
Am Fam Physician. 2002;66(8):1497-1501
A patient information handout on knee joint aspiration and injection is provided on page 1511.
Knee joint aspiration and injection are performed to aid in diagnosis and treatment of knee joint diseases. The knee joint is the most common and the easiest joint for the physician to aspirate. One approach involves insertion of a needle 1 cm above and 1 cm lateral to the superior lateral aspect of the patella at a 45-degree angle. Once the needle has been inserted 1 to 1½ inches, aspiration aided by local compression is performed. Local corticosteroid injections can provide significant relief and often ameliorate acute exacerbations of knee osteoarthritis associated with significant effusions. Among the indications for arthrocentesis are crystal-induced arthropathy, hemarthrosis, unexplained joint effusion, and symptomatic relief of a large effusion. Contraindications include bacteremia, inaccessible joints, joint prosthesis, and overlying infection in the soft tissue. Large effusions can recur and may require repeat aspiration. Anti-inflammatory medications may prove beneficial in reducing joint inflammation and fluid accumulations.
Knee joint aspiration and injection are performed to establish a diagnosis, relieve discomfort, drain off infected fluid, or instill medication. Because prompt treatment of a joint infection can preserve the joint integrity, any unexplained monarthritis should be considered for arthrocentesis (Table 1).
Arthrocentesis also may help distinguish the inflammatory arthropathies from the crystal arthritides or osteoarthritis. If a hemarthrosis is discovered after trauma, it can indicate the presence of a fracture or other anatomic disruption.
The knee is the most common and the easiest joint for the physician to aspirate. It was chosen for discussion here because of the frequent clinical problems associated with this joint. The indications, complications, and pitfalls for knee arthrocentesis generally can be applied to other joints (Tables 2 and 3). Many of the principles of needle aspiration and injection also can be used for soft tissue disorders, such as bursitis or tendinitis.
An effusion of the knee often produces detectable suprapatellar or parapatellar swelling. Large effusions can produce ballottement of the patella. Medial or lateral approaches to the knee can be selected; some investigators advocate the medial approach when the effusion is small and the lateral approach with larger effusions. The knee generally is easiest to aspirate when the patient is supine and the knee is extended.
Corticosteroids are believed to modify the vascular inflammatory response to injury, inhibit destructive enzymes, and restrict the action of inflammatory cells. Intrasynovial steroid administration is designed to maximize local benefits and minimize systemic adverse effects. Local corticosteroid injections can provide significant relief and often ameliorate acute exacerbations of knee osteoarthritis associated with significant effusions.
| Crystal-induced arthropathy |
| Hemarthrosis |
| Limiting joint damage from an infectious process |
| Symptomatic relief of a large effusion |
| Unexplained joint effusion |
| Unexplained monarthritis |
There is no convincing evidence that corticosteroids modify rheumatic joint destruction, and steroid injections in patients with rheumatoid arthritis should be considered ancillary to rest, physical therapy, nonsteroidal anti-inflammatory drugs (NSAIDs), or disease-modifying antirheumatic drugs.
| Adjacent osteomyelitis |
| Bacteremia |
| Hemarthrosis |
| Impending (scheduled within days) joint replacement surgery |
| Infectious arthritis |
| Joint prosthesis |
| Osteochondral fracture |
| Periarticular cellulitis |
| Poorly controlled diabetes mellitus |
| Uncontrolled bleeding disorder or coagulopathy |
Judicious use of corticosteroids rarely produces significant adverse effects. The introduction of infection after injection is believed to occur in less than 1 in 10,000 procedures. The concept of steroid arthropathy is largely based on studies in subprimate animal models, and it is an unusual occurrence in humans if the number of injections is limited to three to four per year in weight-bearing joints. More conservative researchers have even advocated limiting knee injections to three or four over an individual's lifetime.
Methods and Materials
PATIENT PREPARATION
Clothing is removed from over the affected joint. The patient is placed in the supine position, and the knee is extended (some physicians prefer to have the knee bent to 90 degrees). An absorbent pad is placed beneath the knee.
EQUIPMENT
Sterile Tray for the Procedure
Place the following items on a sterile sheet covering a Mayo stand:
Sterile gloves
Sterile fenestrated drape
2 10-mL syringes
2 21-gauge, 1-inch needles
1 inch of 4 × 4 gauze soaked with povidone-iodine solution (Betadine)
Hemostat (for stabilizing the needle when exchanging the medication syringe for the aspiration syringe)
Sterile bandage
Procedure Description
The patient is supine on the table with the knee extended (some physicians prefer that the knee be bent to 90 degrees). Some physicians prefer the medial approach for smaller effusions, but the lateral approach will be discussed here. The knee is examined to determine the amount of joint fluid present and to check for overlying cellulitis or coexisting pathology in the joint or surrounding tissues.
The superior lateral aspect of the patella is palpated. The skin is marked with a pen, one fingerbreadth above and one fingerbreadth lateral to this site. This location provides the most direct access to the synovium.
The skin is washed with povidone-iodine solution. The physician should be gloved, although there is no consensus as to whether sterile gloves must be used. A 21-gauge, 1-inch needle is attached to a 5- to 20-mL syringe, depending on the anticipated amount of fluid present for removal.
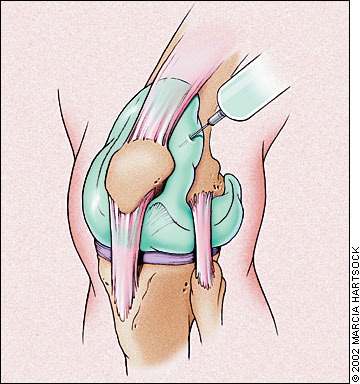
The needle is inserted through stretched skin. Some physicians administer lidocaine (Xylocaine) into the skin, but stretching the pain fibers in the skin with the nondominant hand can also reduce needle-insertion discomfort. The needle is directed at a 45-degree angle distally and 45 degrees into the knee, tilted below the patella (Figure 1).
Once the needle has been inserted 1 to ¼ inches, aspiration is performed, and the syringe should fill with fluid. Using the nondominant hand to compress the opposite side of the joint or the patella may aid in arthrocentesis.
Once the syringe has filled, a hemostat can be placed on the hub of the needle. With the needle stabilized with the hemostat, the syringe can be disconnected and the fluid sent for studies. Care should be taken not to touch the needle tip against the joint surfaces when removing the syringe. A syringe filled with corticosteroid medication can then be attached to the needle.
For injection, use betamethasone (Celestone, 6 mg per mL), 1 mL, mixed with 3 to 5 mL of 1 percent lidocaine. Alternately, methylprednisolone (Depo-Medrol, 40 mg per mL), 1 mL, mixed with 3 to 5 mL of 1 percent lidocaine can be used. After injection of the medication, the needle and syringe are withdrawn.
The skin is cleansed, and a bandage is is applied over the needle-puncture site. The patient is warned to avoid forceful activity on the joint while it is anesthetized.
| Bacteremia |
| Clinician unfamiliar with anatomy of or approach to the joint |
| Inaccessible joints |
| Joint prosthesis |
| Overlying infection in the soft tissues |
| Severe coagulopathy |
| Severe overlying dermatitis |
| Uncooperative patient |
Follow Up
After diagnostic arthrocentesis, appropriate intervention usually will be dictated by the results of the fluid analysis. Joint infections are usually treated aggressively with intravenous antibiotics. An inflammatory arthritis, such as rheumatoid arthritis, can be treated with disease-modifying medications such as methotrexate or penicillamine. Patients with traumatic or bloody effusions may be considered for further orthopedic evaluation.
Large effusions can recur and may require repeat aspiration. Anti-inflammatory medications may prove beneficial in reducing joint inflammation and fluid accumulations.
Corticosteroid injections for osteoarthritis often provide a short-lived benefit. Repeat injections can be considered after six weeks. Large, weight-bearing joints should not be injected more than three times a year.
Procedure Pitfalls/Complications
The Patient Complains of Severe Pain During the Procedure. Severe pain during the procedure usually results from the needle coming into contact with the highly innervated cartilaginous surfaces. The needle can be redirected or withdrawn when pain is encountered. Slow, steady movement of the needle during insertion can prevent damage to the cartilage surface from the needle bevel.
The Patient's Effusion Was Sterile, But Became Infected After the Joint Injection. Introduction of infection into a joint is a rare event, occurring in less than 0.01 percent of injections; however, infection can develop when the needle is introduced into the joint through an area of cellulitis. Severe dermatitis or soft tissue infection overlying a joint is a contraindication for arthrocentesis. Some physicians advocate that steroid injection should not be performed before excluding joint infection.
The Patient Complains That the Joint Hurts Much Worse the Day After the Injection Than It Did Before the Injection. A recognized complication of steroid injections to joints is the postinjection flare. The flare reaction represents an increase in joint pain occurring in 1 to 2 percent of persons. The steroid crystals can induce an inflammatory synovitis that usually begins about six to 12 hours after the injection. The postinjection flare can present with swelling, tenderness, and warmth over the joint that persists for hours or days. If the patient takes anti-inflammatory medications immediately after the injection, they may reduce or abort this reaction. Aspiration should be performed to rule out joint sepsis if symptoms persist beyond two to three days.
The Patient Develops Joint Instability From Repeated Injections. The most serious complication of repeated injections is joint instability from the development of osteonecrosis of juxta-articular bone and weakened capsular ligaments. Although this complication occurs in less than 1 percent of patients, it is recommended that injections be performed no more frequently than every six to eight weeks, and no more than three times per year in weight-bearing joints.
A Large Knee Effusion Re-accumulated Right After Being Drained. Large effusions from the knee can rapidly re-accumulate. Some physicians advocate placing an elastic wrap around the knee immediately after large effusion drainage.
The Patient's Pain Returned Just a Few Weeks After the Injection. A major disadvantage to intra-articular corticosteroid injections is the short duration of action. The average duration of benefit may be only two to three weeks; however, a small percentage of patients with osteoarthritis may have sustained relief after one or two injections.
Physician Training
Experience is important for the proper performance of joint aspiration and injection procedures. Physicians skilled in arthrocentesis usually have had the opportunity to gain experience with a rheumatologist or other physician who performs many procedures. Each joint has different anatomic landmarks, and novice physicians may need to review a textbook for approaches to an unfamiliar joint. Although arthrocentesis is a simple technique with minimal risk, physicians should have assistance or supervision with their first attempts at any site. Family physicians wanting to perform arthrocentesis on deep joints, such as the hip or vertebral joints, should obtain extensive training in these higher risk procedures. Additional training in arthrocentesis is available from the American Academy of Family Physicians.