
Am Fam Physician. 2001;64(7):1266-1267
The decision to discontinue cardiopulmonary resuscitation (CPR) is a difficult one for physicians. Pre-arrest and intra-arrest factors associated with increased risk of unsuccessful CPR include hypotension, renal failure, pneumonia, low functional status, metastatic cancer, prolonged duration of CPR and initial cardiac rhythms other than pulseless ventricular tachycardia or ventricular fibrillation. These decision aids, however, are complicated, difficult to administer at bedside, and poorly validated in distinct populations, and have proved unable to definitely identify patients with no hope of survival. Van Walraven and associates attempted to validate a clinical decision aid in predicting survival to discharge following cardiac arrest and attempted CPR in hospitalized patients.
The authors had determined in a previous study that resuscitated patients likely to be discharged from the hospital were those with (1) a witnessed arrest, (2) an initial rhythm of ventricular tachycardia or fibrillation, or (3) a pulse within the first 10 minutes of beginning chest compressions. They proposed that resuscitative efforts might safely be withdrawn on patients who did not satisfy this decision criteria, since none of these patients was discharged from the hospital. This validation study, a secondary analysis of a resuscitation registry at a major medical center, included all hospital cardiac arrests (with the exception of those in the neonatal intensive care unit or operating room) that occurred between 1987 and 1996. All resuscitations in the hospital registry were eligible for this study with the exception of patients younger than 16 years and patients undergoing surgery at the time of arrest. The decision aid was applied to patients who were pulse-less at the start of resuscitation and further excluded patients in whom the initial rhythm was pulseless ventricular tachycardia, ventricular fibrillation, pulseless electrical activity or asystole.
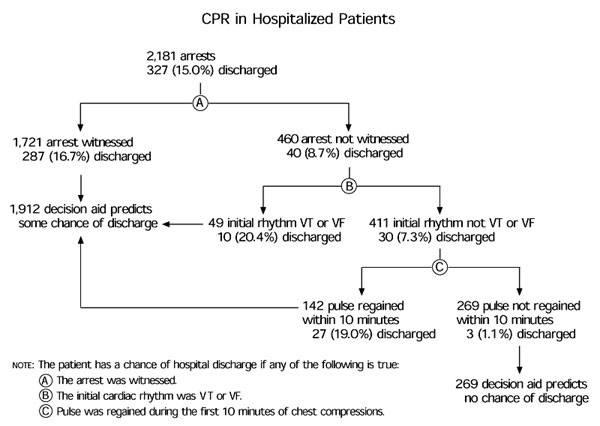
The accompanying figure illustrates how the decision aid identified patients who would be discharged from the hospital. Of the 327 resuscitations, patients in 324 cases satisfied the decision aids and were predicted to survive to hospital discharge (sensitivity: 99.1 percent). In 269 resuscitations, patients did not satisfy the decision aid and were predicted to have no chance of being discharged. The mean resuscitation duration in the latter group of patients was 22.6 minutes, and spontaneous circulation was achieved in 53 patients who were transferred to the intensive care unit. Of these 53 patients, 26 lived for at least 24 hours but died later during hospitalization. Of the 269 predicted to not survive to discharge, all but three (1.1 percent) died following arrest.
The authors conclude that their decision aid, in addition to other clinical factors, can help physicians determine which patients are unlikely to benefit from ongoing CPR.