
Am Fam Physician. 2004;69(8):1941-1948
Diagnosis of upper extremity injuries depends on knowledge of basic anatomy and biomechanics of the hand and wrist. The wrist is composed of two rows of carpal bones. Flexor and extensor tendons cross the wrist to allow function of the hand and digits. The ulnar, median, and radial nerves provide innervation of the hand and wrist. A systematic primary and secondary examination of the hand and wrist includes assessment of active and passive range of motion of the wrist and digits, and dynamic stability testing. The most commonly fractured bone of the wrist is the scaphoid, and the most common ligamentous instability involves the scaphoid and lunate.
Whether a physician is working in a rural clinic or an urban academic center, or is attending a high school football game, acute injuries of the hand and wrist will be encountered. Patients may not appreciate the severity of these injuries and are as likely to present in a clinic as in the emergency department. Timely diagnosis and treatment of upper extremity injuries are of paramount importance. Failure to diagnose, manage, and rehabilitate upper extremity injuries has the potential to result in permanent disability.1
Part one of this two-part article reviews an anatomic-based examination of the hand and wrist, allowing the physician to quickly evaluate a patient in a nonemergent setting. Part two2 focuses on the emergent evaluation of hand and wrist injuries.
Anatomy
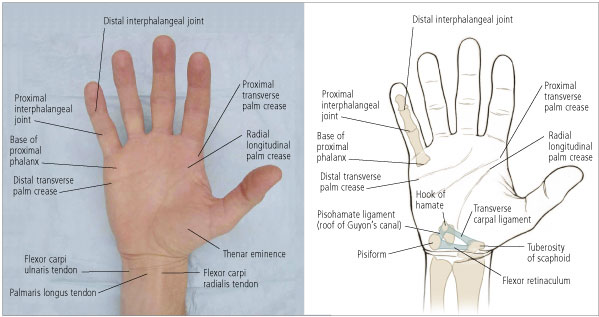
Many injuries of the hand and wrist are obvious, but subtle injuries can be missed without a systematic primary and secondary examination. There are eight carpal bones in the wrist, five metacarpals, and 14 nonsesamoid bones that comprise the phalanges. These 27 bones act dynamically to allow oppositional grip.3 The proximal row of carpal bones includes the scaphoid (i.e., carpal navicular bone), lunate, triquetrum, and pisiform, which are closely approximated to the distal radius (Figure 1). The triangular fibrocartilage complex, an articular disk located between the proximal row of carpals and the ulna, completes the concave surface on which the carpals move (Figure 2). The distal row of carpals includes the hamate, capitate, trapezium, and trapezoid, which are closely approximated to the metacarpals. The scaphoid links the two rows of carpals.
Each digit has two neurovascular bundles near the palmar aspect of the finger—one located radially and the other ulnarly. The neurovascular bundle includes the digital artery, vein, and nerve.4
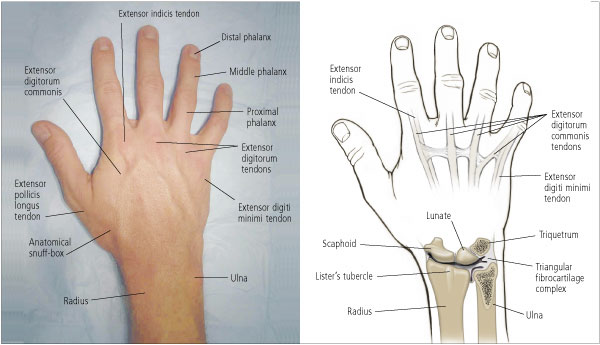
Twelve extensor tendons of the wrist are arranged in six compartments along the dorsum of the wrist. There are multiple slips of the abductor pollicis longus and two slips of the extensor digiti quinti. The extensors originate in the lateral and dorsal forearm, inserting on the dorsal aspect of the hand. Twelve flexor tendons of the wrist originate in the medial part of the forearm and insert on the palmar aspect of the hand and wrist.5
Each phalanx has a superficial flexor tendon that inserts at the base of the middle phalanx and a profundus flexor tendon that inserts at the base of the distal phalanx. Consequently, injuries of the flexor tendons are more complicated to evaluate and repair than injuries of the extensor tendons.
In general, the radial nerve accounts for wrist and finger extension, the ulnar nerve provides power grip, the median nerve allows for fine control of the pincer grip, and the median and ulnar nerves supply sensation to the palmar surface. However, to truly place the hand in a functioning position, the entire upper extremity must be involved. The ulnar nerve enters the hand alongside the ulnar artery through Guyon's canal, located between the pisiform and the hook of the hamate and covered by the pisohamate ligament (Figure 4). The ulnar nerve supplies the intrinsic muscles of the hand as well as the extrinsic muscles for flexion of the fourth and fifth fingers to provide power grip. The ulnar nerve also innervates the adductor pollicis and first dorsal interosseous muscles, which allow pinch. The median nerve passes into the hand via the carpal tunnel of the volar aspect of the wrist. The median nerve supplies the thenar compartment, providing opposition and circumduction for fine control. The radial nerve extends the fingers to enhance grasp with the ulnar nerve.
Examination
| Examination technique | Abnormal result | Possible pathology |
|---|---|---|
| While the patient's hand is in the resting position look for fingers that are flexed or extended | Flexed finger | Disrupted extensor tendon (see Figure 6 right) |
| Extended finger | Disrupted flexor tendon (see Figure 6 left) | |
| While patient flexes fingers toward the palm, check that tips of fingers point toward the scaphoid (see Figure 7) | Fingers extend normally but overlap when flexed | Fracture with rotational deformity of finger |
| Check for changes in skin color or ability to sweat | Part or all of finger has a different skin color (blanched or hyperemic) or lacks ability to sweat | Digital nerve injury |
| Check capillary refill after applying pressure to distal fingertip or nail bed | Blanching lasts more than two seconds | Microvascular compromise |
| Check two-point discrimination in distal fingertip using blunt calipers or a paper clip | Patient cannot distinguish two points at least 5 mm apart | Neurologic compromise |
PRIMARY EXAMINATION
The primary survey includes evaluation of passive and active range of motion of the fingers and wrist while noting the resting position of the hand. Manipulation is not always necessary; much can be noted about the hand and fingers with simple observation.
| Examination technique | Abnormal result | Possible pathology |
|---|---|---|
| The patient flexes the proximal IP joint of the affected finger while the other fingers are kept extended. | Patient cannot flex joint | Disrupted flexor digitorum superficialis |
| The patient extends the distal IP joint of the affected finger while the other fingers are kept extended. | Patient cannot flex joint | Disrupted flexor digitorum profundus (i.e., jersey finger) |
| The patient extends the distal IP joint of the affected finger. | Patient cannot extend joint or lacks complete joint extension | Fracture of distal phalanx or rupture of extensor tendon (i.e., mallet finger) |
| The patient shakes hands with the examiner, then attempts to pronate and supinate the wrist while the examiner resists movement. | Patient has pain or cannot complete the movement | Pathology of distal ulnar joint or triangular fibrocartilage complex (in the absence of radiographic findings) |
| Locate the small, bony prominence on the ulnar aspect of the palm in the area of the palmar crease. | Tenderness | Trauma to pisiform |
| After pisiform is located, the physician's thumb IP joint is placed on the pisiform, and the thumb is directed toward the patient's index finger. When the patient flexes the wrist, the hook of the hamate can be felt with the tip of the thumb. | Tenderness | Fracture of hook of the hamate |
| Follow the extensor carpi radialis tendon distally where it intersects the palmar crease, then palpate the small protuberance. | Tenderness | Fracture of scaphoid tubercle |
| Locate the extensor pollicis longus and abductor pollicis longus, then palpate the depression between them (the anatomical snuff-box). | Tenderness | Fracture of distal pole |
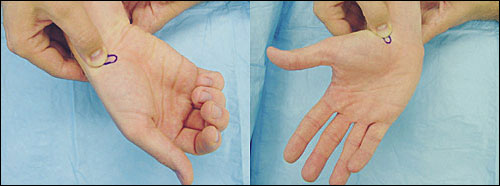
| Physician's thumb is placed on scaphoid tubercle while thewrist is held in ulnar deviation, then the patient actively radially deviates the wrist while the physician exerts pressure on the tubercle (see Figure 8) | Pain | Fractured scaphoid |
| Pain with clunk | Scapholunate instability | |
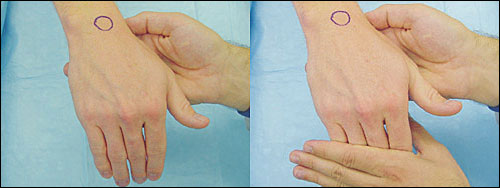
| Patient's wrist is held in flexion while the physician resists active finger extension (see Figure 9) | Pain | Parascaphoid inflammation, radiocarpal instability, midcarpal instability |
A patient's inability to assume the “safe hand” position (Figure 5) may suggest a tendon or nerve disruption.7 If the hand is immobilized in the safe hand position, extension contractures of the metacarpophalangeal (MCP) joint and flexion contractures of the IP joints can be avoided. In normal anatomic position, the thumb is slightly abducted, the MCP joint is at 45 to 70 degrees, and each of the IP joints is slightly flexed at 10 degrees. Physicians should be alerted to the possibility of tendon disruption if any of the fingers are not maintained in the position8 (Figure 6). As the hand is closed, fingers should point toward the base of the scaphoid (Figure 7). The distal nail tips should align when the fingers are partially flexed.
Subtle skin changes can alert the physician to possible nerve injury. The hand normally has moisture on it; absence of moisture on the distal phalanx may indicate a digital nerve injury. The vascular status of the finger is evaluated by blanching the fingertip; capillaries should refill within two seconds. Sensory nerve function of the digits can be evaluated with two-point discrimination using a paper clip or blunt calipers. The patient should be able to distinguish two points about 5 mm apart.3

SECONDARY EXAMINATION
The secondary survey should include tests of the superficialis and profundus flexor tendon of each finger.1 With practice, each of the flexor tendons of the fingers can be evaluated. Each digit should flex independently. The patient should be able to actively flex the distal IP joint, indicating an intact profundus flexor tendon. The superficialis tendon is evaluated by having the patient flex the proximal joint of the finger while the remaining fingers are extended. If there is any question of tendon disruption, a simple test can be performed. In this test, the physician grasps the patient's forearm approximately 6 to 7 cm from the proximal palmar crease of the wrist and squeezes the forearm.9 As the forearm is grasped, each of the flexor tendons can be identified by passive flexion of the patient's corresponding digit. Range of motion of the wrist, as well as any deformity or swelling, should be noted. Full forced pronation and supination of the hand without pain virtually eliminates pathology of the distal radioulnar joint or triangular fibro-cartilage complex from consideration.10

Palpation of the hand usually starts on the ulnar side. The pisiform can be palpated easily in the hypothenar eminence just distal to the distal wrist crease on the palmar ulnar aspect of the hand. To locate the hook of the hamate, the physician places his or her thumb's IP joint on the patient's pisiform and directs the distal aspect of his or her thumb toward the patient's index finger. When the patient's wrist is flexed, the hook of the hamate can be felt with the tip of the physician's thumb. A fracture of the hook of the hamate usually is not apparent on typical radiographic images of the hand; a carpal tunnel view or computed tomographic scan sometimes is necessary.11

The flexor carpi ulnaris, the flexor carpi radialis, and the palmaris longus tendons usually can be observed by having the patient oppose the thumb and fifth finger while flexing the wrist. The flexor carpi ulnaris inserts on the pisiform. Because 12 to 15 percent of people lack a palmaris longus tendon, care must be taken not to confuse the flexor carpi radialis for the missing tendon. The flexor carpi radialis can be seen distally on the volar radial aspect of the wrist as it crosses the distal palmar crease. In this area, the proximal tubercle of the scaphoid is a prominence that can be palpated easily. If the thumb is placed on the scaphoid tubercle, four fingers can wrap around the distal radius while the wrist is held in ulnar deviation. As the patient radially deviates the wrist, the scaphoid tubercle will volarflex into the physician's thumb. If pressure is directed dorsally with the thumb, pain may be elicited. This reaction may indicate a fractured scaphoid, or a scapholunate instability if an associated “clunk” is noted. This maneuver is termed the Watson or Scaphoid Shift Test12 (Figure 8).
On the dorsum of the wrist, the anatomical snuff-box can be identified easily as the patient abducts and extends the thumb. The extensor pollicis longus tendon can be identified on the radial aspect of the wrist by having the patient raise the thumb with the palm pronated on a surface. The waist of the scaphoid is located just radial in a depression in the wrist. Pain in this area can be an indication of a scaphoid fracture.13 The patient's wrist is then held in flexion, and active finger extension with resistance is tested. Significant parascaphoid inflammation, radial carpal, or midcarpal instability will cause considerable pain with this maneuver, known as the Shuck Test1 (Figure 9).
The triscaphe joint is located by following the dorsal side of the second finger proximally; the physician's thumb will fall into a recess. The scapholunate joint can be palpated by following the third finger proximally until the thumb falls into a recess, just distal to Lister's tubercle dorsally. Lister's tubercle is a small, mast-like protuberance in the center of the distal radius that is identified by palpating the distal radius while the patient flexes the wrist. The lunate is the most prominent area on the dorsum of a flexed wrist. Kienböck's disease, a post-traumatic avascular necrosis of the lunate, is present in up to 20 percent of patients with lunate fractures.
Pathology
Understanding the surface anatomy of the hand and wrist allows the physician to evaluate common injuries and appreciate less common injuries that might be overlooked on examination.
The scaphoid is the most commonly fractured bone of the wrist. Most of these fractures are caused by falling on an outstretched hand. Depending on the patient's age, bone density, and reaction time, this type of fall can result in a fractured scaphoid, scapholunate dislocation, or distal radius fracture.14
Patients with pain over the anatomical snuff-box should be treated for a possible scaphoid fracture, and a radiograph in what is called the “stretch or navicular view” should be obtained. This type of fracture carries a high likelihood of nonunion. To prevent supination and pronation of the wrist, the patient should be put into a long arm cast, or a short arm thumb spica splint or cast and shoulder sling; a simple palmar splint or “sugar-tong” splint is inadequate.
Patients with negative radiographs should be put into a temporary thumb spica splint for two weeks. When they are reexamined, another radiograph should be taken. If the patient's wrist is not tender and the second A gap of more than 3 mm in the scapholunate joint in a symptomatic patient should alert the physician to consider scapholunate instability until proven otherwise. radiograph is negative, the patient can be instructed to return only if symptoms recur. If the wrist is still tender, further evaluation and a surgical consultation are warranted even if the second radiograph is negative.15
A fractured hook of the hamate is a less common injury of the wrist that often is not diagnosed because it is not apparent on standard radiographic views. This injury may occur when a patient falls while holding an object, and the object lands between the ground and the ulnar side of the palm. It also may be caused when a bat hits a ball or a golf club catches the ground, and the hypothenar eminence is struck. Standard radiographs and a “carpal tunnel” view should be obtained in patients with tenderness over the hook of the hamate, and the ulnar nerve should be tested. These patients can be put in an ulnar gutter splint or simple volar splint and referred to a surgeon, because treatment often requires removal of a bone chip.10
The most common ligamentous instability of the wrist occurs between the scaphoid and the lunate. Patients with injuries of these ligaments often have a high degree of pain even though initial radiographs may appear normal. A gap of more than 3 mm in the scapholunate joint is considered abnormal, and a comparison radiograph of the opposite wrist should be obtained. Physicians should suspect this type of injury if a patient has wrist effusion and pain that is seemingly out of proportion to the injury. Patients with this type of injury often will not tolerate a Watson test. These injuries require an immediate consultation but can be stabilized with a thumb spica splint.16