
Am Fam Physician. 2003;67(6):1233-1240
Molluscum contagiosum and warts are benign epidermal eruptions resulting from viral infections of the skin. Molluscum contagiosum eruptions are usually self-limited and without sequelae, although they can be more extensive in immunocompromised persons. Spontaneous disappearance of lesions is the norm, but treatment by local destruction (curettage, cryotherapy, or trichloroacetic acid) or immunologic modulation can shorten the disease course, possibly reducing autoinoculation and transmission. Warts result from a hyperkeratotic reaction to human papillomavirus infection; nongenital warts are classified as common, periungual, flat, filiform, or plantar, based on location and shape. Warts are treated by local destruction (acids, cryotherapy, electrodesiccation-curettage), chemotherapy, or immunotherapy. The choice of treatment varies with the age and wishes of the patient, the potential side effects of the treatment, and the location of the lesions.
Molluscum contagiosum (MC) and warts are benign epidermal eruptions that result from viral infections of the skin. They are frequently encountered in the primary care setting. Armed with clinical experience and a few tools and medicines, family physicians will be able to treat most cases.
Molluscum Contagiosum
Papular eruptions that result from infection with the MC virus are usually self-limited and without sequelae in immunocompetent persons, although the lesions can last for months or even years.
MC infection occurs frequently among children and also affects sexually active adults, where it is classified among the sexually transmitted diseases.1 MC has gained additional attention over the past two decades because of its prevalence as an opportunistic infection in persons with human immunodeficiency virus (HIV) infection. In patients with HIV, MC infection often is not self-limited and can be much more extensive and even disfiguring. Recent studies have suggested that MC may serve as a cutaneous marker of severe immunodeficiency and sometimes is the first indication of HIV infection.2
MC is a double-stranded DNA virus in the Poxviridae family. As with other poxviruses, MC is spread through fomite or skin-to-skin contact, and microscopic abrasions in the epidermis are thought to facilitate transmission.3
DIAGNOSIS
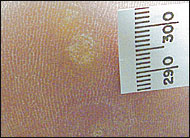
The typical MC lesion is an asymptomatic, firm, smooth, round papule with central umbilication (Figure 1). Lesions are usually 3 to 5 mm in diameter and number less than 30,4 although these parameters often are exceeded in persons with HIV and other immunocompromised conditions.5,6 In children, the papules typically are found on the extremities, trunk, and face (Figure 2). In sexually transmitted cases, they usually occur on the lower abdomen and in the genital region.
TREATMENT
Spontaneous disappearance of MC lesions with no residual scarring is common, often after a period of inflammation and minor tenderness.7 Few controlled studies of treatment efficacy have been performed, but many experts recommend local destruction to prevent autoinoculation (spread by scratching) and transmission to others.
Lesion eradication may be mechanical (curettage, laser, or cryotherapy with liquid nitrogen or nitrous oxide cryogun), chemical (trichloroacetic acid, tretinoin [Retin-A]), or immunologic (imiquimod [Aldara]).
Curettage or cryotherapy is commonly performed in the primary care setting. In children, application of topical anesthetic (e.g., lidocaine/prilocaine [EMLA cream]) under occlusion 15 to 30 minutes before curettage has been shown to significantly reduce pain.8
Anecdotal reports and small studies suggest that imiquimod, an immune enhancer that induces cytokines, may be useful in treating MC, especially when numerous lesions are present or destructive methods are not tolerated.9 [Evidence level C, consensus/expert guidelines] This treatment seems to be migrating into clinical practice. Advantages to imiquimod therapy include minimal side effects and ease of application.
Early studies using varying potencies and application regimens have shown clearance rates of 40 to 82 percent.9 Imiquimod is available as a 5-percent cream and is approved for treating genital and nongenital warts. It is applied three times per week, left on the skin for six to 10 hours, then washed off. A typical course of treatment lasts from four to 16 weeks.
MC in patients with HIV infection and other immunocompromising conditions can be more severe, making treatment more difficult. Researchers have had some initial success with the nucleotide analog cidofovir in HIV-infected patients with advanced MC. Topical and intravenous forms have been tested,10 and controlled trials of cidofovir are likely to be forthcoming.
Warts
Like MC, warts result from infection with a double-stranded DNA virus trophic to human skin. In the case of warts, the agent responsible is human papillomavirus (HPV), of which there are more than 150 serotypes.11 Some are known to cause cervical cancer, but common warts that affect nongenital skin are not thought to have malignant potential. With the exception of cervical lesions, determining the serotype of a wart is not clinically useful. Some physicians use the serotype of cervical lesions to determine how aggressively they evaluate and treat the patient.
The most useful information is gleaned from clinical appearance and the area of the body that is affected. Trained clinicians usually can diagnose warts based solely on their typical appearances in different locations.12 Non-genital warts are subcategorized into common, periungual, flat, filiform, and plantar types.
DIAGNOSIS
Common Warts
Common warts (verrucae vulgaris) are irregularly surfaced, domed lesions that can occur almost anywhere on the body (Figure 3). Multiple warts are common and are spread by skin-to-skin contact or contact with a contaminated surface. After initial infection, warts frequently are spread by autoinoculation from scratching, shaving, or other skin trauma.
On exposed skin, these warts tend to be hard and, if not affected by mechanical forces, develop the typical carpet-like (verrucous) surface (Figure 4). On areas that receive frequent friction, such as the hands, the firm, nodular aspect predominates (Figure 5). On areas that are moist or occluded, warts tend to be softer and more polypoid.
Periungual Warts
Periungual warts occur at the nail margins (Figure 6). As with other warts on the hands and feet, they often show peeling and roughening of the surface and tend to be somewhat abraded although not as much as palmar warts. They can affect the shape of the nail by undermining its side and pushing the nail up or causing partial detachment, sometimes mimicking the changes that occur with onychomycosis (Figure 7). Occasionally, when the wart affects the nail matrix or when destruction of the wart injures the nail matrix, permanent nail deformity can result.
Flat Warts
Filiform Warts
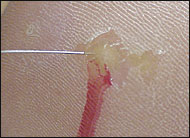
Filiform warts have frond-like projections that often rapidly grow. They are common on the face (Figure 9).

Plantar Warts
Plantar warts occur on the plantar surface of the foot (Figure 10). Because of the forces exerted on the foot, plantar warts tend to become callused and grow into the foot instead of rising above the plantar surface. They often occur in multiples, are firm, and can be very painful. Patients may feel as if they are walking with a pebble in their shoe. Plantar warts can be differentiated from a corn or callus by paring down the surface (Figure 11). A wart has the typical punctate pattern of multiple pinpoint blood vessels (Figure 12). Warts also do not retain the normal fingerprint lines of the hands and feet, as calluses and corns do.



TREATMENT
Treatment options for warts include mechanical destruction and adjustment of the patient's immune system through medications, and observation. The most commonly employed treatments involve destroying the affected tissue by freezing, burning, curetting (usually with electrodesiccation), or applying topical acids. Chemotherapeutics are sometimes used in refractory or severe cases (Table 1). A review of the placebo arms of 17 treatment trials showed an average spontaneous regression rate of 30 percent at an average of 10 weeks.14 Six trials using salicylic acid averaged a 75 percent cure rate, and two trials comparing cryotherapy and salicylic acid found no difference in success rates.14
| Acids |
| Over-the-counter salicylic acids (e.g., Compound W, DuoFilm liquid or patches) |
| Bi- or trichloroacetic acid |
| Freezing |
| Liquid nitrogen freeze via spray gun or cotton-tipped applicator at −196 C (−320.8 F)16 |
| Cryogun with nitrous oxide tank freeze at −89 C (−128.2 F)16 |
| Aerosol spray with adapter freeze (e.g., Verruca-Freeze) at −70 C (−94 F)16 |
| Burning |
| Electrocautery, LEEP, laser |
| Chemotherapy |
| Bleomycin (Blenoxane) |
All treatments are hampered by wart persistence and recurrence. Warts are only an outward symptom of an underlying infection; topical treatments do not eradicate HPV but merely hold it at bay.15 [Evidence level C, consensus/expert guidelines]
Acids
Many patients treat warts themselves with over-the-counter salicylic acid preparations. Advantages of these acids include convenience, reasonable cost, minimal discomfort, and reasonable effectiveness. Disadvantages include the length of time before results are seen (usually weeks to months) and complex instructions. Patients have to soak the wart in water for five to 10 minutes before each application (daily for liquids, every 48 hours for patches), then debride the dead skin after each application.
Bi- and trichloroacetic acids are applied in the physician's office on a weekly basis, usually after paring down the wart. Although this usually is a painless and effective procedure, these more potent acids have a greater potential to significantly burn surrounding skin.
Acids are well suited for use in children (as long as they don't put the affected area in their mouths) and are appropriate for plantar warts and warts on sensitive body parts where cryotherapy would be more painful.
Freezing
The different methods of freezing warts are presented in Table 1. One advantage of a nitrous oxide cryogun versus a liquid nitrogen gun is its ability to adhere the probe to the skin and elevate the lesion to avoid damage to underlying structures, such as veins, nerves, or tendons (Figure 14). Liquid nitrogen at −196°C (−320.8°F) and nitrous oxide at −89°C (−128.2°F) exceed the temperature required for complete tissue destruction (−50°C [−58°F]), but liquid nitrogen produces a faster freeze.16 A reasonable option for the low-volume practitioner is Verruca-Freeze, a liquid applied from a spray can, at −70°C (−94°F).

The wart is frozen until it and 1 to 2 mm of surrounding skin have turned white (Figure 15). A repeat freeze after thawing causes more effective tissue destruction than a single freeze. The affected tissue turns red or blisters over the next one to two days, then gradually sloughs off over the following weeks. The dead tissue also may generate an immune system reaction to help resolve additional warts. Freezing is time-efficient and works well for most warts. In plantar warts, the discomfort and blistering after freezing can temporarily limit mobility.

Burning
Burning and surgical removal are usually reserved for resistant warts. Appropriate anesthetic measures are necessary because of the associated pain. Treatment can be accomplished in a single visit and is effective, but as with all destructive methods, not guaranteed. A disadvantage is prolonged recovery time from an often large and deep skin defect. Full-thickness excision and suturing are not warranted and can produce additional scarring and complications. Filiform warts are easily shaved or snipped off with an iris scissors (Figure 16). Light electrocautery of the base provides hemostasis and destruction of the residual wart.

Chemotherapy
Chemotherapy with bleomycin (Blenoxane) injection causes acute tissue necrosis. As with cryotherapy, the tissue left behind may stimulate an immune response. Disadvantages are the pain of injection and the expense of the drug. Bleomycin is a sterile powder that is reconstituted with saline. It is stable for only 24 hours after mixing, so it cannot be saved for dosing multiple patients on different days. Chemotherapy may be useful at a designated wart clinic, where several patients can be treated from the same vial of bleomycin in a single day. It is commonly used for plantar warts.
Immunotherapy
HPV infection does not disappear once the gross lesions are destroyed. Cell-mediated immunity is required to keep the infection in check, as demonstrated by the high prevalence of warts among immunosuppressed organ-transplant recipients and patients with acquired immunodeficiency syndrome.17,18 Several treatment methods for warts are directed toward enhancing the immune response that suppresses HPV infection (Table 2).
| Injected agents |
| Candida antigen |
| Mumps antigen |
| Interferon alfa-2b (Intron A) and interferon alfa-N3 (Alferon N)* |
| Topical agents |
| Imiquimod (Aldara) |
| Systemic agents |
| Cimetidine (Tagamet) |
Most people have been exposed to Candida and will mount an immune response. Candida antigen (0.1 mL of 1:1,000 solution, as is used for dermal testing) is mixed with 0.9 mL of 1-percent lidocaine (Xylocaine) and injected into the base of the wart (Figure 17). The wart is then stabbed repeatedly with the needle. Although uncomfortable, this procedure induces an immune response and brings about resolution of the wart in many cases.
In a small study19 using mumps or Candida injection, 74 percent of participants had resolution of the injected wart and, of those with resolution, 78 percent also had resolution of all of their noninjected warts. Candida antigen is available in a multi-dose vial that can be saved with refrigeration, so the cost is not prohibitive. Candida antigen can be used on most verrucae, particularly plantar warts.
Cimetidine (Tagamet) is known to stimulate T-lymphocyte populations, which are important in controlling viral infections. At a dosage of 30 to 40 mg per kg per day, it has been tried with varying success in the treatment of warts. A small trial20 in children found cimetidine to be as effective as the usual topical agents or cryotherapy. Another trial21 combining cimetidine with levamisole (an immunomodulator used in the treatment of colon cancer) reported cure rates of 85.7 percent versus 45.5 percent with cimetidine alone. However, in a more recent double-blind study,22 cimetidine was not found to be significantly more effective than placebo in adults or children, although there was a trend toward efficacy in younger patients. Cimetidine or watchful waiting could be considered for use in children who cannot tolerate destructive treatment methods.
The immunomodulating agents interferon alfa-2b (Intron A), interferon alfa-N3 (Alferon N), and imiquimod are approved for genital HPV. In addition to case reports, one study23 of 50 patients showed a 56 percent clearance rate with imiquimod. Imiquimod is more rapidly being adopted into clinical practice because of its easy application. It may be useful in non-genital HPV, but more study is needed.9
Topical application of sensitizing agents such as diphenylcyclopropenone, dinitrochlorobenzene, and squaric acid causes an allergic contact reaction that has been used for treatment of warts, but these chemicals are not commonly stocked by family physicians.