
Am Fam Physician. 2002;66(5):785-795
Most ankle injuries are straightforward ligamentous injuries. However, the clinical presentation of subtle fractures can be similar to that of ankle sprains, and these fractures are frequently missed on initial examination. Fractures of the talar dome may be medial or lateral, and they are usually the result of inversion injuries, although medial injuries may be atraumatic. Lateral talar process fractures are characterized by point tenderness over the lateral process. Posterior talar process fractures are often associated with tenderness to deep palpation anterior to the Achilles tendon over the posterolateral talus, and plantar flexion may exacerbate the pain. These fractures can often be managed nonsurgically with nonweight-bearing status and a short leg cast worn for approximately four weeks. Delays in treatment can result in long-term disability and surgery. Computed tomographic scans or magnetic resonance imaging may be required because these fractures are difficult to detect on plain films.
Ankle injuries are commonly evaluated by primary care and emergency physicians. Most of these injuries do not pose a diagnostic dilemma and can be managed nonsurgically without a prolonged or costly work-up. However, the clinical presentation of some subtle fractures can be similar to that of routine ankle sprains, and they are commonly misdiagnosed as such. Many of these injuries, if left without a definitive diagnosis, result in long-term disability (Table 1).
| Fracture type | Mechanism of injury | Important physical examination findings* | Best plain radiograph† | Treatment |
|---|---|---|---|---|
| Talar dome (lateral) | Inversion with dorsiflexion | Tenderness anterior to the lateral malleolus, along the anterior border of the talus | Mortise view: shallow, wafer-shaped lesion | Stage I or II (see Table 3): NWBSLC for six weeks Stage III or IV (see Table 3), or persistent symptoms: surgical Treatment |
| Talar dome (medial) | Inversion with plantar flexion or atraumatic | Tenderness posterior to the medial malleolus, along the posterior border of the talus | AP view: deep, cup-shaped lesion; initial radiograph can be normal because changes in subchondral bone may not develop for weeks. | Stage I, II, or III (see Table 3): NWBSLC for six weeks Stage IV (see Table 3): surgical treatment |
| Lateral talar process | Rapid inversion with dorsiflexion | Point tenderness over the lateral process (anterior and inferior to the lateral malleolus) | Mortise view; lateral view may show subtalar effusion | Small fragment with <2 mm Displacement: NWBSLC for four to six weeks Large or displaced fragments: operative treatment |
| Posterior talar Process (lateral tubercle) | Hyperplantar flexion or forced inversion | Tenderness to deep palpation anterior to the Achilles tendon over posterolateral talus Plantar flexion may reproduce pain. | Lateral radiograph (an accessory ossicle, the os trigonum, may be present) | Minimally displaced fracture: NWBSLC for four to six weeks Large or displaced fragments or persistent symptoms: operative treatment |
| Posterior talar process (medial tubercle) | Dorsiflexion with pronation | Tenderness to deep palpation between the medial malleolus and the Achilles tendon | Difficult with standard views; an oblique ankle radiograph taken with the foot placed in 40 degrees of external rotation has been successful. | Similar to lateral tubercle Fractures |
| Anterior process of the calcaneus | Inversion with plantar flexion can lead to an avulsion fracture. Forced dorsiflexion compression fracture. | Point tenderness over the calcanealcuboid joint (approximately 1 cm inferior and 3 to 4 cm anterior to the lateral malleolus) | Lateral radiograph (an accessory ossicle, the calcaneus secondarium, may be present) | Small nondisplaced fracture: nonweight-bearing with compressive dressing or NWBSLC for four to six weeks Large or displaced fractures may require operative treatment. |
This article features subtle fractures to facilitate timely diagnosis and treatment of these less-common injuries. These fractures should be considered in the differential diagnosis of any acute ankle sprain, as well as any suspected sprain that does not improve with routine treatment (Table 2).
| Acute care | Joint rest, ice, compression, and elevation (RICE) |
| Simple analgesics for 24 to 72 hours | |
| Follow-up care | Progressive range-of-motion and proprioceptive exercises |
| Protection from further ankle injury with a wrap or brace | |
| Gradual return to normal activity level |
Overall, optimal results are achieved with early diagnosis and treatment of these fractures. When treatment is delayed, patients tend to have a more complex clinical course.
Talar Dome Injuries
The dome of the talus articulates with the tibia and fibula, and has a key role in ankle motion and in supporting the axial load during weight bearing1–4 (Figures 1 and 2). Fractures of the talar dome are generally the result of inversion injuries of the ankle. They are located medially or laterally with equal frequency and occasionally through both.3–5 Lateral talar dome fractures are almost always associated with trauma, while medial talar dome lesions can be traumatic or atraumatic in origin.
Although the etiology in atraumatic lesions is unclear, osteochondral fragments can separate from the surrounding cartilage surface and dissect into the joint space. As these osteochondral fragments (often referred to as osteochondritis dissecans lesions) become loose in the joint, they can cause pain, locking, crepitance, and swelling.1,4,5
DIAGNOSIS
Clinical diagnosis of talar dome fractures can be highly challenging because there are no pathognomonic signs or symptoms.5 The patient may have sustained a fall or a twisting injury to the ankle and may generally ambulate with an antalgic gait. In the acute setting, the symptoms of a talar dome fracture are similar to and often occur with an ankle sprain.3,5
In lateral talar dome lesions, tenderness is generally found anterior to the lateral malle-oli, along the anterior lateral border of the talus.3,6 In medial talar dome lesions, tenderness is usually located posterior to the medial malleolus, along the posterior medial border of the talar dome.3,6 Chronic talar dome lesions—traumatic and atraumatic osteo-chondritis dissecans lesions—may have a clinical presentation similar to that of arthritis. Typical findings include crepitance, stiffness, and recurrent swelling with activity.5
Diagnosis of talar dome lesions can often be made with standard anteroposterior (AP), lateral, and mortise ankle radiographs. However, repeated radiographs may be necessary because initial films may appear normal. Secondary changes in the subchondral bone (visible on plain radiographs) caused by a compression fracture of the articular osteochondral surface may take weeks to appear.2,4 In addition, small chondral fragments are radiolucent and not evident on standard radiographs.
Generally, the AP ankle view is best for visualizing deep, cup-shaped medial lesions,1,4 although the lesions are often appreciated on the mortise view as well (Figure 3). Lateral lesions are best visualized on a mortise view and are generally thin and wafer-shaped.1,4 (Figure 4). If suggested by the clinical scenario, fractures not visualized with plain radiographs may require magnetic resonance imaging (MRI) or computed tomography (CT).6 The fracture classification developed by Berndt and Harty is widely used to stage talar dome lesions (Table 3).5


| Stage I | Compression fracture of subchondral bone |
| Stage II | Partial osteochondral fragment fracture |
| Stage III | Completely detached fragment without displacement |
| Stage IV | Completely detached fragment with displacement |
TREATMENT
An orthopedic surgeon should be consulted for treatment of talar dome lesions because of the high functional demands of for the talar dome and the potential for complications. Stage I, II, and III medial lesions can usually be treated nonsurgically with six weeks in a nonweight-bearing cast.1,3,5 Adequate reduction and immobilization are crucial for fracture healing and to avoid avascular necrosis of the fracture fragment.5
Lateral Process Fractures
The lateral talar process is an osseous protuberance that articulates superolaterally with the fibula, helping to stabilize the ankle mortise, and inferomedially with the calcaneus, forming the lateral portion of the subtalar joint7 (Figures 1 and 2). Lateral process fractures are the second most common talar fractures. From 33 to 41 percent of these fractures are missed on initial presentation.8–11 Traditionally, the causative injuries are falls, motor vehicle crashes, or direct trauma. Some recent reports7–9,12 implicate snowboarding accidents in these fractures.
DIAGNOSIS
Physical examination findings are similar to those in lateral ankle ligamentous injuries. Pain with plantar flexion, dorsiflexion, and subtalar joint movement is generally present.7 Although the normal anatomy of the ankle may be obscured by soft tissue swelling, a helpful diagnostic indicator is point tenderness over the lateral process. The lateral process can be palpated anteriorly and inferiorly to the tip of the lateral malleolus.8,11
TREATMENT
A nonweight-bearing, short leg cast can be used if anatomic position with less than 2 mm displacement can be maintained.7,11 A nonweight-bearing cast should be maintained for four to six weeks, followed by two weeks in a walking cast and initiation of rehabilitation exercises.7 For large and displaced fragments, the treatment of choice is usually surgical reduction and fixation.7,8
Posterior Process Fractures
The posterior process of the talus is composed of two tubercles, the lateral and medial (Figures 1 and 2). The lateral tubercle is the larger of the two and serves as the attachment of the posterior talocalcaneal and posterior talofibular ligaments.9,14,15 The medial tubercle serves as the attachment for the posterior third of the deltoid ligament.9,14,15 The under-surface of both tubercles forms the posterior fourth of the subtalar joint.9,14
Again, these fractures have been commonly misdiagnosed as ankle sprains.2,9,15,16 In one case series,15 17 of 20 patients with fractures were misdiagnosed with ankle sprains. Posterior process fractures can occur at either or both tubercles.14–18 Lateral and medial tubercle fractures are discussed separately.
FRACTURES OF THE POSTERIOR PROCESS: LATERAL TUBERCLE
Fractures of the lateral tubercle can be caused by hyperplantar flexion or inversion.1,2,15 Hyperplantar flexion injuries tend to cause compression fractures, while inversion injuries tend to produce avulsion fractures.1,2,15 Both of these injuries have been described after falls and have been associated with football and rugby kicking injuries, which place the ankle in a forced plantar flexed position.19 If present, an os trigonum can be injured by the same mechanisms described above.2,19
Diagnosis
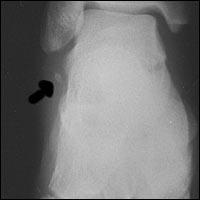
Clinically, patients with a fracture of the lateral tubercle present with pain and swelling in the posterolateral area of the ankle. The pain is often exacerbated by activities requiring plantar flexion.15 Physical examination findings in lateral tubercle fractures of the posterior process are highly consistent for tenderness to deep palpation anterior to the Achilles tendon over the posterior talus. The pain is often reproduced with plantar flexion and occasionally accentuated with dorsiflexion of the great toe. This is caused by compression of the fracture fragment as the flexor hallucis longus tendon passes between the medial and lateral tubercle.15
A lateral radiograph of the foot usually best visualizes the lateral tubercle and, if present, the os trigonum.6,9 When evaluating the fracture line, a rough, irregular cortical surface suggests the presence of an acute fracture (Figure 6). In acute injuries, this rough irregular surface may help distinguish a fracture from a normal os trigonum, which generally has a smooth, rounded cortical surface.15 In chronic cases, these differences may be less distinct, making the distinction between a fracture and a normal os trigonum difficult. When the diagnosis is unclear and clinical suspicion is present, an MRI or CT will clearly demonstrate this fracture.16

Treatment
Nondisplaced or minimally displaced fractures can be treated with a non-weight-bearing, short leg cast for four to six weeks.9,15 After this period of immobilization, weight bearing is allowed as tolerated. If symptoms persist, an additional four to six weeks of immobilization would be recommended.6 If the fracture site continues to be symptomatic after six months, fragment excision is usually curative.6,9 Larger and more displaced fractures may require open reduction internal fixation.6,16
FRACTURES OF THE POSTERIOR PROCESS: MEDIAL TUBERCLE
Diagnosis
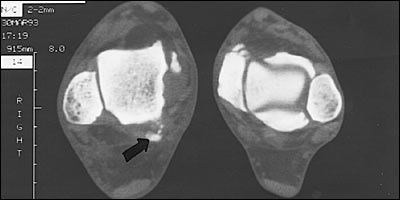
Visualization of the medial tubercle fracture on plain radiograph may be challenging, but the fracture can generally be seen on an oblique projection with the foot and ankle externally rotated 40 degrees and the beam centered 1 cm posterior and inferior to the medial malleolus16,17 (Figure 7). However, CT (Figure 8) or MRI may be necessary if the diagnosis is unclear.16,17

Treatment
Fracture of the Anterior Process of the Calcaneus
The anterior process of the calcaneus is a saddle-shaped bony protuberance that articulates with the cuboid. It is attached to the cuboid by an interosseous ligament and to the cuboid and navicular bones by the strong bifurcate ligament21,22 (Figures 1 and 2). Fractures of the anterior process account for approximately 15 percent of all calcaneal fractures and are commonly misdiagnosed as ankle sprains.6,21,23,24
Anterior process fractures secondary to compression generally occur when the foot is forcefully dorsiflexed and the anterior process is pressed against the cuboid.22 Because of the energy involved with this mechanism, anterior process fractures secondary to compression are often intra-articular and are commonly associated with other fractures.7,23
DIAGNOSIS
Patients with anterior process fractures generally have a history of a previous inversion injury or involvement in a motor vehicle crash.21 Clinically, patients generally show signs and symptoms similar to those of a lateral ankle sprain.21,23 The pain may be minimal with standing but increases substantially with ambulation.21,23 An important diagnostic feature is point tenderness over the calca-neocuboid joint that is localized approximately 1 cm inferior and 3 to 4 cm anterior to the lateral malleolus, just distal to the anterior talofibular ligament insertion.21,22,23 Careful assessment of the point of maximal tenderness may help differentiate this fracture from a lateral ligament sprain.21,23
Although this fracture can be difficult to assess on routine radiographs of the foot and ankle, a careful inspection of the lateral view of the calcaneus often reveals this subtle fracture21,24 (Figure 9). As the clinical scenario dictates, a CT scan or MRI may be necessary.9,21,23 In addition, an accessory ossicle (calcaneus secondarium) maybe located near the anterior process and could be misinterpreted as a fracture.21,24

TREATMENT
Although fracture healing may appear radiographically to be complete, approximately 25 percent of patients require more than a year before becoming asymptomatic.21 Following nonsurgical management, most patients report satisfactory results and a return to preinjury activity levels.21,23,24 Symptomatic nonunions or large, displaced fractures may require surgical intervention.21,24
Final Comment
The fractures discussed here can be serious injuries and cause prolonged disability. In general, extra-articular fractures of the talus and calcaneus can be managed with nonsurgical treatment. However, intra-articular fractures require special attention to ensure that the articular surface is restored to anatomic congruity and that the correct mechanical alignment is maintained. This step optimizes the chance for a full recovery and decreases the incidence of post-traumatic arthritis and associated morbidities.
Appropriate radiographs are essential to the diagnosis of these fractures but, in the work-up of an ankle injury, radiographs are not always required. The Ottawa ankle rules (Figure 1025 ) offer the physician clinical guidance as to which injuries require radiographs. Prospective studies have validated the effectiveness of these guidelines and shown the rules to be 100 percent sensitive for clinically significant fractures.25,26
Although fractures of the talus were vary rarely encountered in the Ottawa ankle trials, the fractures discussed in this article would likely be identified using the Ottawa ankle rules, because of the inability of the patient to bear weight after the injury and during the examination.
Nevertheless, some patients with these fractures are able to ambulate and, because patients with these fractures generally do not present with tenderness along the posterior border of the lateral or medial malleolus, radiographic evaluation may not be indicated under the Ottawa guidelines. However, as with all guidelines, clinical judgment and experience may be grounds for radiographic analysis in unique cases. Furthermore, in the case of a suspected ankle sprain that does not improve as expected or is accompanied by tenderness over a potential fracture site, radiographic analysis at a follow-up evaluation may be indicated. The fracture may then be diagnosed and treated soon enough after the injury to avoid an adverse prognosis.