
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2002;65(1):93-97
Peritonsillar abscess, the most common deep infection of the head and neck that occurs in adults, is typically formed by a combination of aerobic and anaerobic bacteria. The presenting symptoms include fever, throat pain, and trismus. Ultrasonography and computed tomographic scanning are useful in confirming a diagnosis. Needle aspiration remains the gold standard for diagnosis and treatment of peritonsillar abscess. After performing aspiration, appropriate antibiotic therapy (including penicillin, clindamycin, cephalosporins, or metronidazole) must be initiated. In advanced cases, incision and drainage or immediate tonsillectomy may be required.
Peritonsillar abscess is the most common deep infection of the head and neck that occurs in adults. This infection begins as a superficial infection and progresses into tonsillar cellulitis. A peritonsillar abscess forms at the most advanced stage. Early diagnosis of the abscess allows appropriate treatment to begin before the abscess spreads into the surrounding anatomic structures. A family physician who has appropriate training can diagnose and treat the majority of patients with peritonsillar abscess.
Epidemiology
Peritonsillar abscess is most common in persons 20 to 40 years of age. Young children are seldom affected unless they are immuno-compromised, but the infection can cause significant airway obstruction in children.1,2 This infection affects males and females equally. Evidence shows that chronic tonsillitis or multiple trials of oral antibiotics for acute tonsillitis may predispose persons to the development of a peritonsillar abscess.3
Anatomy
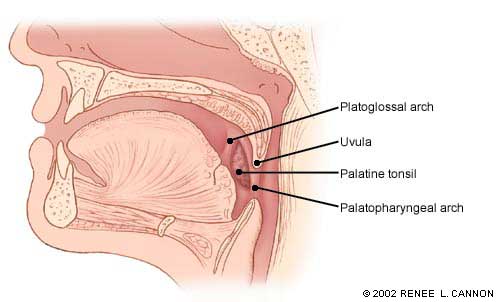
The normal anatomy of the palatine tonsils and their surrounding tissues is depicted in Figure 1. The two tonsillar pillars define the palatine tonsils anteriorly and posteriorly. The glossopalatine and the pharyngopalatine muscles are the major muscles of the anterior and posterior pillars, respectively. The tonsil lays in the depression between the palatoglossal and the palatopharyngeal arches.4
During the embryonic stage, the tonsils arise from the second pharyngeal pouch as buds of endodermal cells.5 Shortly after birth, the tonsils grow irregularly and reach their ultimate size and shape, depending on the amount of lymphoid tissue present.
Each tonsil has an irregular number of ingrowths of the surface epithelium known as tonsillar crypts. The tonsils are surrounded by a capsule, a specialized portion of the intrapharyngeal aponeurosis that covers the medial portion of the tonsils and provides a path for blood vessels and nerves through its fibers.6
Peritonsillar abscesses form in the area between the palatine tonsil and its capsule. If the abscess progresses, it can involve the surrounding anatomy, including the masseter muscles and the pterygoid muscle. If severe, the infection can also penetrate the carotid sheath.
Etiology
The most common organisms associated with peritonsillar abscess are listed in Table 1. Streptococcus pyogenes (group A beta-hemolytic streptococcus) is the most common aerobic organism associated with peritonsillar abscess. The most common anaerobic organism is Fusobacterium. For most abscesses, a mixed profile of both aerobic and anaerobic organisms cause the infection.7–9
| Aerobic | Anaerobic |
|---|---|
| Streptococcus pyogenes | Fusobacterium |
| Staphylococcus aureus | Peptostreptococcus |
| Haemophilus influenzae | Prevotella |
| Neisseria species | Bacteroides |
Diagnosis
The most important information to obtain during the patient's history is the location of the pain in the throat, which suggests the location of the abscess. A thorough history should determine if the patient has a fever, has difficulty swallowing or has possibly ingested foreign objects. During the physical examination, trismus (inability or difficulty in opening the mouth) is often present because of inflammation of the pharyngomaxillary space and pterygoid muscle.1 A distinguishing feature on physical examination is the inferior medial displacement of the infected tonsil with a contralateral deviation of the uvula (Figure 2).3 In addition, many patients will have a thickened, muffled voice often described as having a “hot potato” quality. The most common findings from the history and physical examination are summarized in Table 2.
| Symptoms | Physical examination |
| Progressively worsening sore throat, often localized to one side Fever Dysphagia Otalgia Odynophagia | Erythematous, swollen tonsil with contralateral uvular deviation Trismus Edema of palatine tonsils Purulent exudate on tonsils Drooling Muffled, “hot potato” voice Cervical lymphadenopathy |
Table 3 outlines the differential diagnosis of peritonsillar abscess. Peritonsillar cellulitis is present when the area between the tonsil and its capsule is erythematous but lacks pus. The presence of mononucleosis can be determined by obtaining a complete blood count and a heterophile screen. During the physical examination, the physician should perform a thorough intraoral inspection to rule out an infection of the salivary glands, teeth, and mastoid bone, as well as neoplasms, cervical adenitis, and aneurysm of the internal carotid artery.
| Peritonsillar cellulitis | Cervical adenitis |
| Tonsillar abscess | Dental infections |
| Mononucleosis | Salivary gland infection |
| Foreign body aspiration | Mastoid infection |
| Neoplasms (lymphoma, leukemia) | Aneurysm of internal carotid artery |
A thorough history and physical examination can often determine a diagnosis of peritonsillar abscess, but radiologic tests may be helpful in differentiating peritonsillar abscess from other diagnoses. Ultrasonography is the easiest and most useful tool. The ultrasound can be obtained transcutaneously by placing the transducer over the sub-mandibular gland and scanning the entire tonsillar area.
If there is a peritonsillar abscess, the abscess formation will be demonstrated as an echo-free cavity with an irregular, well-defined circumference.10 The ultrasound can also be performed intraorally by placing the patient in a sitting position. With the use of a tongue blade, the probe can be used to scan the tonsils for echo-free areas. The presence of trismus may limit the ability to use intraoral sonography.11,12
The use of computed tomographic (CT) scanning may also be helpful in identifying an abscess formation. The CT scan should be obtained with contrast to allow for optimal viewing of the abscess. An area of low attenuation on a contrast-enhanced CT scan is suggestive of abscess formation. Other indications of a peritonsillar abscess that are present on CT scanning include diffuse swelling of the soft tissues with loss of the fat planes and the presence of edema in the surrounding area.13,14
NEEDLE ASPIRATION
The gold standard for diagnosis of peritonsillar abscess remains the collection of pus from the abscess through needle aspiration. To obtain this sample, the area should be anesthetized with 0.5 percent benzalkonium (Cetacaine spray) followed by a gargle of 2 percent lidocaine (Xylocaine) with epinephrine. A no. 18-gauge spinal needle attached to a 10-mL syringe can be used to obtain material from the suspected abscess. Figure 3 illustrates this procedure being performed. The fluid obtained should be sent to the laboratory for gram stain and culture to determine the appropriate treatment regimen.
A needle aspiration of a peritonsillar abscess should only be performed by properly trained physicians. Complications of performing the aspiration can include aspiration of pus and blood, and hemorrhage. If the abscess is located in the distal part of the tonsil, puncture of the carotid artery can occur.
Treatment
The treatment of peritonsillar abscess requires both the selection of appropriate antibiotics and the best procedure to remove the abscessed material. Individualized treatment modalities will result in more successful outcomes.
The choice of antibiotics is highly dependent on both the gram stain and culture of the fluid obtained from the needle aspiration. Penicillin used to be the antibiotic of choice for the treatment of peritonsillar abscess, but in recent years the emergence of beta-lactamase-producing organisms has required a change in antibiotic choice.15 Results of studies16,17 suggest that 500 mg of clindamycin administered twice daily or a second- or third-generation oral cephalosporin be used instead of penicillin.
Another study1 recommends using penicillin as the first-line agent, and, if there is no response within the first 24 hours, adding 500 mg of metronidazole administered twice daily to the regimen. All specimens should be examined by culture for antibiotic sensitivity to ensure appropriate antibiotic coverage.
In one study,16 52 consecutive patients who had a positive needle aspiration of a peritonsillar abscess were randomized into two groups comparing needle aspiration alone with incision and drainage.8 There were no significant differences between the two groups in duration of symptoms or initial treatment failure. The results indicated that no further surgical management for peritonsillar abscess was required following the initial needle aspiration. Another study17 conducted in 1991 reported similar results.
A retrospective study18 of 160 patients compared patients who received needle aspiration alone with patients who had undergone incision and drainage. In this study, only eight patients (0.5 percent) required incision and drainage after multiple failed needle aspirations. The authors concluded that needle aspiration alone was an appropriate treatment regimen, but a higher rate of recurrence occurred that could ultimately require incision and drainage.
Controversy remains over the necessity of incision and drainage versus needle aspiration alone. However, most otolaryngologists consider incision and drainage to be the gold standard for treatment. An otolaryngologist should usually be consulted to perform this procedure unless the treating physician has the appropriate experience and training. A review of the incision and drainage technique for peritonsillar abscess is beyond the scope of this article.
Most experts agree that immediate tonsillectomy is not required for treatment of peritonsillar abscess. Tonsillectomy should be performed three to six months after the abscess in patients who have recurrent tonsillitis or peritonsillar abscess. If the family physician is inexperienced in treating peritonsillar abscess, an otolaryngologist should be consulted at the time of the diagnosis to determine the appropriate surgical treatment.