
Am Fam Physician. 2004;69(5):1046-1049
to the editor: A healthy 20-year-old United States Navy search and rescue swimmer trainee, who was equipped with only a mask and fins, developed hemoptysis, sharp substernal chest pain, and shortness of breath after performing a dive to a depth of 12 feet. He immediately surfaced and began to cough up pink, frothy sputum and have persistent shortness of breath. His initial oxygen saturation was 70 percent on room air and improved to 86 percent on three liters of oxygen via nasal cannula during ambulance transfer. On arrival at the emergency department, the patient had an oxygen saturation of 100 percent on three liters of oxygen with improved shortness of breath and resolved hemoptysis.
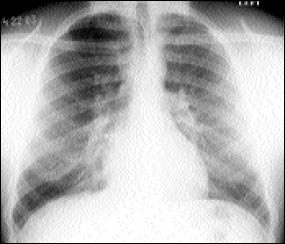
Auscultation of the lungs revealed bilateral rhonchi. The remainder of the physical examination was unremarkable with all vital signs being normal. Electrocardiogram, complete blood count, electrolytes, creatine kinase, troponin, and coagulation studies were all within normal limits. A chest radiograph showed fluffy perihilar infiltrates bilaterally (see the accompanying figure). A chest radiograph taken several hours later showed resolving infiltrates. The patient was diagnosed with swimming-induced pulmonary edema (SIPE) and discharged.
While the exact pathophysiology of SIPE remains uncertain, it is believed to be related to exertion, immersion in cold water, and overhydration. The body's normal response to exercise is to increase cardiac output to meet the increased oxygen demand. Although an increased cardiac output is known to cause pulmonary edema in racehorses, this increase is rarely enough to produce such an effect in humans.1 Cold-water immersion is instrumental in this process because the peripheral vasculature constricts to divert blood away from the extremities in an effort to maintain the core body temperature. This results in a central pooling of blood, leading to an increased preload, increased pulmonary artery pressure, and an increased cardiac output. The vasoconstriction also causes an increase in afterload, which leads to an increase in pulmonary vasculature resistance. The increased cardiac output from exertional activities coupled with an increased preload and afterload from immersion appear to be sufficient to rupture the pulmonary capillary membranes, thus resulting in pulmonary edema. In several documented cases of SIPE, it has been noted that the patients consumed anywhere from two to four liters of water in the hours leading up to their swim in an effort to remain well hydrated.2 It is believed that this degree of hydration led to a fluid overload that contributed to the onset of pulmonary edema by increasing the pulmonary capillary pressure.2 Patients may present with symptoms, such as cough, dyspnea, hemoptysis, tachypnea, and confusion with hypoxia, after exertional cold water activity such as swimming and scuba diving.3
Treatment for patients with SIPE consists primarily of supportive measures such as removing the patient from the wet and/or cold environment and providing supplemental oxygen. Although useful in treating pulmonary edema in racehorses, diuretics are typically not necessary because patients tend to show relief of symptoms soon after being placed on supplemental oxygen.4 Full resolution of radiographic findings typically occurs within 24 to 48 hours.