
A more recent article on groin pain and injuries is available.
Am Fam Physician. 2001;64(8):1405-1415
Groin injuries comprise 2 to 5 percent of all sports injuries. Early diagnosis and proper treatment are important to prevent these injuries from becoming chronic and potentially career-limiting. Adductor strains and osteitis pubis are the most common musculoskeletal causes of groin pain in athletes. These two conditions are often difficult to distinguish. Other etiologies of groin pain include sports hernia, groin disruption, iliopsoas bursitis, stress fractures, avulsion fractures, nerve compression and snapping hip syndrome.
The diagnosis of groin pain in athletes is difficult because the anatomy of the region is complex and because two or more injuries often coexist. Intra-abdominal pathology, genitourinary abnormalities, referred lumbosacral pain and hip joint disorders (e.g., arthritis, synovitis, avascular necrosis) must first be excluded. Once these conditions are ruled out, other musculoskeletal conditions involving the groin may be pursued (Table 1).
Between 2 and 5 percent of all sports injuries occur in the groin area.1,2 These injuries are more prevalent in persons who participate in sports such as ice hockey, fencing, handball, cross country skiing, hurdling and high jumping, and may comprise as many as 5 to 7 percent of all injuries in soccer players.3 The diagnosis is often frustrating for both the athlete and the physician, and remains unclear in approximately 30 percent of cases.4 Factors that complicate the diagnosis include the complex anatomy of the region and the frequent coexistence of two or more disorders. In one study5 of 21 patients with groin pain, 19 patients were found to have two or more disorders. The investigators concluded that groin pain in athletes is complex and can be difficult to evaluate even by experienced physicians.
| Intra-abdominal disorders (e.g., aneurysm, appendicitis, diverticulosis, inflammatory bowel disease) |
| Genitourinary abnormalities (e.g., urinary tract infection, lymphadenitis, prostatitis, scrotal and testicular abnormalities, gynecologic abnormalities, nephrolithiasis) |
| Referred lumbosacral pain (e.g., lumbar disc disease) |
| Hip joint disorders (e.g., Legg-Calvé-Perthes disease, synovitis, slipped femoral capital epiphysis in younger patients and osteochondritis disse-cans of femoral head, avascular necrosis of the femoral head, osteoarthritis, acetabular labral tears) |
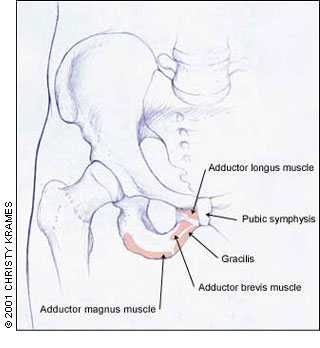
The ability to visualize the anatomy of the groin area is important for both the physical examination and the differential diagnosis. The anatomy of the groin region is illustrated in Figure 1.
Adductor Strains
These strains are usually easily diagnosed on physical examination with pain on palpation of the involved muscle and pain on adduction against resistance.6 They must, however, be distinguished from osteitis pubis and “sports hernias,” which can present with pain in similar locations.
Although the diagnosis is usually made clinically, radiographs can be helpful in excluding fractures or avulsions.6 If the diagnosis is in question, magnetic resonance imaging (MRI) can be used to confirm muscle strain or tears, and partial and complete tendon tears. Ultrasound is useful for diagnosing muscle and tendon tears, but not muscle strains.7 The most common site of strain is the musculotendinous junction of the adductor longus or gracilis. Complete avulsions of these tendons also occur, but much less frequently.
Once the diagnosis of adductor strain has been established, three questions must be considered. First, are there biomechanical abnormalities that may predispose to injury? Foot and lower leg malalignment, muscular imbalances, leg length discrepancy, gait or sport-specific motion abnormalities can all theoretically place abnormal loads on the adductors. Although controlled clinical studies demonstrating a causal relationship between biomechanical abnormalities and adductor strains have not been conducted, many physicians specializing in sports medicine believe that these are important contributing factors.6 If present, these abnormalities should be evaluated and corrected if possible.
Second, what is the location of the tear? This has important therapeutic and prognostic implications. If an acute tear occurs at the musculotendinous junction, a relatively aggressive approach to rehabilitative treatment can be undertaken. When an acute partial tear occurs at the tendinous insertion of the adductors into the pubic bone, a period of rest must be completed before pain-free physical therapy is possible.8
Third, what is the chronicity of the symptoms? Athletes often do not recall an acute inciting incident and complain instead of pain of an insidious onset. These athletes are difficult to treat because they remain able to play their sports (at least for a while) after a good warm-up and are not motivated to take time off and undergo proper rehabilitation.
Although few controlled studies of the treatment of adductor strains exist in the literature, most clinical experience dictates that acute treatment include physical therapy modalities (i.e., rest, ice, compression, elevation) that help prevent further injury and inflammation. Following this, the goal of therapy should be restoration of range of motion and prevention of atrophy. Finally, the patient should regain strength, flexibility and endurance.6 When the athlete has regained at least 70 percent of his or her strength and pain-free full range of motion, a return to sport may be allowed.9 This return may take four to eight weeks following an acute musculotendinous strain and up to six months for chronic strains.6,10
One randomized trial of 68 athletes with chronic adductor strain11 compared physical therapy (i.e., friction massage, stretching, transcutaneous electrical nerve stimulation, laser treatment) with active training exercise. A significantly greater number of participants (23 versus four in the physical therapy group) were able to return to their sport after an eight- to 12-week active training program. Further studies may corroborate this initial investigation, and active training methods may be the future in treating acute and chronic adductor strains. Nonsteroidal anti-inflammatory drugs (NSAIDs) and steroid injections have been mentioned in the treatment of these conditions, but their efficacy is debatable and lacks support in the literature.6
Patients with chronic adductor longus strains that have failed to respond to several months of conservative treatment have been shown to do well after surgical tenotomy and should be referred to a sports medicine surgeon for this consideration.12,13 Complete tears of the tendinous insertion from the bone, though rare, generally do better with surgical repair.9
Osteitis Pubis
Osteitis pubis is characterized by pubic symphysis pain and joint disruption.14 It occurs commonly in distance runners and soccer players, and has been found in some sports medicine clinics to be the most common cause of chronic groin pain.5 Osteitis pubis may be difficult to distinguish from adductor strains, and the two conditions may occur concomitantly in the same patient. Also, one must remember that osteomyelitis of the pubic symphysis, although usually seen following a surgical procedure around the pelvis, has been reported to occur spontaneously in athletes.15,16
The most likely mechanism is repetitive stress from increased shearing forces on the pubic symphysis or from increased stress placed on the joint from the traction of the pelvic musculature.17 Other factors, such as limitation of internal rotation of the hips or fixation of the sacroiliac joint, also place excessive stresses on the joint.18,19 No published clinical studies have addressed the role that biomechanical abnormalities of the lower limb (e.g., leg length discrepancies, excessive pronation, varus or valgus deformities) might play in the genesis of osteitis pubis. However, it is plausible that such abnormalities could place the pelvis in the path of excessive force.
The clinical symptoms of osteitis pubis include exercise-induced pain in the lower abdomen and medial thighs. Symptoms are gradual in onset, slowly increasing in severity if activities are not curtailed. One review article20 noted the following incidence of symptoms in patients with documented osteitis pubis: adductor pain in 80 percent, pain around the pubic symphysis in 40 percent, lower abdominal pain in 30 percent and hip pain in 12 percent. Referred scrotal pain, which is said to be typical, was found in only 8 percent.
On physical examination, tenderness over the pubic symphysis is usually present, and lack of such tenderness usually excludes the diagnosis.3 Pain can often be provoked by active adduction if the distal symphysis is involved, or by sit-ups if the proximal portion is involved.
Plain radiographs may show widening of the pubic symphysis, irregular contour of articular surfaces or periarticular sclerosis. However, in early or mild disease, radiographic findings may be normal.17 Plain films are also confusing in young patients because almost identical radiographic “abnormalities” may be seen during normal ossification.7 In one study of professional soccer players,21 radiographic changes around the symphysis were found in 76 percent of asymptomatic players.
An isotope bone scan may demonstrate increased uptake in the area of the pubic symphysis, but some patients who have symptoms fail to show any abnormality.7 Thus, clinicians are helped only by a positive scan. In a recent review of osteitis pubis,17 it was noted that the correlation between symptoms and either radiograph or isotope bone scan is difficult.
In general, treatment is based on physical rehabilitation. Pain-producing activity should be avoided and pain-free exercise should be maintained in the interest of general fitness.9 Physical therapy should progress in the usual stepwise fashion, with particular attention to hip range of motion and adductor stretching and strengthening. In addition, any biomechanical abnormalities that would place undue shear stresses on the pelvis (leg length discrepancy, excessive pronation, etc.) should be corrected.
Controversy surrounds the use of corticosteroid injections in this condition; however, they can be helpful in selected patients (e.g., athletes with acute osteitis pubis of less than two weeks' duration.)22
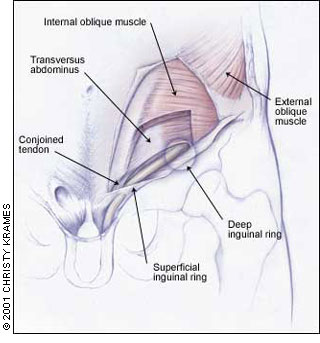
Sports Hernias
Posterior abdominal wall abnormalities causing groin pain include “sports hernias” and groin disruption (Figures 2 and 3). A sports hernia is caused by weakening of the posterior inguinal wall, resulting in an occult direct or indirect hernia. Because only the posterior abdominal wall is violated, no clinically detectable inguinal hernia is found on physical examination.23 Some researchers believe that sports hernias may be the most common cause of chronic groin pain in athletes.3,14 Other investigators have found them to be only a rare cause of chronic groin pain.24
Clinically, the sports hernia is characterized by insidious-onset, gradually worsening, diffuse, deep groin pain. It may radiate along the inguinal ligament, perineum and rectus muscles. Maneuvers that cause increases in intra-abdominal pressure will usually increase pain. Radiation of pain to the testicles is present in about 30 percent of symptomatic patients.9 Clinically, it is difficult to distinguish between sports hernia, distal rectus strain/avulsion and groin disruption. (See next section.) However, the pain of sports hernia is usually located more laterally and proximally than in groin disruption.
Radiographs, isotope bone scan and MRI may help exclude other causes of groin pain but are not useful in the diagnosis of sports hernia.24 Nonoperative treatment is rarely successful, but because a definitive diagnosis is often difficult to make, a trial of several weeks of conservative treatment may be warranted. If symptoms persist, the patient should undergo surgical exploration and repair. A 90 percent success rate is reported.23
Groin Disruption
Groin disruption was first described in 1980 when three professional soccer players with chronic, apparently career-ending groin pain underwent surgical exploration and repair and were then able to return to competitive sport. The phrase “groin disruption” today is often used interchangeably with sports hernia, and the literature is not clear on proper terminology.8
The posterior abdominal wall abnormalities found in groin disruption are more varied than those associated with sports hernias. They may include tears of the external oblique aponeurosis, tears of the conjoined tendon or dehiscence of the conjoined and inguinal ligament25—again without any evidence of a “regular” hernia. In a study of 157 athletes who underwent surgery for chronic groin pain,24 57 percent were found to have “loose-feeling inguinal floors.” Forty-eight percent had external oblique aponeurosis defects and 23 percent had a thin insertion or tear of the rectus abdominus.
Clinically, these patients present with groin pain on exertion, but pain with Valsalva's maneuver, coughing or sneezing is uncommon (10 percent of patients). Many patients (about 65 percent) also have pain with resisted adduction of the hip.24 Pain and tenderness may be provoked with pressure or when the patient does half sit-ups.
Radiographs, computed tomographic (CT) scans, isotope bone scans and MRI are helpful in excluding other injuries, but less helpful in establishing the diagnosis of groin disruption. Diagnosis is usually made only at the time of surgery.24
After a trial of conservative treatment, definitive surgical repair is usually required. In more than 95 percent of cases, the athlete returns to his or her pre-injury level of competition.
Iliopsoas Strains/Bursitis
The anatomy of the region of the iliopsoas is shown in Figure 4. The iliopsoas bursa is the largest bursa in the body and communicates with the hip joint in 15 percent of patients.4,26 Bursitis is caused by overuse and friction as the tendon rides over the iliopectineal eminence of the pubis. The condition is associated with sports requiring extensive use of the hip flexors (e.g., soccer, ballet, uphill running, hurdling, jumping). Iliopsoas bursitis is characterized by deep groin pain, sometimes radiating to the anterior hip or thigh, often accompanied by a snapping sensation. (See section on snapping hip syndrome.) If severe enough, it may be accompanied by a limp.8
The pain is difficult for patients to localize and difficult for clinicians to reproduce. In fact, the average time from the onset of symptoms to diagnosis is 31 to 42 months.26 Physical examination will, however, reveal pain on deep palpation over the femoral triangle (adjacent to the femoral artery), where the musculotendinous junction of the iliopsoas can be palpated.26 (Figure 5 shows the anatomy of this region.) Pain may also be produced when the affected hip is extended or when the supine patient raises his or her heels off the table at about 15 degrees. In the latter position, the only active hip flexor is the iliopsoas.6

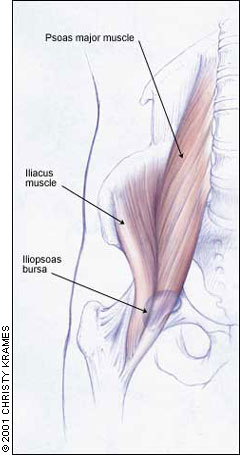
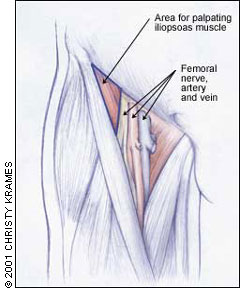
Iliopsoas bursitis is best visualized on MRI, which reveals a collection of fluid coursing adjacent to the muscle.7 Treatment is conservative and consists of rest followed by stretching of the hip flexors and rotators, then strengthening and gradual return to sport. As in any overuse injury, biomechanical abnormalities must be sought and corrected. Corticosteroid injections, usually performed with imaging localization, may be helpful in selected patients. Rarely, surgical management of recalcitrant cases is warranted.26
Stress Fractures
The two commonly encountered stress fractures centered in the groin region are femoral neck stress fractures and pubic ramus fractures. These are caused by repetitive overuse and overload as seen in distance runners or military recruits. Contributing risk factors include relative osteoporosis in young female athletes with nutritional or hormonal imbalances, muscle fatigue (which may reduce shock-absorbing abilities), changes in foot gear or training surface, or sudden increases in the training regimen.4,27
Femoral neck stress fractures present with groin or anterior thigh pain that is exacerbated by activity and relieved by rest. Again, the pain is difficult to localize on physical examination, but the diagnosis may be suggested by painful limitation of internal rotation of the hip.
If the diagnosis is suspected by history, radiographs may be obtained, keeping in mind that changes (when present) normally lag behind the onset of symptoms by two to four weeks. Isotope bone scan or MRI should be performed to make an early, definitive diagnosis.4 Compared with isotope bone scan, MRI has a similar sensitivity but an improved specificity, and is becoming the diagnostic procedure of choice in some medical centers.28
Runners with stress fractures of the inferior femoral neck (compression side) seen on MRI or CT can be treated conservatively, with good prognosis for uneventful healing. Many clinicians recommend follow-up imaging to ensure healing before progression of activity. Return to running usually occurs in two to three months.9
Superior femoral neck stress fractures (traction/tension) are more worrisome and must be treated with open reduction and internal fixation because the risk of progression to complete fracture, displacement and avascular necrosis is high.27
Inferior pubic ramus stress fracture is less worrisome.8 It usually occurs in female distance runners and military recruits, and is fairly easily diagnosed. On physical examination, pain may be elicited on palpation directly over the pubic ramus. Pain is also elicited by one-legged standing or jumping. The diagnosis can be confirmed by a bone scan. Treatment is conservative and straightforward: four to six weeks of relative rest followed by gradual return to sport. Most athletes show complete healing within three to five months.
In femoral neck and pubic ramus stress fractures, treatment would be incomplete without also addressing and modifying risk factors. Maintenance of hormonal and nutritional balance, modification of foot gear and training surface, and conscientious review of the athlete's training program should be undertaken.
Avulsion Fractures
Avulsions are seen mainly in adolescent athletes and occur in three main locations (Figure 6). First, avulsions from the anterior superior iliac spine (ASIS) are caused by rapid sartorius contraction and are experienced during jumping sports. Second, avulsions from the anterior inferior iliac spine (AIIS) are caused by strong rectus femoris contractions and are seen mainly in kicking sports such as soccer. Third, avulsions from the ischial tuberosity occur when the hamstrings are subject to violent contractions in sprinting and hurdling sports.
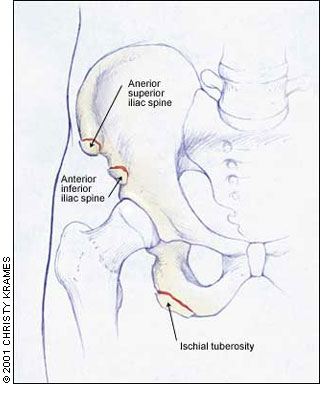
Nonoperative treatment is generally recommended for avulsions from the ASIS and AIIS, and good results can be expected. Treatment of avulsions of the hamstrings from the ischial tuberosity is controversial. Orthopedic evaluation is warranted in these patients. Large fragments displaced greater than 1 to 2 cm may require surgical fixation.9
Nerve Compression
Nerve compression in the groin is uncommon but can include injury to the ilioinguinal nerve, lateral femoral cutaneous nerve or the obturator nerve.14
ILIOINGUINAL NERVE
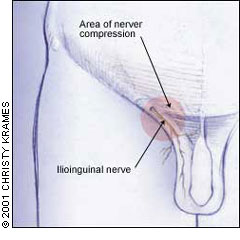
Ilioinguinal nerve compression is a well-established cause of chronic groin pain in patients who have undergone appendectomy or herniorrhaphy. It is also a cause of chronic groin pain in athletes, in whom the nerve can be injured by direct trauma or by overzealous training of the abdominal musculature.3
The nerve transmits sensation from the base of the penis and scrotum (or in women, the labia majora and mons pubis) and from the upper medial thigh. It traverses the inguinal canal/superficial inguinal ring and crosses through the abdominal musculature where compression can occur (Figure 7).
Diagnosis of ilioinguinal nerve compression can often be determined by eliciting Tinel's sign and can be confirmed when an injection of local anesthesia over the site of entrapment or injury relieves pain.3,9 Treatment consists of local corticosteroid injections or, if pain is refractory, surgical neurolysis.3
OBTURATOR NERVE
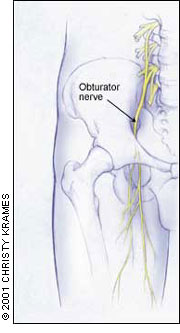
Obturator nerve entrapment is becoming more widely recognized as a cause of chronic groin pain in athletes. The obturator nerve supplies the adductor muscles and has a variable cutaneous distribution to the medial thigh (Figure 8). Two recent studies from Australia29,30 reviewed 182 cases of obturator-induced chronic groin pain. These athletes (Australian-rules football players and soccer players) experienced deep aching centered on the adductor origin at the pubic bone. With exercise, the pain became more severe and radiated down the medial thigh toward the knee. Some of the athletes also experienced exercise-related weakness in the affected leg, especially when attempting to jump. Paresthesias were rarely present.
Diagnosis can be made by electromyogram (if symptoms are present longer than three months) where a denervation pattern of the adductor longus and brevis is seen.
LATERAL FEMORAL CUTANEOUS NERVE
The lateral femoral cutaneous nerve passes under or through the inguinal ligament, where compression and meralgia paresthetica(paresthesias in the proximal lateral portion of the hip) can occur (Figure 9). Lateral femoral cutaneous nerve entrapment has been noted in women who sit with the involved leg underneath the body. It has also been seen in rifle team members who were required to sit in this same position for prolonged periods. Treatment is composed of refraining from the offending activity; rarely, surgery is warranted.
Snapping Hip Syndrome
Snapping hip syndrome refers to a snapping sensation felt about the hip with movement. Less than one third of these patients experience pain with snapping.31 The abnormality may be classified as external/lateral or as interior/medial/anterior. The more common external/lateral syndrome occurs when the iliotibial band, tensor muscle of fascia lata or gluteus medius tendon rides back and forth across the greater trochanter, where bursitis may also develop.

Internal causes of snapping hip include the iliopsoas tendon passing over the iliopectineal eminence, acetabular labral tears, subluxation of the hip and loose bodies.14
The physician should attempt to identify the source of the clicking on physical examination and treatment should be undertaken if pain is present. Correcting any contributing biomechanical abnormalities and stretching tightened muscles (e.g., iliopsoas muscle, iliotibial band) are important. Corticosteroid injections can be useful if bursitis is present. Surgical treatment is rarely indicated unless loose bodies are the cause of the syndrome.
Final Comment
The family physician should be aware of the complex anatomy in the groin region, keep in mind the many diagnostic possibilities and approach the physical examination in a systematic manner. Correct diagnosis is paramount to ensure that proper treatment is started so that athletes may be optimally rehabilitated and returned to sport in a timely fashion.