
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2001;63(3):467-475
See patient information handout on plantar fasciitis, written by the authors of this article.
Plantar fasciitis is a common cause of heel pain in adults. The disorder classically presents with pain that is particularly severe with the first few steps taken in the morning. In general, plantar fasciitis is a self-limited condition. However, symptoms usually resolve more quickly when the interval between the onset of symptoms and the onset of treatment is shorter. Many treatment options exist, including rest, stretching, strengthening, change of shoes, arch supports, orthotics, night splints, anti-inflammatory agents and surgery. Usually, plantar fasciitis can be treated successfully by tailoring treatment to an individual's risk factors and preferences.
Plantar fasciitis is a common cause of heel pain in adults. The pain is usually caused by collagen degeneration (which is sometimes misnamed “chronic inflammation”) at the origin of the plantar fascia at the medial tubercle of the calcaneus. This degeneration is similar to the chronic necrosis of tendonosis, which features loss of collagen continuity, increases in ground substance (matrix of connective tissue) and vascularity, and the presence of fibro-blasts rather than the inflammatory cells usually seen with the acute inflammation of tendonitis.1 The cause of the degeneration is repetitive microtears of the plantar fascia that overcome the body's ability to repair itself.
The classic sign of plantar fasciitis is that the worst pain occurs with the first few steps in the morning, but not every patient will have this symptom. Patients often notice pain at the beginning of activity that lessens or resolves as they warm up. The pain may also occur with prolonged standing and is sometimes accompanied by stiffness. In more severe cases, the pain will also worsen toward the end of the day.
The plantar fascia is a thickened fibrous aponeurosis that originates from the medial tubercle of the calcaneus and runs forward to form the longitudinal foot arch. The function of the plantar fascia is to provide static support of the longitudinal arch and dynamic shock absorption. Individuals with pes planus (low arches or flat feet) or pes cavus (high arches) are at increased risk for developing plantar fasciitis.
Other anatomic risks include overpronation, discrepancy in leg length, excessive lateral tibial torsion and excessive femoral anteversion. Functional risk factors include tightness and weakness in the gastrocnemius, soleus, Achilles tendon and intrinsic foot muscles. However, overuse rather than anatomy is the most common cause of plantar fasciitis in athletes. A history of an increase in weight-bearing activities is common, especially those involving running, which causes microtrauma to the plantar fascia and exceeds the body's capacity to recover. Plantar fasciitis also occurs in elderly adults. In these patients, the problem is usually more biomechanical, often related to poor intrinsic muscle strength and poor force attenuation secondary to acquired flat feet and compounded by a decrease in the body's healing capacity.
On examination, the patient usually has a point of maximal tenderness at the anteromedial region of the calcaneus. The patient may also have pain along the proximal plantar fascia. The pain may be exacerbated by passive dorsiflexion of the toes or by having the patient stand on the tips of the toes.
Diagnostic testing is rarely indicated for the initial evaluation and treatment of plantar fasciitis. Plantar fasciitis is often called “heel spurs,” although this terminology is somewhat of a misnomer because 15 to 25 percent of the general population without symptoms have heel spurs and many symptomatic individuals do not.2 Heel spurs are bony osteophytes that can be visualized on the anterior calcaneus on radiography. However, diagnostic testing is indicated in cases of atypical plantar fasciitis, in patients with heel pain that is suspicious for other causes (Table 1) or in patients who are not responding to appropriate treatment.
| Disease or injury | Differentiating clinical features | |
|---|---|---|
| Neurologic causes (entrapment syndromes) | Radiating burning pain, numbness and tingling, especially at night | |
| Tarsal tunnel syndrome | Diffuse symptoms over plantar surface | |
| Medial calcaneal branch of the posterior tibial nerve entrapment | Medial and plantar heel symptoms | |
| Abductor digiti quinti nerve entrapment | Burning pain in heel pad area | |
| Skeletal causes | Bony point tenderness | |
| Calcaneal stress fracture activity | Pain with weight-bearing; worsens with prolonged weight-bearing | |
| Paget's disease | Bowed tibias, kyphosis, headaches | |
| Tumor | Deep bone pain; constitutional symptoms late in the course | |
| Calcaneal apophysitis (Sever's disease) | Posterior heel pain in adolescents | |
| Soft tissue causes | ||
| Fat pad syndrome | Atrophy of heel pad | |
| Heel bruise | History of acute impact injury | |
| Bursitis | Usually retrocalcaneal; swelling and erythema of posterior heel | |
| Plantar fascia rupture | Sudden acute, knife-like pain, ecchymosis | |
| Tendonitis | Pain with resisted motions | |
| Plantar fasciitis | See text. | |
Treatment
In general, plantar fasciitis is a self-limiting condition. Unfortunately, the time until resolution is often six to 18 months, which can lead to frustration for patients and physicians. Rest was cited by 25 percent of patients with plantar fasciitis in one study as the treatment that worked best.3 Athletes, active adults and persons whose occupations require lots of walking may not be compliant if instructed to stop all activity. Many sports medicine physicians have found that outlining a plan of “relative rest” that substitutes alternative forms of activity for activities that aggravate the symptoms will increase the chance of compliance with the treatment plan.4
It is equally important to correct the problems that place individuals at risk for plantar fasciitis, such as increased amount of weight-bearing activity, increased intensity of activity, hard walking/running surfaces and worn shoes. Early recognition and treatment usually lead to a shorter course of treatment as well as increased probability of success with conservative treatment measures.3,5,6
STRETCHING AND STRENGTHENING
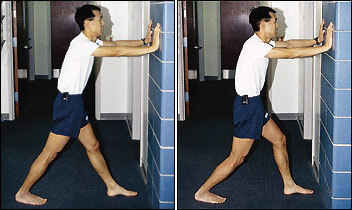
Stretching and strengthening programs play an important role in the treatment of plantar fasciitis and can correct functional risk factors such as tightness of the gastrocsoleus complex and weakness of the intrinsic foot muscles. Increasing flexibility of the calf muscles is particularly important. Frequently used stretching techniques include wall stretches (Figure 1) and curb or stair stretches (Figure 2).

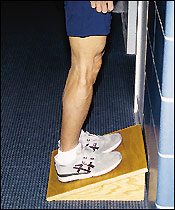
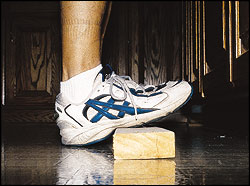
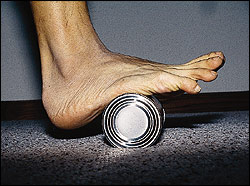
Other effective techniques include use of a slant board (Figure 3) or placing a two-inch × four-inch piece of wood (Figure 4) in areas where the patient stands for a prolonged time (e.g., workplaces, kitchen or stoves) to use in stretching the calf. Dynamic stretches such as rolling the foot arch over a 15-oz size can or a tennis ball are also useful (Figure 5). Cross-friction massage above the plantar fascia (Figure 6) and towel stretching (Figure 7) may be done before getting out of bed and serve to stretch the plantar fascia.


In one study,3 83 percent of patients involved in stretching programs were successfully treated, and 29 percent of patients in the study cited stretching as the treatment that had helped the most compared with use of orthotics, nonsteroidal anti-inflammatory drugs (NSAIDs), ice, steroid injection, heat, heel cups, night splints, walking, plantar strapping and shoe changes.3
Strengthening programs should focus on intrinsic muscles of the foot. Exercises used include towel curls and toe taps. Exercises such as picking up marbles and coins with the toes are also useful. To do a towel curl, the patient sits with the foot flat on the end of a towel placed on a smooth surface. Keeping the heel on the floor, the towel is pulled toward the body by curling the towel with the toes. To do toe taps, all the toes are lifted off the floor and, keeping the heel on the floor and the outside four toes in the air, the big toe is tapped to the floor repetitively. Next, the process is reversed, and the outside four toes are repetitively tapped to the floor while keeping the big toe in the air.
In another study,6 strengthening programs were cited as the most helpful treatment by 34.9 percent of the subjects, compared with exercise, night splints, orthotics, heel cups, NSAIDs, steroid injection or surgery.
SHOES
A change to properly fitting, appropriate shoes may be useful in some patients. Some individuals wear shoes that are too small, which can exacerbate many types of foot pain.7 Patients often find that wearing shoes with thicker, well-cushioned midsoles, usually made of a material like high-density ethylene vinyl acetate (such as is found in many running shoes), decreases the pain associated with long periods of walking or standing. Studies5 have shown that with age, running shoes lose a significant portion of their shock absorption. Thus, simply getting a new pair of shoes may be helpful in decreasing pain.
For individuals with flat feet, motion control shoes or shoes with better longitudinal arch support may decrease the pain associated with long periods of walking or standing.5 Motion control shoes usually have the following characteristics: a straight last, board or combination lasted construction, an external heel counter, a wider flare and extra medial support.5 A change in shoes was cited by 14 percent of patients with plantar fasciitis as the treatment that worked best for them.3
ARCH SUPPORTS AND ORTHOTICS
Patients with low arches theoretically have a decreased ability to absorb the forces generated by the impact of foot strike.5 The three most commonly used mechanical corrections are arch taping, over-the-counter arch supports and custom orthotics. Arch taping and orthotics were found to be significantly better than use of NSAIDs, cortisone injection or heel cups in one randomized treatment study.8 Arch taping was cited by 2 percent of patients as the treatment that worked best for plantar fasciitis in another study.3 A single taping treatment is much less expensive than an over-the-counter arch support or an orthotic.
Taping provides only transient support, with studies9,10 showing that as little as 24 minutes of activity can decrease the effectiveness of taping significantly. Arch taping can be used as definitive treatment or as a trial to determine if the expense of arch supports or orthotics is worth the benefit. Taping may be more cost effective for acute onset of plantar fasciitis, and over-the-counter arch supports and orthotics may be more cost-effective for chronic or recurrent cases of plantar fasciitis and for prevention of injuries. In athletes, arches must be retaped at least for every new game or practice session, whereas an over-the-counter arch support usually lasts a full sports season and a custom orthotic usually lasts for many seasons.
Over-the-counter arch supports may be useful in patients with acute plantar fasciitis and mild pes planus. The support provided by over-the-counter arch supports is highly variable and depends on the material used to make the support. In general, patients should try to find the most dense material that is soft enough to be comfortable to walk on. Over-the-counter arch supports are especially useful in the treatment of adolescents whose rapid foot growth may require a new pair of arch supports once or more per season.
Custom orthotics are usually made by taking a plaster cast or an impression of the individual's foot and then constructing an insert specifically designed to control biomechanical risk factors such as pes planus, valgus heel alignment and discrepancies in leg length. For patients with plantar fasciitis, the most common prescription is for semi-rigid, three-quarters to full-length orthotics with longitudinal arch support. Two important characteristics for successful treatment of plantar fasciitis with orthotics are the need to control over-pronation and metatarsal head motion, especially of the first metatarsal head.11 In one study,3 orthotics were cited by 27 percent of patients as the best treatment. The main disadvantage of orthotics is the cost, which may range from $75 to $300 or more and which is frequently not covered by health insurance.
Heel cups are used to decrease the impact on the calcaneus and to theoretically decrease the tension on the plantar fascia by elevating the heel on a soft cushion. Although heel cups have been found to be useful by some physicians and patients,6 in our experience they are more useful in treating patients with fat pad syndrome and heel bruises than patients with plantar fasciitis. In a survey of 411 patients with plantar fasciitis,12 heel cups were ranked as the least effective of 11 different treatments.
NIGHT SPLINTS
Night splints usually are designed to keep a person's ankle in a neutral position overnight. Most individuals naturally sleep with the feet plantar-flexed, a position that causes the plantar fascia to be in a foreshortened position. A night dorsiflexion splint allows passive stretching of the calf and the plantar fascia during sleep. Theoretically, it also allows any healing to take place while the plantar fascia is in an elongated position, thus creating less tension with the first step in the morning. A night splint can be molded from plaster or fiberglass casting material or may be a prefabricated, commercially produced plastic brace (Figure 8).

Several studies13,14 have shown that use of night splints has resulted in improvement in approximately 80 percent of patients using night splints. Other studies15,16 found that night splints were especially useful in individuals who had symptoms of plantar fasciitis that had been present for more than 12 months. Night splints were cited as the best treatment by approximately one third of the patients with plantar fasciitis who tried them.3,6 Disadvantages of night splints include mild discomfort, which may interfere with the patient's or a bed partner's ability to sleep.
ANTI-INFLAMMATORY AGENTS
Anti-inflammatory agents used in the treatment of plantar fasciitis include ice, NSAIDs, iontophoresis and cortisone injections. Ice is applied in the treatment of plantar fasciitis by ice massage, ice bath or in an ice pack. For ice massage, the patient freezes water in a small paper or foam cup, then rubs the ice over the painful heel using a circular motion and moderate pressure for five to 10 minutes. To use an ice bath, a shallow pan is filled with water and ice, and the heel is allowed to soak for 10 to 15 minutes. Patients should use neoprene toe covers or keep the toes out of the ice water to prevent injuries associated with exposure to the cold. Crushed ice in a plastic bag wrapped in a towel makes the best ice pack, because it can be molded to the foot and increase the contact area. A good alternative is the use of a bag of prepackaged frozen corn wrapped in a towel. Ice packs are usually used for 15 to 20 minutes. Icing is usually done after completing exercise, stretching, strengthening and after a day's work.
The use of anti-inflammatory drugs in chronic inflammatory diseases is somewhat controversial.1,17 Eleven percent of the patients in one study3 cited NSAIDs as the treatment that worked best for them, and 79 percent of the patients using NSAIDs were in the successfully treated group.3 Advantages of NSAIDs are the acceptability of the use of an oral medication as a treatment modality by many patients, the convenience and ease of administration, and the acceptance by medical insurance. Disadvantages of NSAIDs are many, including the risk of gastrointestinal bleeding, gastric pain and renal damage.18
IONTOPHORESIS
Iontophoresis is the use of electric impulses from a low-voltage galvanic current stimulation unit to drive topical corticosteroids into soft tissue structures. One study19 found that the use of iontophoresis resulted in significant improvement after two weeks but no long-term differences at six weeks. The major disadvantages of iontophoresis are cost and time because, to be effective, it must be administered by an athletic trainer or physical therapist at least two to three times per week. Thus, iontophoresis use is probably best reserved for the treatment of elite athletes and of laborers with acute plantar fasciitis whose symptoms are preventing them from working.
CORTICOSTEROID INJECTIONS
Corticosteroid injections, like iontophoresis, have the greatest benefit if administered early in the course of the disease but, because of the associated risks, they are usually reserved for recalcitrant cases. A plain radiograph of the foot or calcaneus should always be obtained before injecting steroids to ensure that the cause of pain is not a tumor. Steroids can be injected via plantar or medial approaches with or without ultrasound guidance. Studies20,21 have found steroid treatments to have a success rate of 70 percent or better.
Potential risks include rupture of the plantar fascia and fat pad atrophy.22,23 Rupture of the plantar fascia was found in almost 10 percent of patients after plantar fascia injection in one series.22 Long-term sequelae of plantar fascia rupture were found in approximately one half of the patients with plantar fascia rupture, with longitudinal arch strain accounting for more than one half of the chronic complications.22,23 On the other hand, one author24 found that most individuals with rupture of the plantar fascia had resolution of symptoms with rest and rehabilitation.
SURGERY
In cases that do not respond to any conservative treatment, surgical release of the plantar fascia may be considered. Plantar fasciotomy may be performed using open, endoscopic or radiofrequency lesioning techniques. Overall, the success rate of surgical release is 70 to 90 percent in patients with plantar fasciitis.24–27 Potential risk factors include flattening of the longitudinal arch and heel hypoesthesia as well as the potential complications associated with rupture of the plantar fascia and complications related to anesthesia.
TYPICAL TREATMENT PLAN
In general, we start by correcting training errors. This usually requires relative rest, the use of ice after activities, and an evaluation of the patient's shoes and activities. Next, we try correction of biomechanical factors with a stretching and strengthening program. If the patient still has no improvement, we consider night splints and orthotics. Finally, all other treatment options are considered. Non-steroidal anti-inflammatory medications are considered throughout the treatment course, although we explain to the patient that this medicine is being used primarily for pain control and not to treat the underlying problem.