
Am Fam Physician. 2002;65(10):2067-2068
Umbilical granulomas are common inflammatory reactions to the resolving umbilical stump. The double-ligature technique is simple to perform and provides good cosmetic and functional results with only minor complications. The granuloma becomes necrotic and drops off within seven to 14 days. The double-ligature is a preferable alternative to multiple topical applications of silver nitrate for the treatment of pedunculated umbilical granulomas in children.
The umbilical cord normally separates within three days to two months postpartum.1 After separation, an excess of granulation tissue may persist at the base. These umbilical granulomas consist of true granulation tissue with fibroblasts and abundant capillaries, and their surfaces often have a pedunculated appearance. Persistent drainage from the base of the cord or chronic periumbilical inflammation unresponsive to the usual therapy for omphalitis is suggestive of a patent urachus or an omphalomesenteric duct as the underlying disease.2 The differential diagnosis of umbilical granulomas can be seen in Table 1.
| Vestiges of urachus | Vestiges of omphalomesenteric duct | Umbilical masses | |||
| Fistula Sinus Cyst Bladder diverticulum | Mucosal polyp Sinus Fistula Meckel's diverticulum Cyst | Polyp Urachal remnant Cyst Ectopic pancreatic tissue Adenoma | |||
| Umbilical hernia | |||||
Although treatment of umbilical granulomas can be conservative, such as using alcohol or chlorhexidine (Peridex), the most common treatment is the topical application of concentrated silver nitrate solution or stick (75 percent). Because chemical burns to the periumbilical area are a possible complication of this technique, caution is imperative.3–5 Careful drying of the umbilical exudate to prevent spillage is essential in preventing staining of the skin or chemical burns. Further protection can be attained by isolating the skin around the umbilicus with petroleum jelly cream before each application. Cryosurgery is another treatment option.6,7 Surgical excision of umbilical granulomas is rarely necessary.
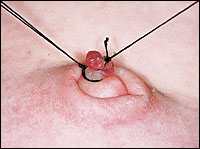
Most umbilical granulomas are located relatively deep into the umbilical region and are difficult to locate (Figure 1). The double-ligature technique overcomes the technical difficulty of ligating the granuloma on its base. After cleansing and prepping the periumbilical area with a povidone-iodine solution, 3-0 silk sutures are used for ligation. The use of 4-0 silk sutures is only necessary with more delicate and friable umbilical granulomas.

The first stage of the double-ligature procedure involves placing the superficial “stay” ligature, which brings the granuloma into a position more easily approached (Figure 2). The second stage involves placing a deeper and more precise ligature at the base of the lesion (Figure 3). Before positioning this final ligature, ask the child's mother or father to hold up the first ligature; this gives them a feeling of active participation in the therapeutic process and results in a more precise final ligature. The granuloma becomes necrotic and drops off within seven to 14 days, similar to the original umbilical cord remnant. The complications of this technique are minor and include bleeding, especially with large sessile umbilical granulomas. Some larger granulomas may require more than one double-ligature.

The only contraindications for this double-ligature technique are the large sessile umbilical granulomas with a wide base, small deep lesions and very friable lesions that may bleed during the procedure. Before performing the ligation, a complete evaluation should be conducted to rule out more serious pathology on any lesion in question.