
Am Fam Physician. 2002;66(10):1882-1887
Sinusitis is one of the most common diseases treated by primary care physicians. Uncomplicated sinusitis does not require radiologic imagery. However, when symptoms are recurrent or refractory despite adequate treatment, further diagnostic evaluations may be indicated. Plain radiography has a limited role in the management of sinusitis. Although air-fluid levels and complete opacification of a sinus are more specific for sinusitis, they are only seen in 60 percent of cases. Noncontrast coronal computed tomographic (CT) images can define the nasal anatomy much more precisely. Mucosal thickening, polyps, and other sinus abnormalities can be seen in 40 percent of symptomatic adults; however, clinical correlation is needed to avoid overdiagnosis of sinusitis because of nonspecific CT findings. Use of CT is typically reserved for difficult cases or to define anatomy prior to sinus surgery. Magnetic resonance imaging (MRI) cannot define bony anatomy as well as CT. MRI is only used to differentiate soft-tissue structures, such as in cases of suspected fungal infection or neoplasm. Referral will occasionally be needed in unusual or complicated cases. Immunocompromised persons and smokers are at increased risk for serious sinusitis complications.
Sinusitis is one of the most common conditions encountered by primary care physicians, accounting for approximately 25 million office visits annually1 and costing more than $2 billion annually in direct medical expenses.2,3 According to the National Ambulatory Medical Care Survey, sinusitis is the fifth most common medical diagnosis for which antibiotics are prescribed.4,5
Advances in diagnostic imaging techniques (e.g., computed tomographic [CT] scan and magnetic resonance imaging [MRI]) have enhanced the understanding and management of sinusitis. Diagnostic imaging is generally used in cases of recurrent or complicated sinus disease. Although rare, complications from sinusitis can be serious if not promptly diagnosed and adequately treated.
Plain Radiography
Plain radiography has a limited role in the management of sinusitis. Possible findings in acute sinusitis include mucosal thickening, air-fluid levels, and complete opacification of the involved sinus. Although mucosal thickening is seen in more than 90 percent of sinusitis cases, it is very nonspecific.6–8 Air-fluid levels and complete opacification are more specific for sinusitis but are seen in only 60 percent of sinusitis cases.6 Interpretation of plain radiographs can vary widely among different observers, and there is a high rate of false-negative results.2,9
Radiographs of the sinuses in infants aged three years or younger are not useful because of false “opacification” from undeveloped sinuses.10 Other important limitations of plain radiographs include poor visualization of ethmoid air spaces and difficulty differentiating between infection, tumor, and polyp in an opacified sinus.2
Because clinical judgment is sufficient to diagnose sinusitis in a majority of cases, and empiric treatments are inexpensive and safe, only a small percentage of patients who develop recurrent or complicated sinusitis are candidates for imaging studies. Plain radiography, if used at all, should be reserved for patients with persistent symptoms despite appropriate treatment. A single Waters' view (occipitomental) appears to provide as much information as the standard four-view series.11
CT Scan
CT scans can provide much more detailed information about the anatomy and abnormalities of the paranasal sinuses than plain films.12 A CT scan provides greater definition of the sinuses and is more sensitive than plain radiography for detecting sinus pathology, especially within the sphenoid and ethmoid sinuses.6,13 CT scan findings can also be quite nonspecific, however, and should not be used routinely in the diagnosis of acute sinusitis.6,14 The primary role of CT scans is to aid in the diagnosis and management of recurrent and chronic sinusitis, or to define the anatomy of the sinuses prior to surgery.2 In many institutions, a limited CT scan costs about the same as a full radiographic series but provides more useful information.2,15,16
A coronal CT image is the preferred initial procedure. Bone window views provide excellent resolution and a good definition of the complete osteomeatal complex and other anatomic details that play a role in sinusitis.2 The coronal view also correlates best with findings from sinus surgery. A noncontrast CT scan is usually sufficient, except for complicated acute sinusitis (e.g., periorbital cellulitis or abscess). Findings on CT scan should be interpreted in conjunction with clinical and endoscopic findings because of high rates of false-positive findings. Up to 40 percent of asymptomatic adults have abnormalities on sinus CT scans, as do more than 80 percent of those with minor upper respiratory tract infections.14
MRI
MRI allows better differentiation of soft tissue structures within the sinuses. It is used occasionally in cases of suspected tumors or fungal sinusitis.17–19 Otherwise, MRI has no advantages over CT scanning in the evaluation of sinusitis. Disadvantages of MRI include high false-positive findings, poor bony imaging, and higher cost. MRI scans take considerably longer to accomplish than CT scans and may be difficult to obtain in patients who are claustrophobic.
Considerations for Referral
The most common reason referral for sub-specialty care is considered is failure of medical management for chronic or recurrent sinusitis. Persistent or progressive symptoms after maximal medical therapy, in combination with CT evidence of paranasal sinus disease, should prompt referral. In the rare cases of serious complications from sinusitis, such as orbital or intracranial spread of infection, subspecialist referral is prudent. Immuno-compromised patients are at increased risk for complicated bacterial or fungal infections. Sinonasal cancers are quite uncommon, with an annual incidence of less than 1:100,000 in the United States. Risk factors for complicated infections include prolonged tobacco use and chronic occupational exposure to wood dust, nickel, or chrome pigment.
Clinical Cases of Complication
CASE 1
The patient is a 37-year-old man who smokes. He has a history of bilateral nasal obstruction and facial pressure pain over a number of years. Frontal headaches and purulent nasal drainage have been present intermittently for years. He received multiple courses of oral antibiotics, nasal steroids, and decongestants, with only temporary relief. Two pulses of oral steroids produced a prolonged response that was again only temporary. There was no seasonal variation to his symptoms, and allergy testing was negative.
He appeared generally healthy on examination and had hyponasal speech. His ears were clear bilaterally. Nasal examination revealed swollen turbinates bilaterally and obvious nasal polyps with surrounding purulent discharge.
The patient was started on a four-week course of broad-spectrum antibiotics in combination with an oral steroid pulse. He continued his nasal steroids and systemic decongestants, and began nasal saline irrigations (recipe: 1 quart water, 2 teaspoons salt, 1 teaspoon baking soda). After this treatment, his symptoms improved approximately 50 percent, and he received a limited CT scan of the sinuses. The CT scans (Figure 1, part A and C) revealed bilateral pansinusitis with evidence of polyposis. He also had a large air cell (i.e., con-cha bullosa) within the left middle turbinate, which likely contributed to obstruction of ostia draining adjacent sinuses (Figure 1, part B). The patient underwent endoscopic sinus surgery with improvement of his symptoms.

CASE 2
The patient is a 20-year-old healthy man with an upper respiratory tract infection that has lasted two weeks. He progressed to an acute sinusitis with associated fevers and left facial pressure, pain, and swelling. His nasal symptoms improved after he started taking decongestants and antibiotics, but a persistent headache prompted a visit back to his family physician.
He had left maxillary and frontal tenderness to palpation on examination. His ears were clear by otoscopy, and his nasal examination revealed a right-sided septal deviation.
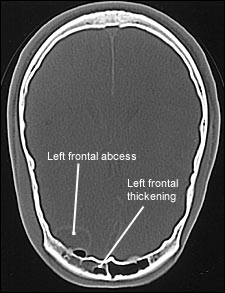
Because of the progression of his headaches, a maxillofacial and head CT scan was obtained, revealing acute sinusitis with frontal epidural abscess (Figure 2).
He was started on intravenous antibiotics and underwent external frontal sinusotomy to decompress the adjacent infected frontal sinus. After a prolonged course of antibiotics, serial CT scans revealed resolution of the frontal abscess and sinusitis. He subsequently underwent a successful frontal sinus obliteration to prevent future episodes of frontal sinusitis.
CASE 3
The patient is a 45-year-old healthy white man with longstanding right-sided nasal obstruction associated with postnasal discharge and cheek pressure. He recently developed intermittent left-sided epistaxis. His symptoms failed to improve after a prolonged antibiotic and decongestant course.
He appeared healthy on examination and had hyponasal speech. Nasal endoscopy revealed bilateral profuse mucus that required suctioning. A large nasal mass was seen emanating from the right middle meatus with a smooth mucosal surface and prominent blood vessels. He had a slight right cheek swelling visible externally.
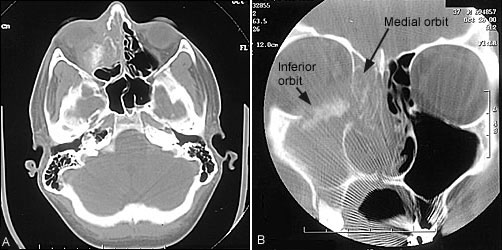
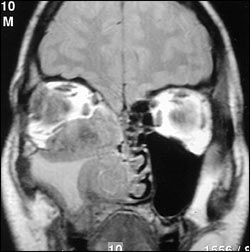
CT scan showed a large neoplasm of the right paranasal sinuses with bony erosion of inferior and medial orbit (Figure 3). For better definition of the neoplasm, an MRI scan was obtained. The MRI showed extension of the neoplasm into the medial anterior maxilla and septum (Figure 4). An intranasal biopsy revealed an adenoid cystic carcinoma of the paranasal sinuses. He underwent transfacial and endoscopic resection of the mass with postoperative radiation therapy.
Final Comment
Our understanding and management of paranasal sinus infections have improved since the introduction of nasal endoscopy, CT scans, and MRI. Uncomplicated cases of sinusitis are most often treated empirically based on findings from the history and physical examination. Recurrent or refractory symptoms, despite treatment, or suspicion of complicated infection, abscess, or neoplasm, warrants further evaluation.