
Am Fam Physician. 2002;65(7):1409-1412
A patient information handout on excision of epidermoid cysts is provided on page 1423.
Epidermoid cysts are asymptomatic, dome-shaped lesions that often arise from a ruptured pilosebaceous follicle. The minimal excision technique for epidermoid cyst removal is less invasive than complete surgical excision and does not require suture closure. The procedure is easy to learn, and most physicians experienced in skin surgery can perform the procedure after three to five precepted sessions. It involves making a 2- to 3-mm incision, expressing the cyst contents through compression and extracting the cyst wall through the incision. Gauze or a splatter shield should be used to protect the physician from spraying of cyst contents. The rarity of associated cancer makes histologic evaluation necessary only if unusual findings or clinical suspicion of cancer is present. Inflamed cysts are difficult to e excise, and it is often preferable to postpone excision until inflammation has subsided.
Epidermoid cysts are asymptomatic, slowly enlarging, firm-to-fluctuant, dome-shaped lesions that frequently appear on the trunk, neck, face, scrotum or behind the ears. Occasionally, a dark keratin plug (a comedo) can be seen overlying the cyst cavity. These epithelial, walled cysts vary from a few millimeters to 5 cm in diameter. The cysts are mobile unless fibrosis is present.
The term “sebaceous cyst” has fallen into disuse; current terms include epidermal cyst, keratin cyst, epithelial cyst, and epidermoid cyst. Other types of cysts are included in Table 1. Epidermoid cysts often arise from a ruptured pilosebaceous follicle associated with acne. Duct obstruction of a sebaceous gland in the hair follicle can result in a long, narrow channel opening in the surface comedo. Other causes include a developmental defect of the sebaceous duct or traumatic implantation of surface epithelium beneath the skin.
The cysts contain keratin and lipid, and the rancid odor often associated with these cysts relates to the relative fat content, bacterial infection, or decomposition. Spontaneous rupture discharges the soft, yellow keratin material into the dermis. A tremendous inflammatory response (foreign-body reaction) ensues, often producing a purulent material. Scarring makes removal more difficult.
| Branchial cleft cyst | Myxoid cyst |
| Dermoid cyst | Parotid tumor |
| Favre-Racouchot syndrome | Pilar cyst |
| Fibrous tissue tumor | Pilonidal cyst |
| Gardner's syndrome | Preauricular cyst |
| Lipoma | Steatocystoma |
| Median raphe cyst | Thyroglossal duct |
| Milia |
Most cysts are simple lesions, but a few special situations should be considered. Multiple epidermoid cysts (associated with lipomas or fibromas of the skin) and osteomas should be considered as part of Gardner's syndrome, with associated premalignant colonic polyps. Dermoid cysts of the head often can be confused with epidermoid cysts, and attempted removal of a dermoid cyst can create a wound with Excision and closure of epidermoid cysts can be difficult if inflammation is present; it may be preferable to postpone excision until the inflammation has subsided. intracranial communication. Some cysts can be associated with basal cell and squamous cell carcinoma, and some authors advocate histologic evaluation of the wall of all removed cysts. The rarity of associated cancer makes routine histologic evaluation necessary only when solid tumors or unusual findings are present.
Cyst infection can develop spontaneously or following rupture. It is often unclear whether an inflamed cyst is infected, and many physicians prefer to treat these lesions with antibiotics, incision, and drainage. Excision and closure can be very difficult with inflamed cysts, and it may be preferable to postpone the surgical procedure until the inflammation has subsided (typically one week).
There are many surgical approaches to epidermoid cysts. While complete surgical excision can ensure removal of the sac and prevent recurrence, this technique is time-consuming and requires suture closure. The minimal excision technique has been proposed as a less invasive and successful intervention. The minimal excision technique involves a 2- to 3-mm incision, expression of the cyst contents, and extraction of the cyst wall through the incision. Vigorous finger compression is used to express the cyst contents and loosen the cyst wall from the surrounding tissues to facilitate removal of the sac. The tiny wound can be closed with a single suture, although most physicians do not close this opening. A variation of this technique uses a punch biopsy instrument to create the opening into the cyst.
Expression of the cyst contents through the small opening can cause the sebaceous material to spray across the surgery room. Gauze can be used to cover the area as compression is applied, or a clear adhesive splatter-control shield can be used to cover the site. Some practices require the use of protective eye wear for the procedure.
Simple incision and drainage of cysts frequently results in recurrence. Two iodine crystals can be placed in the center of the cyst and, during the next few weeks, the cyst will become dark brown and hard. This hard nodule can then be expressed from the skin. This simple technique is inexpensive, but the need for a follow-up visit and the length of time for lesion removal may make this technique less desirable to many patients.
Other Types of Epithelial Cysts
Pilar or Trichilemmal Cyst (Wen). These cysts occur predominantly on the scalp, are odorless and have less fat and more keratin than epidermoid cysts. They are very amenable to removal by the minimal excision technique.
Dermoid Cyst. These congenital cysts occur in the lines of cleavage and sublingually around the eyes and on the base of the nose. These cysts have a rancid odor. The lesions can extend intracranially, and a preoperative computed tomographic (CT) scan is recommended.
Milia. These 1- to 2-mm lesions can arise spontaneously or can be caused by trauma. A small nick in the epidermis with a no. 11 blade allows expression of the keratinaceous white kernel.
Steatocystoma Multiplex. These multiple, small, yellow, cystic nodules (a few millimeters in diameter) can be found on the trunk, upper arms, axillae and thighs. The multitude of lesions may preclude cyst removal.
Favre-Racouchot Syndrome. These multiple lesions on the face result from profound sun damage. The pilosebaceous openings stretch, and the orifices fill with keratin material, producing comedones and cysts.
Methods and Materials
EQUIPMENT
Nonsterile Tray for Anesthesia
Place the following items on a nonfenestrated drape covering a Mayo stand:
Nonsterile gloves and mask
1 inch of 4 × 4 gauze soaked with povidone-iodine solution
1 inch of 4 × 4 gauze
5-mL syringe, filled with 2 percent lidocaine with epinephrine (Xylocaine with epinephrine) with a 30-gauge needle
25-gauge, 1 ¼-inch needle (for anesthetizing beneath the cyst)
Sterile Tray for the Procedure
Place the following items on a sterile drape covering a Mayo stand:
Sterile gloves
Fenestrated disposable drape
Two sterile bandages to anchor the drape
Three small-tipped hemostats (mosquito clamps)
No. 11 blade
Needle holder for suturing (if needed)
Iris scissors
Adson forceps
2 inches of 4 × 4 sterile gauze
Suture materials (if needed)
Splatter control shield (if desired)
Some physicians use the nonsterile gloves that were used to administer the anesthesia for the removal of small or superficial cysts.
Procedure Description
1. The skin overlying the site is cleansed with povidone-iodine solution. The skin overlying the cyst and the tissue to the sides and beneath the cyst are anesthetized with 2 percent lidocaine with epinephrine.
2. A fenestrated drape can be placed on the patient, with the lesion beneath the fenestration. A no. 11 blade is used to create a stab incision into the center of the cyst. A small-tipped hemostat is placed into the cyst, the tips gently opened and compression applied to allow the cyst con tents to pass through the opening (Figure 1).
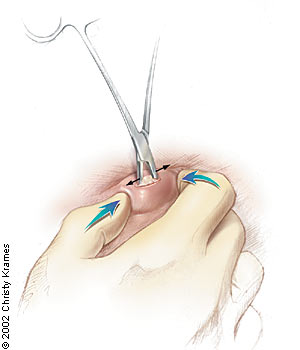
3. The hemostat can be removed, and both thumbs are used to express the cyst contents. Gauze or a splatter shield can be used to shield the physician from splatter. The hemostat can be reinserted, if needed, to assist with passage of the sebaceous material.
4. Following vigorous and complete expression, the hemostat is reintroduced into the cyst cavity, and the capsule at the base of the wound is grasped and elevated. An attempt should be made to gently remove the entire sac through the small opening (Figure 2). The sac may break, and several pieces may need to be removed.
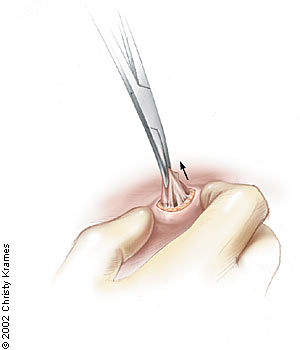
5. At the end of the procedure, the wound should be inspected to ensure that all of the cyst wall has been removed. The cyst wall can be pieced together to provide additional confirmation of complete removal.
6. Direct pressure is applied to the site with gauze. Antibiotic ointment is applied and gauze is taped over the site. The patient is encouraged to hold direct pressure (using gauze) to the site for one to two hours following the procedure. Most small incisions do not require suture closure.
Follow-Up
Malignant growths may require a second procedure to provide a wider margin of excision around the original lesion. Rarely, malignancy may be detected at the site of the original surgery. Once the cyst contents have been squeezed out, a mass may be palpated adjacent to the cyst, suggesting that a tumor may be present. It is recommended that the minimal excision technique be abandoned for a formal excision and biopsy if a solid tumor is detected. If malignancy is discovered in a cyst wall that is removed at the time of the minimal excision technique, the physician may consider a second excision.
Because malignancy is rarely associated with a cyst, some physicians believe it is not cost-effective to send all epidermoid cyst walls for histologic evaluation. Others believe that all specimens should be sent for evaluation because the literature does note the occurrence of cancer. Certainly any atypical-appearing lesion or one associated with a palpable irregularity in the cyst wall should be sent for histologic analysis.
Many lesions can be confused with epidermoid cysts. If a solid tumor is discovered at the time of the procedure, a biopsy should be obtained. Incisional biopsy can be performed for very large lesions, and excisional biopsy for the smaller lesions. Pilar tumors of the scalp are often confused with epidermoid cysts and may require wide excision because they can erode into the skull.
Simple epidermoid cysts that appear to be completely excised do not generally require follow-up. If a recurrence is brought to the physician's attention at a later date, standard surgical excision should be attempted.
Procedure Pitfalls/Complications
The Contents of the Cyst Sprayed. Vigorous expression of the cyst contents can cause material to literally fly across the room. Gauze should be loosely held over the site to prevent spraying. Masks and eye protection may be needed for the physician, and care should be taken to avoid spraying the nursing personnel. Some physicians use a splatter control shield to avoid this problem.
The Cyst Wall Will Not Come Out of the Tiny Incision. Cysts that have previously ruptured or been inflamed may have significant adjacent scarring. The scarring may preclude removal with the minimal excision technique. In addition, less-experienced physicians are often not vigorous enough when compressing the cyst. Pressure applied with the thumbs can loosen the cyst wall from the surrounding tissues. Inability to remove the cyst should prompt the physician to perform a formal excision procedure.
The Cyst Wall Breaks During the Procedure. Cyst wall breakage during the procedure may relate to the surgical technique or the anatomic location of the cyst. Cysts on the scalp (trichilemmal cysts, or wens) may have thicker walls than typical epidermoid cysts on the face. Many physicians report that it is easier to remove scalp cysts intact. Thin-walled cysts tend to break and may need to be removed in pieces; however, if adequate kneading of the skin occurs before attempted removal, many cysts can be removed intact.
A Blood Clot Developed After Cyst Wall Removal. Removal of large cysts can create a significant open space beneath the skin. Hematomas or infectious material can fill this space. Major bleeding is rarely associated with this procedure, and hematomas can be avoided by having the patient apply firm pressure (using gauze) to the surgical site after the procedure. Direct pressure can also express any clot that may develop at this site.
Expressing the Cyst Contents Is Tiring. The minimal excision technique can be physically demanding when performed correctly. Despite the amount of work that is required, this technique can be very gratifying to the physician and patient. Using the thumbs to express the cyst contents produces greater pressure.
Cyst Contents Could Not Be Expressed. Solid tumors may masquerade as a typical epidermoid cyst. The pilar cyst or pilar tumor of the scalp can be confused with a typical cyst, and the pilar tumor can invade surrounding tissues. If a solid tumor is suspected during minimal excision, it should be removed by a formal surgical excision and sent for histologic evaluation.
Physician Training
Formal training is needed for the techniques of anesthetic administration, lesion excision, and closure, if it is performed. Most family physicians receive the necessary surgical skills during their residency training. Others could obtain this training with the assistance of an experienced preceptor. Most physicians experienced in skin surgery can perform these procedures unsupervised after three to five precepted procedures.