
Am Fam Physician. 2003;68(8):1527-1532
Lower extremity stress fractures are common injuries most often associated with participation in sports involving running, jumping, or repetitive stress. The initial diagnosis can be made by identifying localized bone pain that increases with weight bearing or repetitive use. Plain film radiographs are frequently unrevealing. Confirmation of a stress fracture is best made using triple phase nuclear medicine bone scan or magnetic resonance imaging. Prevention of stress fractures is most effectively accomplished by increasing the level of exercise slowly, adequately warming up and stretching before exercise, and using cushioned insoles and appropriate footwear. Treatment involves rest of the injured bone, followed by a gradual return to the sport once free of pain. Recent evidence supports the use of air splinting to reduce pain and decrease the time until return to full participation or intensity of exercise.
Stress fractures are among the most common sports injuries and are frequently managed by family physicians. A stress fracture should be suspected in any patient presenting with localized bone or periosteal pain, especially if he or she recently started an exercise program or increased the intensity of exercise. Other possible sources of bone pain, including metastatic lesions, should be considered.
Stress fractures can result from participation in many activities and sports, especially those requiring running and jumping. Athletics, or track and field sports, account for 50 percent of stress fractures in men and 64 percent in women.1 Participation in some sports that are not considered to be high-impact, such as platform diving and rowing (crew), also may cause stress fractures, particularly of the metatarsals and ribs. Hockey, golf, swimming, fencing, and softball have very low reported incidences of stress fractures.1
This article reviews common stress fractures of the lower extremity, especially those involving the tibia, fibula, and metatarsal bones. Stress fractures of the upper extremity may occur in sports involving repetitive use of the arms, such as baseball or tennis. Stress fractures of the ribs occur in sports such as rowing. Upper extremity and rib stress fractures are far less common than lower extremity stress fractures.1
Etiology and Pathophysiology
Stress fractures of the lower extremity most commonly involve the tibia and metatarsal bones.1,2 Stress fractures of the fibula, the navicula, the pelvis, and the femoral neck of the femur are less common.1 Although several factors appear to contribute to the development of stress fractures (Table 1),1–9 they generally occur as a result of a repetitive use injury that exceeds the intrinsic ability of the bone to repair itself.3,10
| Participation in sports involving running and jumping |
| Rapid increase in physical training program |
| Poor preparticipation physical condition |
| Female gender |
| Hormonal or menstrual disturbances |
| Low bone turnover rate |
| Decreased bone density |
| Decreased thickness of cortical bone |
| Nutritional deficiencies (including dieting) |
| Extremes of body size and composition |
| Running on irregular or angled surfaces |
| Inappropriate footwear |
| Inadequate muscle strength |
| Poor flexibility |
| “Type A” behavior |
Two competing, but not mutually exclusive, theories may explain the development of stress fractures. One theory holds that during the initial increase in exercise activity, the osteoblastic activity lags behind osteoclastic activity by a few weeks, resulting in a period during which bone is more susceptible to injury. Torsional and bending stress forces from repetitive use result in microfractures that consolidate into stress fractures.2,4,11 The other theory emphasizes strong and repetitive stress on bone at the insertion point of muscles, resulting in focal bending stresses beyond the ability of the bone to tolerate.3,4,10
Stress fractures often occur in nonathletes or deconditioned persons who begin a new exercise program, such as military recruits.2,3,4 Women are generally more likely to develop stress fractures than men. In women, nonathletes undertaking unusual activity are more likely to develop stress fractures than athletes, except for those athletes who exercise to the point of amenorrhea.1–3,5,12 In both men and women, stress fractures tend to recur. Approximately 60 percent of persons with a stress fracture have had a previous stress fracture.13
Tibial fractures are the most common lower extremity stress fracture,1,3 accounting for approximately one half of all stress fractures in children and adults.1,14 Stress fractures of the tibia are especially common in sports involving running and jumping.2,3 In children, tibial stress fractures usually occur in the anterior proximal one third of the bone, whereas in adults, the junction of the middle and distal one thirds seems to be the most prevalent site.14 Anterior stress fractures of the tibia usually result from tension stress and have a higher incidence of nonunion than anteromedial fractures.
Metatarsal fractures represent approximately 25 percent of stress fractures.1 These fractures most often involve the distal second and third metatarsals and are least common in the fifth metatarsal.3 Second and third metatarsal fractures are common in military recruits marching for the first time in combat boots (hence the term “march fracture”), and in ballet dancers involved in dancing on the tips of their toes (i.e., “en pointe”).3,15,16 Fifth metatarsal stress fractures are less common and must be distinguished from Jones fractures or avulsion fractures.15 Fifth metatarsal fractures are more common in patients with varum stresses of the foot or knee (genuvarum). The latter are more prone to nonunion.15
Navicular fractures are the most common stress fractures of tarsal bones, with calcaneus fractures accounting for almost all of the remainder.1 These fractures are often associated with jumping and sprinting sports such as athletics or basketball. The fracture is typically linear and located in the central one third of the bone.15 These fractures carry a risk of displacement if not diagnosed.15
Femoral stress fractures also are rare, representing only about 5 percent of all stress fractures.1 They are, however, extremely important because they are difficult to diagnose and have a high incidence of fracture nonunion, complete fractures, or avascular necrosis, which may result in an unrecoverable injury.3 Femoral stress fractures are more common in endurance athletes.1
Diagnosis
Stress fractures of the lower extremity present as localized dull pain not associated with trauma that worsens during exercise or weight bearing.2,17 Localized swelling or periosteal thickening may occur at the pain site. The differential diagnosis includes “shin splints” (periosteitis), compartment syndromes, and nerve or artery entrapment syndromes.2 Tenderness to palpation typically is present at the injury site and is the hallmark of a stress fracture.2,17 In femoral fractures, patients usually complain of pain in the groin, anterior thigh, or knee, as well as painful range of motion of the hip.3
Plain film radiographs generally should be obtained in the initial evaluation but may not reveal a stress fracture soon after the symptom onset (Figure 1).17 Evidence of a fracture may never appear on plain radiographs or may not appear for two to 10 weeks after symptom onset.3,17 Repeat radiographs obtained during the convalescent phase reveal the fracture in approximately 50 percent of cases. The appearance of what has been called “the dreaded black line” (a transverse fracture line across the entire anterior shaft of the tibia that most often occurs in dancers or athletes who participate in jumping sports) on a radiograph is considered a poor prognostic sign with increased likelihood of nonunion.2,3

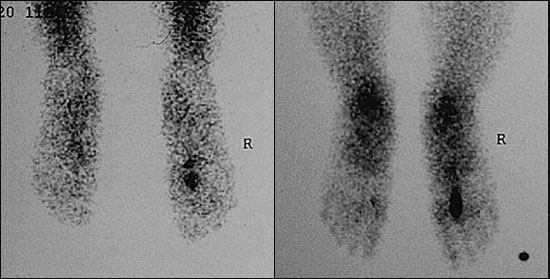
Triple phase nuclear bone scans are more sensitive than plain radiographs in the detection of stress fractures early in the clinical course.3,17 [Evidence level A, meta-analysis/randomized controlled trials (RCTs)] A focal “hot spot” is shown on the bone scan at the point of maximal tenderness (Figure 2). Longitudinal stress fractures, though more rare, tend to show diffuse uptake of the radioisotope along the bone, and therefore are more difficult to diagnose using bone scan.17–19 Magnetic resonance imaging scans are much better than plain films for initial diagnosis and may characterize the fracture better than bone scans.3,17–19 [Evidence level B, nonrandomized studies]
The use of low-frequency ultrasonography over the affected area for several minutes may precipitate a pain response in fractures, allowing rapid and inexpensive diagnosis. Two studies, however, failed to show a significant difference in the use of ultrasonography for the detection of stress fractures.20,21 Low-frequency ultrasonography is not recommended at this time for the routine diagnosis of stress fractures.20 [Evidence level A, meta-analysis/RCTs]
Treatment
Treatment recommendations are summarized in Table 2.3,4,11,14,22–24 Conservative therapy for stress fractures involves the use of ice, nonsteroidal anti-inflammatory drugs, and rest of the affected bone for several weeks or until pain-free.3,4 Additionally, pre-exercise warm-up and stretching, and a gradual return to the offending exercise intensity are indicated.3,10 Substitution of a non–weight-bearing exercise, such as swimming (or upper extremity bicycle for lower extremity fractures), may speed recovery without loss of cardiovascular conditioning.10
| All stress fractures (conservative therapy) |
| Modified rest for six to eight weeks (or until pain-free for two to three weeks); activities of daily living and limited walking are permitted |
| Nonsteroidal anti-inflammatory drugs |
| Cryotherapy |
| Stretching and flexibility exercises |
| Cross-training (non–weight-bearing exercise) |
| Tibial stress fractures |
| Aircast splinting if more severe symptoms or if not resolved with conservative treatment |
| Casting for mid-shaft fractures until pain-free and radiographic evidence of healing |
| Surgery (intramedullary nailing and/or grafting) if no improvement after six months of treatment (or for certain elite athletes) |
| Metatarsal stress fractures |
| Wood-soled shoe or casting for four to six weeks |
| Special attention should be given to fifth metatarsal fractures to prevent nonunion |
| Fibula stress fractures |
| Usually heal in four to six weeks with conservative therapy and rarely require surgery |
| Navicular stress fractures |
| Six weeks of short leg non–weight-bearing cast, followed by four to six weeks of transitional weight-bearing cast |
| Gradual return to full weight bearing with a semirigid shoe |
| Intramedullary nailing if nonunion or delayed union |
| Return to sport in 16 to 20 weeks |
| Femoral stress fractures |
| Conservative therapy for compression fractures (return to sport in eight to 14 weeks) |
| Internal fixation for tension-type fractures |
Promising, but not well-controlled, data indicate that air splinting or pneumatic casting can significantly reduce pain and healing time in tibial and fibular stress fractures.11,17,22,23 A Cochrane Review indicated a likely benefit to the use of such air casting for more rapid return to sports participation.24 [Evidence level A, meta-analysis/RCT] One small noncontrolled study recommended the use of low-intensity ultrasonography for pain relief in tibial fractures.25
For nonunion of stress fractures, such as those involving the “dreaded black line,” surgery and intramedullary nailing may be necessary, with prolonged healing for months to years expected.2 [Evidence level B, nonrandomized studies]
Prevention
A gradual increase in the intensity of exercise, not to exceed an increase of 10 percent per week, generally is recommended for prevention of all stress fractures.6,14 Adequate stretching with warm-up before exercise is advised.4 Stretching is especially important in the prevention of tibial stress fractures.4 The use of lightweight footwear in good condition and smooth, level running surfaces are specifically recommended to prevent lower extremity stress fractures4,26 as well as correcting predisposing biomechanical conditions by using custom orthotics or arch supports.
A Cochrane Review involving four trials suggested that the use of shock-absorbing insoles may prevent stress fractures and stress reactions of the lower extremities.24 [Evidence level A, meta-analysis/RCTs] Another study found that decreased exercise intensity after an initial intense period may be effective in preventing stress fractures but may not be significant when corrected for cluster randomization.24 [Evidence level A, meta-analysis/RCTs]