
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2002;66(7):1259-1267
The purposes of electrosurgery are to destroy benign and malignant lesions, control bleeding, and cut or excise tissue. The major modalities in electrosurgery are electrodesiccation, fulguration, electrocoagulation, and electrosection. Electrosurgery can be used for incisional techniques that produce full-thickness excision of nevi, for shave techniques that produce partial-thickness removal of superficial lesions, and for removing vascular lesions such as hemangiomas or pyogenic granulomas. The correct output power can be determined by starting low and increasing the power until the desired outcome is attained (destruction, coagulation, or cutting). Smaller cherry angiomas can be electrocoagulated lightly. Larger cherry angiomas may be easier to treat by shaving them first, then electrocoagulating or desiccating the base. The elevated portion of pyogenic granulomas can be shaved off with a scalpel or a loop electrode using a cutting/coagulation current. The base of the lesion is curetted to remove the remaining tissue and then electrodesiccated. Complications such as burns, shocks, and transmission of infection can be prevented by careful use of the electrosurgical equipment.
Electrosurgery is used to destroy benign and malignant lesions, to control bleeding, and to cut or excise tissue.1–3 Electrosurgery is simple to perform and is useful for treating a variety of skin lesions, especially small superficial lesions (skin tags and small angiomas). The major modalities in electrosurgery are electrodesiccation, fulguration, electrocoagulation, and electrosection.
Modern, high-frequency electrosurgical devices transfer electrical energy to human tissue via a treatment electrode that remains cool. Most electrosurgical units work at frequencies just below the AM radio frequency band. The electrical resistance of human tissue helps convert this electrical energy into molecular energy, which causes denaturation of intracellular and extracellular proteins, resulting in coagulation or desiccation effects. Raising intracellular water above the boiling point causes cell membrane rupture to produce a cutting effect.
Electrosurgery has many applications in cutaneous surgery: incisional techniques that produce full-thickness excision of nevi; shave techniques that produce partial-thickness removal of superficial lesions, such as warts, without the need for suturing; and removal of vascular lesions such as hemangiomas or pyogenic granulomas with little or no blood loss. Electrosurgery has become familiar to family physicians who treat cervical dysplasia using the technique of loop excision of the transformation zone of the cervix. This technique is performed using the same electrosurgical equipment and procedures as in skin surgery.
Electrosurgery is often incorrectly referred to as electrocautery. In electrocautery, the electrode tip, rather than human tissue, serves as the source of electrical resistance. In electrocautery, the electrode tip becomes hot and can cause a burn in tissue. While electrocautery is a form of electrosurgery, it is inaccurate to refer to electrosurgical techniques that use a cool electrode tip as electrocautery.
Electrodesiccation and Fulguration
In electrodesiccation, an active electrode touches or is inserted into the skin to produce tissue destruction (Figure 1, part A). Electrodesiccation can be used to treat fine telangiectasias and spider angiomas.
In fulguration, the electrode is held away from the skin to produce a sparking at the skin surface and more shallow tissue destruction (Figure 1, part B). Fulguration is especially useful in treating superficial epidermal lesions, such as a superficial basal cell carcinoma of the trunk.
Electrocoagulation
Electrocoagulation is ideal for clotting small blood vessels (less than 2 to 3 mm in diameter) in deep and superficial surgery. Usually, a 2- to 5-mm metallic sphere at the end of a treatment electrode is the optimal tip for hemostasis of small vessels. These electrode tips can be directly applied to the relatively dry surface of a surgical bed that has been momentarily compressed or used indirectly by touching a hemostat or Adson’s forceps which is used to grasp the small bleeder.
Electrosection
In electrosection, the electrode is used to cut tissue. An electrode tip in the shape of a fine needle, wire loop, diamond, ellipse, or triangle is advanced slowly through the tissue, causing a steam envelope to advance around the tip and producing a smooth cutting effect with little sense of pressure against the tissue by the operator.
This minimization of power produces a specimen with minimal heat damage along its margins and clinical wound healing the same as when surgical steel blades are used. The specimen should be acceptable for pathologic interpretation compared with specimens produced with laser techniques. Wound edges can be approximated with sutures when an excisional biopsy is performed. Cosmetic results are similar to those seen with scalpel and suturing.
Dispersive Electrodes
Electrodesiccation and fulguration are monoterminal techniques because they can be accomplished using a single treatment electrode on the patient. Electrosection is a biterminal technique because it requires two electrodes. To efficiently perform cutting using the smallest power settings in electrosection, the current delivered by the treatment electrode needs to return to the generator. This is accomplished by means of a second electrode (referred to as a dispersive, return, or indifferent electrode) placed in contact with the patient (or in the case of the highest frequency units, near the patient).
Blended or ‘Cut and Coag’ Currents
Some of the major advantages of electrosection are the capability of performing nearly bloodless surgery and decreasing treatment time. Decreasing blood loss is best accomplished by blending electrosection and electrocoagulation currents, producing a partially dampened current that retains excellent cutting ability and coagulating capacity. Blended currents allow the operator to treat multiple lesions at one sitting with little blood loss and to do so more rapidly than scalpel techniques. Electrosection is the preferred electrosurgical modality for an elliptical excision of a skin lesion.
Table 1 lists skin lesions that are treatable with electrosurgery techniques. Contraindications to treatment include use of a pacemaker and the treatment of melanoma. Current procedural terminology (CPT) codes for electro-surgical treatment of skin lesions are listed in Table 2. Table 34,5 is a summary of the methods for preventing complications of electrosurgery.
| Type of lesion | Technique |
|---|---|
| Benign lesions | |
| Acrochordons (skin tags) | D, S |
| Angiomas, cherry | C, D |
| Angiomas, spider | C |
| Condyloma acuminatum | D |
| Molluscum contagiosum | D |
| Nevi | S |
| Pyogenic granulomas | S, C |
| Seborrheic keratosis | D |
| Sebaceous hyperplasia | C |
| Telangiectasias | C |
| Verrucae vulgaris | D |
| Verrucae plana | D |
| Premalignant lesions | |
| Actinic keratosis | D |
| Malignant lesions | |
| Basal cell carcinoma | S, D |
| Size of lesions | |||||
|---|---|---|---|---|---|
| CPT code | Procedure | Number of lesions | 0.5 cm | 0.6 to 1.0 cm | 1.1 to 2.0 cm |
| 11200* | Removal of skin tags | Up to 15 | |||
| 11201† | Removal of skin tags | Each additional 10 | |||
| 11400 | Excision, benign lesion: trunk, arms or legs | Each | X | ||
| 11401 | Each | X | |||
| 11402 | Each | X | |||
| 11420 | Excision, benign lesion: scalp, neck, hands, feet, genitalia | Each | X | ||
| 11421 | Each | X | |||
| 11422 | Each | X | |||
| 11440 | Excision, benign lesion: face, ears, eyelids, nose, lips, mucous membrane | Each | X | ||
| 11441 | Each | X | |||
| 11442 | Each | X | |||
| 11600 | Excision, malignant lesion: trunk, arms or legs | Each | X | ||
| 11601 | Each | X | |||
| 11602 | Each | X | |||
| 11620 | Excision, malignant lesion: scalp, neck, hands, feet, genitalia | Each | X | ||
| 11621 | Each | X | |||
| 11622 | Each | X | |||
| 11640 | Excision, malignant lesion: face, ears, eyelids, nose, lips, | Each | X | ||
| 11641 | Each | X | |||
| 11642 | Each | X | |||
| 17000* | Destruction, benign lesion: any method | 1st | |||
| 17003† | Destruction, benign lesion: any method | 2 to 14 | |||
| 17004ठ| Destruction, benign lesion: any method | 15 or more | |||
| Complications | Prevention |
|---|---|
| Burns | Avoid preparing the skin with alcohol, or let it dry thoroughly. |
| Do not use ethyl chloride as a topical anesthetic. | |
| Do not use oxygen simultaneously. | |
| Do not place dispersive electrode under a bony prominence. | |
| Shocks | Use a three-pronged receptacle that is not overloaded. |
| Do not use the treatment table outlet. | |
| Make sure the patient is not grasping or touching metal parts of the treatment table. | |
| The operator should not make or break contact with the patient during the delivery of the current. | |
| Transmission of infection* | Use a smoke evacuator with the intake nozzle held within 2 cm of the operative area. |
| The operators should consider wearing surgical masks and eye protection when working on lesions that contain HPV. | |
| Pacemaker problems† | Consider thermal pencil cautery. |
| Investigate risk of arrhythmia with the patient’s specific pacemaker. | |
| Eye injury | Use special care when performing electrosurgery near the eye. |
| Do not let the active tip of your electrosurgical device get close to the eye because the spark can arc to the globe and cause damage. |
Selecting Equipment
When choosing an electrosurgical unit, the following questions need to be addressed:
WILL THE UNIT BE USED FOR ELECTROSECTION AND CUTTING TECHNIQUES?
If so, then you must select equipment capable of biterminal technique using a dispersive electrode (not to be confused with bipolar, which refers to the use of electrosurgical forceps where both tips are energized).
WHAT SAFETY FEATURES ARE AVAILABLE?
There should be a visible light and audible warning when the treatment electrode is energized. Units are either foot-pedal operated, have a switch on the handpiece, or have capabilities for both.
WHAT IS THE COST OF PURCHASING AND OPERATING THE UNITS?
An office electrosurgical unit will cost between $1,500 and $2,500 and will include a set of several treatment tips. Additionally, a smoke evacuator will cost $500 to $1,000. The smoke evacuator helps reduce the minimal infectious risk by reducing exposure to the smoke plume, and it reduces the unpleasant odor of electrosurgically treated human tissue in an office that may not be well ventilated.
Availability of reusable tips, dispersive electrodes, and handpieces is also a consideration in selecting equipment. The cost of disposable treatment tips, handpieces, and dispersive electrodes frequently exceeds the reimbursement available for the procedure.
WHAT ARE THE POLICIES, WARRANTIES, AND REPUTATION OF THE EQUIPMENT MANUFACTURER?
Desirable policies of the equipment manufacturer include: a toll-free repair line staffed at least five days a week; the availability of equipment for loan during repair; and at least a two-year warranty on the equipment.
Anesthesia
Injectable lidocaine is administered before most electrosurgical techniques. The use of lidocaine with epinephrine further reduces blood loss, but the use of epinephrine at the tips of digits and the nose should be avoided. Anesthesia may not be necessary for electrosurgery for small lesions such as telangiectasias and small skin tags. Consider the patient’s preference, because short bursts of low power current may be less uncomfortable than injected anesthesia for some persons. When anesthesia is not used for small lesions, it is helpful to stabilize the hand by holding the device against the patient’s body or face so that if the patient moves, the electrode moves with the patient. Another alternative is to use a eutectic mixture of local anesthetics (EMLA) cream, which contains 2.5 percent lidocaine and 2.5 percent prilocaine. The patient should apply EMLA cream under occlusion to skin at least one hour before the procedure to achieve topical anesthesia.
POWER SETTING
Choose the correct output power by starting low and increasing the power until the desired outcome is attained (destruction, coagulation, or cutting). Power requirement varies in accordance with several factors. The closer the dispersive electrode is to the treatment site and the smaller the surface area of the treatment electrode, the lower the power requirements. Generally, coagulation requires higher power settings than cutting, which requires higher power settings than desiccation/fulguration. Power settings for treating cutaneous lesions are generally low (10 to 20 watts).
Detailed Descriptions of Electrosurgery
CHERRY ANGIOMAS
Cherry (also known as capillary or senile) angiomas (Figure 2) are cosmetic lesions that are asymptomatic and have no malignant potential. If the patient requests treatment, electrosurgery is probably the most effective and inexpensive technique. Larger cherry angiomas may be easier to treat by shaving them first and then electrocoagulating or desiccating the base. Smaller cherry angiomas can be electrocoagulated lightly. Any significant remaining char may be wiped off with gauze or a curette.

PYOGENIC GRANULOMA
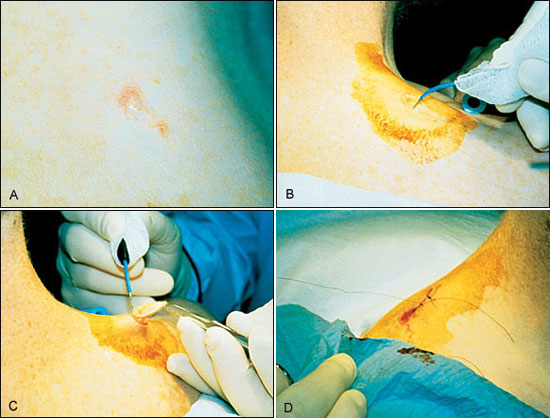
Electrosurgical treatment is ideal for pyogenic granulomas, (Figure 3) which are very vascular, benign tumors. The procedure should not begin for at least 10 minutes after the injection of local anesthesia to maximize the benefit of the epinephrine for vasoconstriction. First, the elevated portion of the lesion should be shaved off with a scalpel or a loop electrode using a cutting/coagulation current. The specimen should be sent for pathology to eliminate the possibility that the lesion is amelanotic melanoma. The base of the lesion should be scraped with a 2-0 to 3-0 sharp dermal curette to remove the remaining tissue. Before an attempt is made to stop the bleeding with electrosurgery, the base should be dried with pressure from cotton swabs because pooled blood will diminish the efficacy of electrosurgery. Finally, the base of the lesion is electrocoagulated. The curettage and coagulation may need to be repeated several times to destroy the whole pyogenic granuloma and stop the bleeding.

BASAL CELL CARCINOMA
After the administration of local anesthesia, the basal cell carcinoma should be scraped out using a sharp dermal curette such as a 2-0 or 3-0. Removing the abnormal tissue by scraping with the curette in all directions increases the likelihood of getting the small pockets of tumor. Using the curette on the border of the basal cell carcinoma will help to obtain the rim of outlying tissue. This procedure is effective because the basal cell carcinoma is softer than the surrounding normal skin. Next, the base should be fulgurated or desiccated, leaving a 2-mm margin of normal tissue. The cycle should be repeated three times to diminish the recurrence rate.
An alternative approach to management of basal cell carcinoma is an elliptical excision (Figure 4). This should be a full-thickness excision, followed by suturing of the wound margins as with scalpel excision. A major advantage of elliptical excision via electrosection is the absence of appreciable bleeding from the wound.
Reasons to Refer to a Skin Surgery Sub-Specialist
The five principal situations that should prompt a referral to a skin surgery sub-specialist are patients who have: (1) a large lesion; (2) a lesion located in a sensitive area (cosmetic or functional); (3) a lesion that is beyond the scope of the physician’s skill; (4) aggressive skin cancer; and (5) a higher chance of having a complication or who may require close monitoring during or after surgery.
Wound Care
Two common types of skin wounds that result from electrosurgery are partial-and full-thickness wounds. Partial-thickness wounds result from the electrodesiccation of epidermal lesions and the curettage and desiccation of basal cell carcinomas. These wounds heal by secondary intention and may be cleansed daily and then covered with petrolatum or antibiotic ointment. These ointments promote a moist environment for new tissue growth and have been proven safe and effective.6 The wound may then be covered with typical adhesive bandages. Full-thickness wounds need to be closed with sutures.
Electrosurgery is often used for incision of the ellipse and electrocoagulation of bleeding in subcutaneous tissues during elliptical, full-thickness excisions. These wounds are then sutured and can be cared for the same as above.
Training
The American Academy of Family Physicians and several private organizations offer basic, one- to three-hour training sessions in electrosurgery. After this basic introduction, the physician should practice on beefsteak or other animal meat models to develop a familiarity with the electrosurgical equipment.
A physician experienced in electrosurgical techniques can serve as a preceptor to help other physicians enhance their electrosurgery skills. Physicians should begin treatment of skin lesions on the trunk rather than the upper thorax where hypertrophic scars are more likely to form.