
Am Fam Physician. 2003;68(5):907-912
A more recent article on evaluation of knee pain in adults is available.
Family physicians frequently encounter patients with knee pain. Accurate diagnosis requires a knowledge of knee anatomy, common pain patterns in knee injuries, and features of frequently encountered causes of knee pain, as well as specific physical examination skills. The history should include characteristics of the patient's pain, mechanical symptoms (locking, popping, giving way), joint effusion (timing, amount, recurrence), and mechanism of injury. The physical examination should include careful inspection of the knee, palpation for point tenderness, assessment of joint effusion, range-of-motion testing, evaluation of ligaments for injury or laxity, and assessment of the menisci. Radiographs should be obtained in patients with isolated patellar tenderness or tenderness at the head of the fibula, inability to bear weight or flex the knee to 90 degrees, or age greater than 55 years.
Knee pain accounts for approximately one third of musculoskeletal problems seen in primary care settings. This complaint is most prevalent in physically active patients, with as many as 54 percent of athletes having some degree of knee pain each year.1 Knee pain can be a source of significant disability, restricting the ability to work or perform activities of daily living.
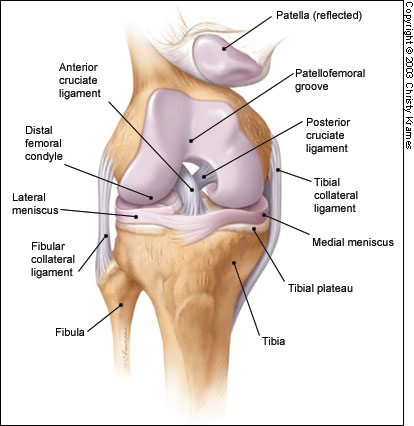
The knee is a complex structure (Figure 1),2 and its evaluation can present a challenge to the family physician. The differential diagnosis of knee pain is extensive but can be narrowed with a detailed history, a focused physical examination and, when indicated, the selective use of appropriate imaging and laboratory studies. Part I of this two-part article provides a systematic approach to evaluating the knee, and part II3 discusses the differential diagnosis of knee pain.
History
PAIN CHARACTERISTICS
The patient's description of knee pain is helpful in focusing the differential diagnosis.4 It is important to clarify the characteristics of the pain, including its onset (rapid or insidious), location (anterior, medial, lateral, or posterior knee), duration, severity, and quality (e.g., dull, sharp, achy). Aggravating and alleviating factors also need to be identified. If knee pain is caused by an acute injury, the physician needs to know whether the patient was able to continue activity or bear weight after the injury or was forced to cease activities immediately.
MECHANICAL SYMPTOMS
The patient should be asked about mechanical symptoms, such as locking, popping, or giving way of the knee. A history of locking episodes suggests a meniscal tear. A sensation of popping at the time of injury suggests ligamentous injury, probably complete rupture of a ligament (third-degree tear). Episodes of giving way are consistent with some degree of knee instability and may indicate patellar subluxation or ligamentous rupture.
EFFUSION
The timing and amount of joint effusion are important clues to the diagnosis. Rapid onset (within two hours) of a large, tense effusion suggests rupture of the anterior cruciate ligament or fracture of the tibial plateau with resultant hemarthrosis, whereas slower onset (24 to 36 hours) of a mild to moderate effusion is consistent with meniscal injury or ligamentous sprain. Recurrent knee effusion after activity is consistent with meniscal injury.
MECHANISM OF INJURY
The patient should be questioned about specific details of the injury. It is important to know if the patient sustained a direct blow to the knee, if the foot was planted at the time of injury, if the patient was decelerating or stopping suddenly, if the patient was landing from a jump, if there was a twisting component to the injury, and if hyperextension occurred.
A direct blow to the knee can cause serious injury. Anterior force applied to the proximal tibia with the knee in flexion (e.g., when the knee hits the dashboard in an automobile accident) can cause injury to the posterior cruciate ligament. The medial collateral ligament is most commonly injured as a result of direct lateral force to the knee (e.g., clipping in football); this force creates a valgus load on the knee joint and can result in rupture of the medial collateral ligament. Conversely, a medial blow that creates a varus load can injure the lateral collateral ligament.
Noncontact forces also are an important cause of knee injury. Quick stops and sharp cuts or turns create significant deceleration forces that can sprain or rupture the anterior cruciate ligament. Hyperextension can result in injury to the anterior cruciate ligament or posterior cruciate ligament. Sudden twisting or pivoting motions create shear forces that can injure the meniscus. A combination of forces can occur simultaneously, causing injury to multiple structures.
MEDICAL HISTORY
A history of knee injury or surgery is important. The patient should be asked about previous attempts to treat knee pain, including the use of medications, supporting devices, and physical therapy. The physician also should ask if the patient has a history of gout, pseudogout, rheumatoid arthritis, or other degenerative joint disease.
Physical Examination
INSPECTION AND PALPATION
The physician begins by comparing the painful knee with the asymptomatic knee and inspecting the injured knee for erythema, swelling, bruising, and discoloration. The musculature should be symmetric bilaterally. In particular, the vastus medialis obliquus of the quadriceps should be evaluated to determine if it appears normal or shows signs of atrophy.
The knee is then palpated and checked for pain, warmth, and effusion. Point tenderness should be sought, particularly at the patella, tibial tubercle, patellar tendon, quadriceps tendon, anterolateral and anteromedial joint line, medial joint line, and lateral joint line. Moving the patient's knee through a short arc of motion helps identify the joint lines. Range of motion should be assessed by extending and flexing the knee as far as possible (normal range of motion: extension, zero degrees; flexion, 135 degrees).5
PATELLOFEMORAL ASSESSMENT
An evaluation for effusion should be conducted with the patient supine and the injured knee in extension. The suprapatellar pouch should be milked to determine whether an effusion is present.
Patellofemoral tracking is assessed by observing the patella for smooth motion while the patient contracts the quadriceps muscle. The presence of crepitus should be noted during palpation of the patella.
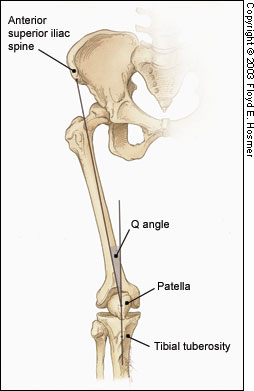
The quadriceps angle (Q angle) is determined by drawing one line from the anterior superior iliac spine through the center of the patella and a second line from the center of the patella through the tibial tuberosity (Figure 2).6 A Q angle greater than 15 degrees is a predisposing factor for patellar subluxation (i.e., if the Q angle is increased, forceful contraction of the quadriceps muscle can cause the patella to sublux laterally).
A patellar apprehension test is then performed. With fingers placed at the medial aspect of the patella, the physician attempts to sublux the patella laterally. If this maneuver reproduces the patient's pain or a giving-way sensation, patellar subluxation is the likely cause of the patient's symptoms.7 Both the superior and inferior patellar facets should be palpated, with the patella subluxed first medially and then laterally.
CRUCIATE LIGAMENTS
Anterior Cruciate Ligament
For the anterior drawer test, the patient assumes a supine position with the injured knee flexed to 90 degrees. The physician fixes the patient's foot in slight external rotation (by sitting on the foot) and then places thumbs at the tibial tubercle and fingers at the posterior calf. With the patient's hamstring muscles relaxed, the physician pulls anteriorly and assesses anterior displacement of the tibia (anterior drawer sign).
The Lachman test is another means of assessing the integrity of the anterior cruciate ligament (Figure 3).7 The test is performed with the patient in a supine position and the injured knee flexed to 30 degrees. The physician stabilizes the distal femur with one hand, grasps the proximal tibia in the other hand, and then attempts to sublux the tibia anteriorly. Lack of a clear end point indicates a positive Lachman test.
Posterior Cruciate Ligament
For the posterior drawer test, the patient assumes a supine position with knees flexed to 90 degrees. While standing at the side of the examination table, the physician looks for posterior displacement of the tibia (posterior sag sign).7,8 Next, the physician fixes the patient's foot in neutral rotation (by sitting on the foot), positions thumbs at the tibial tubercle, and places fingers at the posterior calf. The physician then pushes posteriorly and assesses for posterior displacement of the tibia.
COLLATERAL LIGAMENTS
Medial Collateral Ligament
The valgus stress test is performed with the patient's leg slightly abducted. The physician places one hand at the lateral aspect of the knee joint and the other hand at the medial aspect of the distal tibia. Next, valgus stress is applied to the knee at both zero degrees (full extension) and 30 degrees of flexion (Figure 4)7. With the knee at zero degrees (i.e., in full extension), the posterior cruciate ligament and the articulation of the femoral condyles with the tibial plateau should stabilize the knee; with the knee at 30 degrees of flexion, application of valgus stress assesses the laxity or integrity of the medial collateral ligament.
Lateral Collateral Ligament
To perform the varus stress test, the physician places one hand at the medial aspect of the patient's knee and the other hand at the lateral aspect of the distal fibula. Next, varus stress is applied to the knee, first at full extension (i.e., zero degrees), then with the knee flexed to 30 degrees (Figure 4).7 A firm end point indicates that the collateral ligament is intact, whereas a soft or absent end point indicates complete rupture (third-degree tear) of the ligament.
MENISCI
The physician grasps the patient's heel with one hand and the knee with the other hand. The physician's thumb is at the lateral joint line, and fingers are at the medial joint line. The physician then flexes the patient's knee maximally. To test the lateral meniscus, the tibia is rotated internally, and the knee is extended from maximal flexion to about 90 degrees; added compression to the lateral meniscus can be produced by applying valgus stress across the knee joint while the knee is being extended. To test the medial meniscus, the tibia is rotated externally, and the knee is extended from maximal flexion to about 90 degrees; added compression to the medial meniscus can be produced by placing varus stress across the knee joint while the knee is being extended. A positive test produces a thud or a click, or causes pain in a reproducible portion of the range of motion.
If radiographs are required, three views are usually sufficient: anteroposterior view, lateral view, and Merchant's view (for the patellofemoral joint).7,12 Teenage patients who report chronic knee pain and recurrent knee effusion require a notch or tunnel view (posteroanterior view with the knee flexed to 40 to 50 degrees). This view is necessary to detect radiolucencies of the femoral condyles (most commonly the medial femoral condyle), which indicate the presence of osteochondritis dissecans.13
Radiographs should be closely inspected for signs of fracture, particularly involving the patella, tibial plateau, tibial spines, proximal fibula, and femoral condyles. If osteoarthritis is suspected, standing weight-bearing radiographs should be obtained.
Laboratory Studies
The presence of warmth, exquisite tenderness, painful effusion, and marked pain with even slight range of motion of the knee joint is consistent with septic arthritis or acute inflammatory arthropathy. In addition to obtaining a complete blood count with differential and an erythrocyte sedimentation rate (ESR), arthrocentesis should be performed. The joint fluid should be sent to a laboratory for a cell count with differential, glucose and protein measurements, bacterial culture and sensitivity, and polarized light microscopy for crystals.
Because a tense, painful, swollen knee may present an unclear clinical picture, arthrocentesis may be required to differentiate simple effusion from hemarthrosis or occult osteochondral fracture.4 A simple joint effusion produces clear, straw-colored transudative fluid, as in a knee sprain or chronic meniscal injury. Hemarthrosis is caused by a tear of the anterior cruciate ligament, a fracture or, less commonly, an acute tear of the outer portion of the meniscus. An osteochondral fracture causes hemarthrosis, with fat globules noted in the aspirate.
Rheumatoid arthritis may involve the knee joint. Hence, serum ESR and rheumatoid factor testing are indicated in selected patients.