A patient who will be returning to sports participation may require additional athletic therapy. This component of the rehabilitation process should be supervised by a certified athletic trainer or sports physical therapist who is familiar with the physical demands of the patient's sport. Use of a stabilizing orthotic device or tape, with subsequent weaning, may be recommended during the early period of activity-specific training.