
Am Fam Physician. 2003;67(12):2557-2562
Splinter injuries are common, but larger and deeper splinters are often difficult and painful to remove at home. These splinters often present as a foreign body embedded in the superficial or subcutaneous soft tissues. Whenever possible, reactive objects like wood, thorns, spines, and vegetative material should be removed immediately, before inflammation or infection occurs. Superficial horizontal splinters are generally visible on inspection or easily palpated. A horizontal splinter is exposed completely by incising the skin over the length of the long axis of the splinter, and removed by lifting it out with forceps. A subungual splinter may be removed by cutting out a V-shaped piece of the nail. The point of the V is at the proximal tip of the splinter, which is grasped and removed, taking particular care not to push the splinter further into the nail bed. Removal of an elusive splinter can be challenging and may require the use of imaging modalities for better localization. Deeper splinters, especially those close to important structures such as nerves, tendons, blood vessels, or vital organs, should be referred for removal.
Splinters are common in children and adults, most often presenting as a foreign body embedded in the superficial or subcutaneous soft tissues of the extremities. Wood, glass, and metallic splinters are among the most common retained foreign bodies.1 Most superficial splinters may be removed by the patients themselves, leaving to physicians only the deeper and larger splinters, or retained splinters that have broken down during an attempt at removal.2 If not removed completely, splinters may cause complications such as inflammation, infection, toxic reactions, and granuloma formation. Failure to diagnose the foreign body has emerged as a common cause of malpractice actions against family physicians. Even after a foreign body has been found, the physician should ensure that nothing is left in the wound. The physician also must be cautious in telling the patient that the splinter is entirely removed. It may be preferable to tell the patient that all of the visible splinter has been removed, but there is always a chance that small pieces may be present that are undetectable at that time.
Evaluation
The most common error in the management of soft tissue foreign bodies is the failure to detect their presence.2,3 A patient's suspicion that a foreign body may be present must be taken seriously. It is important to obtain a careful history, inquiring about the nature and timing of the injury, the composition of the material most likely involved, and the presence of any foreign-body sensation in the wound if the splinter is not readily visible. It is also important to ask about, and document, the tetanus immunization status of the patient.
The timing of the injury is important in evaluating splinters. A fresh injury usually has an injury track leading to the splinter that facilitates its detection and removal. Older injuries may present as infection, inflammation, induration, or granuloma formation, sometimes with no apparent history of foreign-body exposure. The composition of the foreign body dictates the reaction of the tissues to the splinter. Some types of foreign material are more toxic and allergic than others (Table 1).3,4 Wood, thorns, spines, and other vegetative foreign bodies are considered highly inflammatory, whereas glass, metal, and plastic are relatively inert materials.5
| Type of material | Reaction severity | Reaction type |
|---|---|---|
| Glass (uncontaminated) | Mild | Encapsulation |
| Blackthorns | Severe | Inflammatory reaction from alkaloids |
| Wood | Severe | Infection, inflammatory reaction from oils and resins |
| Cactus spines | Moderate to severe | Inflammation from fungal coating on the plant; delayed hypersensitivity reaction |
| Rose thorns | Moderate to severe | Inflammation from fungal coating on the plant |
| Sea urchins | Moderate to severe | Inflammation and infection; toxic and allergic reaction |
| Metal | Mild | Encapsulation |
| Plant spines (alkaloids) | Mild to severe | Toxic reaction |
| Animal spines | Mild to severe | Toxic reaction |
| Plastic | Mild | Encapsulation |
On physical examination, most superficial splinters can be visualized or palpated easily. Deeper splinters may be difficult to detect; at times, the only clue to the presence of retained foreign bodies may be swelling, tenderness, a mass, a draining sinus, or a soft tissue infection such as cellulitis, abscess, lymphangitis, bursitis, synovitis, arthritis, or osteomyelitis. While evaluating the patient with skin or soft tissue complaints, the physician should actively look for signs of a hidden foreign body (Table 2).3,4
An array of diagnostic tools is available for detecting and locating splinters (Table 3).3,4,6–11 The cost of an imaging modality and its likelihood of detecting the foreign body should be considered before it is ordered. Standard radiographs are the most practical means of screening for a radiopaque foreign body.3 Almost all glass is radiodense, and glass foreign bodies as small as 0.5 to 2 mm can be detected easily on plain radiographs.
| Puncture wound |
| Blood-stained injury track of a fresh wound |
| Sharp pain with deep palpation over a puncture wound |
| Discoloration beneath the epidermis |
| Wound that elicits pain with movement |
| Wound that fails to heal |
| Abscess (with sterile culture) |
| Pain associated with a mass |
| Mass under the epidermis |
| Chronically draining purulent wound |
| Cyst |
| Granuloma formation |
| Sterile monoarticular arthritis |
| Periosteal reactions |
| Osteomyelitis |
| Pseudotumors of bone |
| Delayed tendon or nerve injury |
On the other hand, wooden splinters are usually difficult to detect on plain radiographs unless there is paint on the wood that contains lead or other radiopaque substances.6 In most cases, two radiographic views may be adequate, but an oblique view may be more revealing and is readily obtainable. Computed tomographic (CT) scanning and magnetic resonance imaging (MRI) detect many foreign bodies that may be missed on radiographs and are particularly helpful in detecting wooden splinters lodged near bones.7 Although wooden splinters may be visible at an early stage on a CT scan, they soon become isodense with the adjacent tissue as the wood absorbs water. Sonography provides an excellent alternative method for identifying and localizing radiolucent foreign bodies.8–13 A 7.5-MHz probe is used to search for small, superficial objects, whereas a 5.0-MHz probe is recommended for larger, deeper objects.
Splinter Removal
When possible, reactive objects should be removed before inflammation or infection occurs. Wood, thorns, spines, and other vegetative foreign bodies should be eliminated immediately, but glass, metal, and plastic can be removed in a less restricted time frame.13 Small elusive splinters may be located more easily once they have become encapsulated by granulomatous or scar tissue.14
Proper preparation and setup include adequate lighting, anesthesia, magnification, and a bloodless, sterile field.4 The physician must resist the temptation to remove the splinter by simply pulling it out of the wound because this may leave small fragments behind.
| Material | Plain radiographs | High-resolution ultrasound scans | Xeroradiographs | CT scans | MRI |
|---|---|---|---|---|---|
| Wood | Poor | Good | Superior to plain radiograph | Good | Good |
| Metal | Good | Good | Good | Good | Poor |
| Glass | Good | Good | Good | Good | Good |
| Organic (thorns, spines) | Poor | Good | Superior to plain radiograph | Good | Good |
| Plastic | Moderate | Superior to plain radiograph | Good | Good | |
| Palm thorn | Poor | Moderate | Poor | Good | Good |
SUPERFICIAL HORIZONTAL SPLINTERS
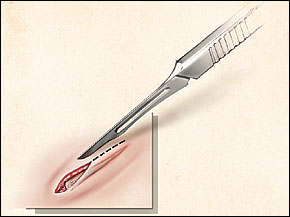
Superficial horizontal splinters are generally visible on inspection or easily palpated. The skin overlying the splinter is cleaned with povidone-iodine solution (Betadine) and infiltrated with 1 to 2 percent lidocaine with epinephrine (Xylocaine with epinephrine). Using a no. 15 scalpel blade, the skin is incised over the length of the long axis of the splinter, completely exposing it. The splinter is then easily lifted out with the blade or a forceps, and the track is cleaned with normal saline or povidone-iodine solution (Figure 1).
Anesthesia may be spared for removal of a small, superficial splinter. The splinter may be removed by picking it out with an 18-gauge needle, using light feathering strokes to de-roof the skin over the splinter.2 Once the sliver is reached, it can be lifted out with the needle tip or with the aid of small forceps. A firm pinching pressure applied to the local area reduces the amount of pain the patient may feel and controls the bleeding.15
VERTICAL SPLINTERS
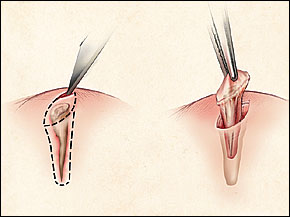
Splinters or foreign bodies such as needles that are at a right angle to the skin surface are usually more painful and difficult to remove. After injection of local anesthesia and a povidone-iodine cleansing, a superficial incision is made over the splinter, followed by deeper incisions around the splinter, undermining both sides of the wound. This maneuver facilitates displacement of the splinter to the middle of the wound, where it is then excised with a deep elliptic incision around the wound entrance (Figure 2).
DEEPER, ELUSIVE SPLINTERS
The search for a deeper, elusive splinter may be difficult. Before searching for an elusive foreign body, the physician should set a time limit for the search, usually 20 to 30 minutes.16 After this time, further effort only increases the chance of tissue damage, and the likelihood of locating the foreign body is minimal. Blind dissection with a curved hemostat is not recommended. Instead, an imaging technique should be used to help localize a deeper splinter.
Radiolucent splinters are not visualized on plain radiographs, and CT scanning, MRI, or ultrasonography should be strongly considered. Markers such as needles help in the precise localization of the splinter and facilitate its removal. Once localized, the foreign body is removed with a forceps or a hemostat, avoiding any unnecessary tissue dissection. Deeper splinters, especially those close to important structures such as nerves, tendons, blood vessels, or vital organs, should be referred for surgical removal.
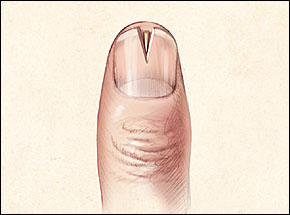
SUBUNGUAL SPLINTERS
The traumatic introduction of wood splinters under the fingernails and toenails is common and frequently associated with severe throbbing pain.17 Most of the splinters are lodged in the distal portion of the nail and their removal does not result in nail dystrophy. However, for a more proximal subungual splinter, caution must be exercised not to disturb the nail matrix because this may result in failure of the nail to grow back normally.
To remove such a splinter, the digit is anesthetized by means of a digital nerve block, and the nail plate overlying the splinter is partially avulsed. This can be accomplished by a variety of methods. Most commonly, a V-shaped piece of nail is cut using small, but strong, scissors. The point of the V is at the proximal tip of the splinter.17 The V-shaped portion of the nail is removed using a nail elevator and a forceps. The splinter is grasped and removed, taking particular care not to push the splinter further into the nail bed (Figure 3).
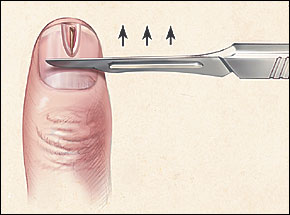
The nail plate also may be partially avulsed by shaving the nail plate overlying the splinter with a no. 15 blade. This is done by using light strokes with the blade held in a proximal-to-distal direction. This technique gradually creates a U-shaped defect in the nail, exposing the entire length of the splinter18 (Figure 4).
Alternatively, the distal portion of the nail plate may be vaporized with a carbon dioxide laser unit, if that option is available.17
Follow-Up Care
After removal of the splinter, the wound is copiously irrigated under high pressure, and the contaminated tissue is debrided.4 Sutures are avoided if possible, especially with contaminated wounds, where delayed primary closure is preferred. Routine wound-care instructions are given to the patient, and a 48-hour follow-up visit is scheduled as an office visit or a telephone call. After subungual splinter removal, postoperative wound care should include an occlusive dressing and a topical antibiotic.
The need for tetanus prophylaxis is addressed at the time of removal.2 Prophylactic antibiotics are generally not required but may be considered in some cases, depending on the type of splinter material and the appearance of the skin and subcutaneous tissues.