
Am Fam Physician. 2003;68(10):2025-2026
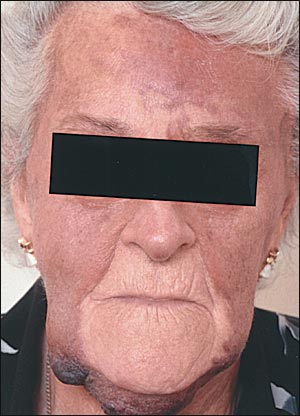
An 85-year-old woman was referred for a two-year history of progressive reddish plaques involving the face and scalp with dependent edema and ecchymoses (see accompanying figure). She said her condition began as a purplish patch on the forehead that gradually increased in size, eventually covering most of her face and scalp. Perioral sparing was noted. Previously, her condition had been diagnosed as benign hemorrhagic dermatitis. The lesions were tender and bled intermittently. She had no history of any hematologic disorder or trauma to the face. Her medications included omeprazole and thyroxine.
Question
Discussion
The answer is B: angiosarcoma. Angiosarcomas are rare neoplasms that make up less than 1 percent of all sarcomas.1 It is uncertain whether they arise from vascular or lymphatic endothelia. Approximately 50 percent occur in the head and neck, usually in elderly persons. Men are affected more frequently than women.2 Angiosarcomas of the scalp behave in a highly malignant manner.3 The diagnosis is often delayed and may be confused with traumatic bruising or allergic reactions. The usual presentation of angiosarcoma is a small erythematous or violaceous macule, sometimes accompanied by facial edema. Other neoplasms that can appear similar to angiosarcoma include Kaposi's sarcoma and hemangiopericytoma.
Treatment of angiosarcoma is not well established. Wide excision is preferable but is usually difficult to achieve with facial lesions. Radiation and chemotherapy, alone or in combination, also are used. The overall prognosis is poor, with five-year survival rates of 32 percent for tumors less than 5 cm, and 13 percent for lesions measuring greater than 5 cm.4 Local recurrence and metastases are common, often occurring in the first few years. Metastases occur most often in the lungs, followed by the lymph nodes, soft tissue, bone, and liver.5
Angiosarcoma may be confused with Kaposi's sarcoma because of similar histologies, but the typical clinical presentation is different. Kaposi's sarcoma most commonly affects patients with acquired immunodeficiency syndrome. Occasionally, it also is seen in immunocompetent patients, usually elderly men of Jewish or Mediterranean descent. Kaposi's sarcoma usually has a slowly progressive course but occasionally disseminates.
Drug reactions can lead to localized cutaneous eruptions but would resolve after withdrawal of the causative medication. Omeprazole and thyroxine are not associated with such eruptions.
Benign ecchymoses would not persist for two years. The patient also has no history of trauma to the head.
Dermatomyositis is well known to cause a heliotrope rash of the face, which is a violaceous discoloration around the eyes. It is not associated with such widespread discoloration or hemorrhagic lesions.