
Am Fam Physician. 2003;67(7):1481-1488
Sports have become increasingly popular and account for numerous eye injuries each year. The sports that most commonly cause eye injuries, in order of decreasing frequency, are basketball, water sports, baseball, and racquet sports. Sports are classified as low risk, high risk, and very high risk. Sports-related eye injuries are blunt, penetrating, and radiation injuries. The use of eye protection has helped to reduce the number and severity of eye injuries. The American Society for Testing and Materials has established performance standards for selected eyewear. Consultation with an eye care professional is recommended for fitting protective eyewear. The functionally one-eyed, or monocular, athlete should take extra precautions. A preparticipation eye examination is helpful in identifying persons who may be at increased risk for eye injury. Sports-related eye injuries should be evaluated on site with an adequate examination of the eye and adnexa. Minor eye injuries may be treated on site. The team physician must know which injuries require immediate referral to an ophthalmologist and the guidelines for returning an athlete to competition.
Sports and recreational activities are becoming increasingly popular and account for more than 40,000 eye injuries each year in the United States. About 90 percent of sports-related ocular injuries are considered preventable.1–5 Athletes should be educated by team physicians about proper eye and facial protection and encouraged to use protective devices.
Thirty percent of ocular injuries among children younger than 16 years are sports related. Basketball, water sports, baseball, and racquet sports account for most injuries.1 Among young persons five to 14 years of age, baseball is most frequently associated with ocular injury, while among persons 15 to 64 years of age, basketball is the leading cause of eye injuries.1,2,6–10
Sport Classification and Risk
The American Medical Association classifies sports as collision (football, rugby, hockey, lacrosse), contact (baseball, soccer, basketball, wrestling), noncontact (cross-country running, track, tennis, crew, swimming), and other (bowling, golf, archery, field events). These classifications may be misleading because golf and racquet sports, for instance, have a great potential for eye injury but may not be considered hazardous for the monocular athlete if these classifications are followed. Conversely, these classifications may be overly restrictive with regard to contact sports such as hockey, for which adequate eye protection is available.7
When considering the potential for eye injury, it may be more appropriate to categorize sports as low risk, high risk, and very high risk. Low risk indicates no use of a ball, puck, bat, stick, or racquet, and no body contact. Examples include track/field, swimming, gymnastics, and cycling. High-risk sports involve the use of a ball, puck, bat, stick, or racquet, and/or body contact. Examples of high-risk sports include baseball, hockey, football, basketball, lacrosse, racquet sports, tennis, fencing, golf, and water polo. Very-high-risk sports, such as boxing, wrestling, and contact martial arts, are those in which eye protectors typically are not worn.2,10
Preparticipation Examination
A complete eye examination should be part of any sports physical. With each athlete, physicians should obtain an ocular history, paying special attention to prior conditions such as a high degree of myopia, surgical aphakia, retinal detachment, eye surgery, and injury or infection. Athletes with any of these conditions may be at increased risk for serious eye injury.2,11,12 It also is important to assess athletes who have a strong family history of retinal detachment, retinal tears, and diabetic retinopathy.12 Athletes with such risk factors should be evaluated by an eye care professional before engaging in any high-risk or very-high-risk sport.13
Most Common Mechanisms of Eye Injuries
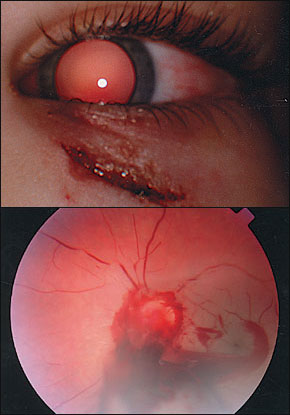
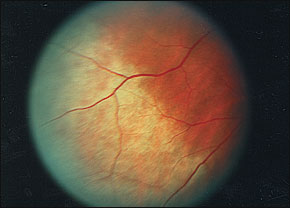
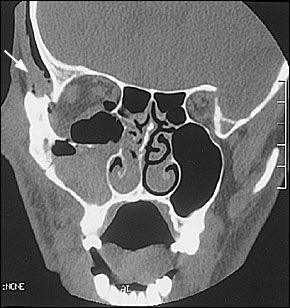
The most common mechanisms of eye trauma involve blunt, penetrating, and radiation injuries. Blunt trauma accounts for most sports-related eye injuries.5,14 The extent of ocular damage depends on the size, hardness, and velocity of the blunt object, and the force imparted directly to the eye. A direct blow to the globe from a blunt object smaller than the eye's orbital opening causes rapid anteroposterior compression and dilation of the middle of the globe, transmitting a great force to the internal ocular structures. A blunt object larger than the orbital opening exerts force on the floor of the orbit or the medial wall, resulting in fractures of the thin bones. This “pressure-release valve” may prevent rupture of the globe. However, there is a high incidence of occult internal ocular injuries1,7 (Figure 1).
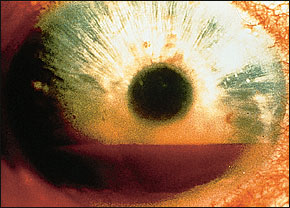
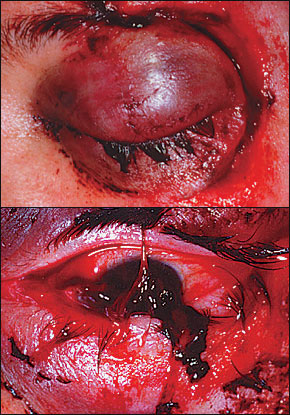
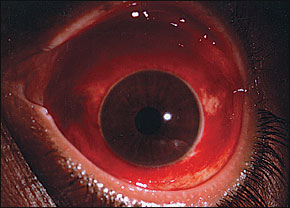
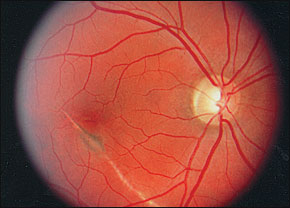
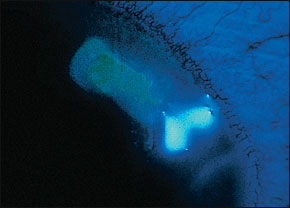
Examples of blunt injuries include orbital blowout fracture, orbital and lid contusions, iris injury, ruptured globe (Figure 2), traumatic iritis, subconjunctival hemorrhage (Figure 3), hyphema—blood in the anterior chamber—(Figure 4), retinal hemorrhage, commotio retinae (Figure 5), vitreous hemorrhage, choroidal rupture (Figure 6), retinal tears, and retinal detachment.3,7,8,12,15–18
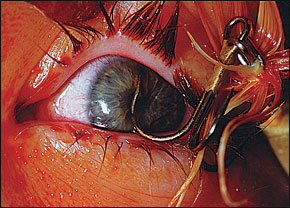
Penetrating injuries are relatively uncommon but may occur even with large projectiles. Eyeglass breakage also can cause penetrating injury.1 Such injuries range from mild abrasions to serious lacerations. Canalicular lacerations usually occur because of trauma from a fellow player's finger in the area of the medial canthus.8 Fishing hooks have been known to cause penetrating globe injuries (Figure 7). Radiation injuries occur as a result of exposure to ultraviolet light in snow skiing, water skiing, and other water sports.5,14
Aspects of the Ocular Examination
Sports-related ocular injuries can be evaluated on site with the appropriate medical supplies (Table 1).1 First, an adequate history should be obtained to determine the force and direction of the impact. For example, the physician should find out whether the injury was from a line drive, a fly ball, a pitched ball, or a hockey “slap shot.”10 Best-corrected visual acuity is checked using an eye chart. Confrontation visual fields should be checked. Visual field defects suggest a retinal, optic nerve, or central nervous system injury.
Next, the pupils should be examined with a bright light source. The physician should check for anisocoria (unequal pupil size) and for a relative afferent pupillary defect. Normally, the pupils constrict promptly and equally during accommodation and exposure to direct light and to light directed at the other pupil (i.e., consensual light reflex). If light reflex is diminished in one eye, a swinging flashlight test may discriminate between an afferent (retina or optic nerve) lesion and an efferent (third nerve or pupillary muscle) lesion. A deafferented pupil constricts consensually, but not to direct light, paradoxically enlarging when the light is quickly brought from the unaffected side (Marcus Gunn pupil). An efferent lesion prevents direct and consensual constriction while the unaffected eye maintains both. Pupil irregularity is almost always pathologic. A penlight examination of the anterior chamber should be performed to check for foreign bodies, hyphema, abrasions (Figure 8), and lacerations.
Both eyes should have full motility in all positions of gaze. Elevation of gaze may be limited by an orbital floor fracture. Double vision in any gaze position suggests significant injury in one or both eyes.1
External examination is then performed. Signs of orbital injury include periorbital ecchymosis, edema, proptosis, and bony step-offs of the orbital rim. Trismus, or pain when opening the mouth, often occurs with fractures of the lateral wall of the orbit. Paresthesia in the V2 (infraorbital) distribution of the trigeminal nerve suggests a fracture of the orbital floor (Figure 9).
| Sudden decrease in or loss of vision |
| Loss of field of vision |
| Pain on movement of the eye |
| Photophobia |
| Diplopia |
| Proptosis of the eye |
| Light flashes or floaters |
| Irregularly shaped pupil |
| Foreign-body sensation/embedded foreign body |
| Red and inflamed eye |
| Hyphema (blood in anterior chamber) |
| Halos around lights (corneal edema) |
| Laceration of the lid margin or near medial canthus |
| Subconjunctival hemorrhage |
| Broken contact lens or shattered eyeglasses |
| Suspected globe perforation |
Finally, funduscopic examination is done to evaluate the red reflex. Even modest bleeding into the ocular media can alter or obscure the red reflex. This may be the only sign of occult rupture of the globe. Any alteration of the red reflex requires immediate ophthalmologic referral.13,19 Signs and symptoms that warrant immediate referral are outlined in Table 2.1,3,10,19
| Injury | Diagnosis/treatment | Comments |
|---|---|---|
| Corneal abrasion | Apply topical anesthetic, then apply fluorescein strips to conjunctival sac; abraded epithelium is identified by fluorescent green stain with use of cobalt blue light. | Pain and blepharospasm may make it difficult to open eyes. Athlete may not return to play. |
| Apply antibiotic ointment to affected eye; 24-hour ophthalmologic follow-up is mandatory. | ||
| Superficial corneal foreign body | Apply topical anesthetic; remove foreign body with sterile irrigating solution or moistened sterile cotton swab; never use needle. Apply antibiotic ointment; 24-hour follow-up is mandatory. | Refer if foreign body cannot be removed. |
| Athlete may not return to play. | ||
| Concealed foreign object | Usually beneath upper eyelid or in lower fornix; hidden foreign object suggested by vertical linear corneal abrasions that appear after fluorescein strip staining. Evert upper eyelid; remove foreign body with sterile irrigating solution or moistened swab. If corneal abrasion is present, follow guidelines for treating corneal abrasions. | If no corneal abrasion is present, athlete may resume play. Patching is not recommended. |
| Superficial eyelid laceration | Rule out globe injury. Full-thickness lacerations, especially involving lid margin, warrant immediate referral. Use sterile skin closures if only skin is involved. Reapproximate superficial lacerations not involving lid margins. | Never forcibly open a lid swollen shut by edema or hematoma (could express eye contents through unsuspected laceration). |
| Athlete may not resume play; refer. | ||
| Athlete may resume play. | ||
| Lacerations medial to pupil involve canalicular system until proved otherwise. | ||
| Athlete may not resume play; refer. | ||
| Blunt trauma | Look for facial fractures and globe injuries. Relative afferent pupillary defect also suggests traumatic optic neuropathy. Immediately refer patient with orbital fractures. | |
| Acute pain, proptosis, resistance to retropulsion, and relative afferent pupillary defect suggest retrobulbar hemorrhage, which requires emergent lateral canthotomy. Refer for high-dose IV steroids. | ||
| If no signs of orbital fracture or optic neuropathy are present, use rest, analgesics, and cold compresses to control further edema and discomfort. | ||
| Hyphema | Blood present in anterior chamber? May result in increased intraocular pressure. Restrict play, shield the eye, and refer immediately. | Rebleeding within five days carries worse prognosis than the primary bleed. |
| Burns | Classic signs of UV burn are intense pain, photophobia, and delay in symptom onset. Fine punctate staining with fluorescein is characteristic. Treat with systemic analgesics and topical antibiotic. Refer if epithelial defect is present. | Occurs in water/snow sports; snow blindness results from prolonged exposure to UV-B rays reflected from snow. |
| Prognosis is usually excellent after treatment. |
When eye trauma occurs, the possibility of a globe rupture must be considered. Perforation and rupture are indicated by darkly pigmented uveal tissue presenting through a laceration.1,19 A tear-drop–shaped pupil may indicate iris prolapse through a wound at the limbus. Subtle signs of globe rupture include subconjunctival hemorrhage, a deep or shallow anterior chamber, or a conjunctival laceration. If globe rupture is suspected, no further manipulation of the eye should take place. After a protective shield is placed over the eye, the patient should be given nothing by mouth and should be referred immediately for ophthalmic evaluation. Table 31,3,10,13,19 outlines treatment of selected eye injuries.
| 2-mm polycarbonate lenses in normal streetwear frames (for athletes who need corrective lenses and are involved in low-risk sports). |
| Sports frames with a 3-mm polycarbonate lens (for athletes participating in moderate- to high-risk sports). Eye protection should be used by athletes who wear contact lenses and by those who do not need corrective lenses. The athlete with refractive errors should wear prescription polycarbonate lenses. |
| A sturdy sports frame meeting impact-resistance standards (i.e., ASTM F803-01) is required. Eyeguards without lenses do not pass ASTM racquet sports eye safety standards. |
| Face masks attached to a helmet should be used in sports such as hockey, football, baseball, and lacrosse.2,3 |
Protective Devices
Eye protection has reduced the number and severity of eye injuries. A protective device should dissipate a potentially harmful force over a larger area. Eye protectors need to shift impact from the eyes and face to the skull without causing intracranial injury. It may be necessary to integrate helmets with eye and face protectors. The American Society for Testing and Materials (ASTM) has established performance standards for selected eyewear in racquet sports, baseball, basketball, women's lacrosse, field hockey, and alpine skiing. ASTM F803–01 standards establish performance requirements for eye-wear that are most appropriate in sports with a risk of ocular injury.9 According to these performance standards, force transfer devices must be acceptable to the athlete, not change the appeal of the game, and not generate unacceptable liability.1,11,13
Protective eyewear often is made of polycarbonate, a highly impact-resistant plastic capable of absorbing ultraviolet light. Because this plastic is eight times stronger than other materials, it is preferred for use in protective glasses. Polycarbonate lenses are available in prescription and nonprescription lenses. Contact lenses offer no eye protection, and eyeglasses provide inadequate protection. Regular eyeglasses have only 4 to 5 percent of the impact resistance of polycarbonate of comparable thickness.1–3,11,20 Guidelines for protective eyewear are listed in Table 4.2,3
Functionally One-Eyed Athletes
An athlete is considered monocular when the best corrected visual acuity in the weaker eye is less than 20/40. Such athletes must wear sports eye protectors that meet ASTM racquet sports standards in all sports that carry risks of eye injury, for all games and practices. An eye protector must be worn beneath a face mask in sports that require facial protection (i.e., hockey, football, and lacrosse). The athlete should be instructed to wear protective lenses at all times in case of non–sports-related trauma.2,3,7,11,20,21
Monocular athletes should wear polycarbonate lenses and frames while playing basketball. In hockey, a helmet with a full-face cage, made of either wire or polycarbonate, and sports goggles are needed. While playing football, the monocular athlete should wear a helmet with a face mask, a polycarbonate shield, and sports goggles. Monocular baseball players should wear sports goggles at all times. While batting or running bases, the appropriate helmet with a polycarbonate face guard and sports goggles should be worn. Boxing, wrestling, and full-contact martial arts are contraindicated in monocular athletes because no adequate eye protection is available.2,11,21 The functionally monocular athlete should be evaluated by an ophthalmologist before being admitted to participation in a particular sport.13
Return to Play
Several guidelines for returning to play after an injury should be followed. In patients with significant ocular injury, a full examination and clearance by an ophthalmologist are required. The injured eye should feel comfortable and have adequate return of vision. Eye protectors must be worn. During the game, immediate return to play depends on the athlete's symptoms and the nature of the injury as determined by the team physician. Athletes should never be allowed to use topical anesthetics to prolong play.10