
Am Fam Physician. 2004;70(5):879-884
Scaphoid fracture is a common injury encountered in family medicine. To avoid missing this diagnosis, a high index of suspicion and a thorough history and physical examination are necessary, because early imaging often is unrevealing. Anatomic snuffbox tenderness is a highly sensitive test for scaphoid fracture, whereas scaphoid compression pain and tenderness of the scaphoid tubercle tend to be more specific. Initial radiographs in patients suspected of having a scaphoid fracture should include anteroposterior, lateral, oblique, and scaphoid wrist views. Magnetic resonance imaging or bone scintigraphy may be useful if the diagnosis remains unclear after an initial period of immobilization. Nondisplaced distal fractures generally heal well with a well-molded short arm cast. Although inclusion of the thumb is the standard of care, it may not be necessary. Nondisplaced proximal, medial, and displaced fractures warrant referral to an orthopedic subspecialist.
The scaphoid bone is the most commonly fractured carpal bone; this injury occurs most often in young men. Scaphoid fractures are rare in young children and the elderly because of the relative weakness of the distal radius compared with the scaphoid in these age groups.1 Scaphoid fractures are significant because a delay in diagnosis can lead to a variety of adverse outcomes that include nonunion, delayed union, decreased grip strength, decreased range of motion, and osteoarthritis of the radiocarpal joint.2 Timely diagnosis, appropriate immobilization, and referral when indicated can decrease the likelihood of adverse outcomes.
Anatomy and Biomechanics
The scaphoid is a biomechanically important, boat-shaped carpal bone (from the Greek “skaphos,” meaning “boat”) that articulates with the distal radius, trapezium, and capitate. During radial deviation and dorsiflexion of the wrist, the scaphoid encroaches on the radius, limiting this motion. If this motion is forceful (e.g., a fall on an outstretched arm), enough stress on the scaphoid occurs to fracture it (Figure 1).

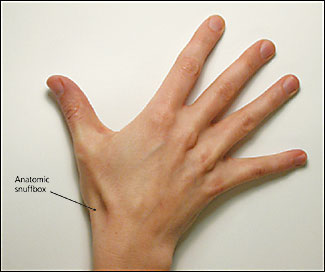
On surface anatomy, the scaphoid is located below the anatomic snuffbox (Figure 2). This triangular depression is defined by the extensor and abductors of the thumb, and is easily visible when the wrist is partially ulnar deviated and the thumb abducted and extended.
The blood supply of the scaphoid comes from the radial artery, feeding the bone on the dorsal surface near the tubercle and scaphoid waist. Because the proximal portion has no direct blood supply, nonunion caused by poor blood supply is an important complication of scaphoid fracture.
Clinical Presentation
The primary mechanism of injury is a fall on the outstretched hand with an extended, radially deviated wrist, which results in extreme dorsiflexion at the wrist and compression to the radial side of the hand. Forces are transmitted from the hand proximally to the arm through the scaphoid.1,3,4 The patient complains of a deep, dull pain in the radial wrist. The pain, which often is mild, is worsened by gripping or squeezing. There may be mild wrist swelling or bruising and, possibly, fullness in the anatomic snuffbox, suggesting a wrist effusion. Scaphoid fractures are most common in males 15 to 30 years of age4 and are rare in young children and infants.1
Physical Examination
When examining a patient with a suspected scaphoid injury, it is important to compare the injured wrist with the uninjured wrist. The classic hallmark of anatomic snuffbox tenderness on examination is a highly sensitive (90 percent) indication of scaphoid fracture, but it is nonspecific (specificity, 40 percent).5 For example, a false-positive result can occur when the radial nerve sensory branch, which passes through the snuffbox, is pressed and causes pain. Other physical examination maneuvers should be performed. Tenderness of the scaphoid tubercle (i.e., the physician extends the patient’s wrist with one hand and applies pressure to the tuberosity at the proximal wrist crease with the opposite hand) provides better diagnostic information; this maneuver has a similar sensitivity (87 percent) to that of anatomic snuffbox tenderness, but it is significantly more specific (57 percent).5 Absence of tenderness with these two maneuvers makes a scaphoid fracture highly unlikely.
Pain with the scaphoid compression test (i.e., axially/longitudinally compressing a patient’s thumb along the line of the first metacarpal) also was shown, in a retrospective analysis,6 to be helpful in identifying a scaphoid fracture, but in another study,7 this technique had a poor predictive value for identifying scaphoid fractures. Another maneuver that suggests fracture of the scaphoid is pain in the snuffbox with pronation of the wrist followed by ulnar deviation (52 percent positive predictive value, 100 percent negative predictive value).7
Differential Diagnosis
The differential diagnosis for suspected scaphoid injuries includes fractures of other metacarpal bones or the distal radius, scapholunate dissociation, arthritis, tenosynovitis, or strains (Table 1). These can be differentiated by the location of tenderness, pain with certain maneuvers, and radiographic abnormalities.
| Diagnosis | Physical and radiographic findings |
|---|---|
| Arthritis of the carpometacarpal or radiocarpal joint | Local tenderness, abnormal radiographs |
| De Quervain’s tenosynovitis | Lateral wrist pain, tenderness over radial styloid, positive Finkelstein’s test |
| Distal radius fracture | Local tenderness and deformity, abnormal plain radiographs |
| Extensor carpi radialis strain | Local tenderness, swelling, and pain elicited with wrist flexion |
| First metacarpal fracture | Local tenderness and deformity, abnormal plain radiographs |
| Flexor carpi radialis strain | Local tenderness, swelling, and pain elicited with wrist extension |
| Injuries to radioulnar joint | Local tenderness |
| Scapholunate dissociation | Tenderness over scapholunate ligament, increased gap between scaphoid and lunate on plain films |
| Scaphoid fracture | Anatomic snuffbox tenderness, pain with scaphoid compression test, tenderness of scaphoid tubercle |
Imaging
There are various imaging options for assessing a patient with a suspected scaphoid injury. They include plain radiographs, magnetic resonance imaging (MRI), ultrasonography, and bone scintigraphy. All of these modalities have advantages and disadvantages when evaluating patients for potential scaphoid fracture.
RADIOGRAPHY
Anteroposterior, lateral, and oblique radiographic views are required for evaluation of a suspected scaphoid fracture. Occasionally, a special radiograph called a scaphoid view may be helpful; the wrist is ulnarly deviated and extended while the film is shot from a dorsalvolar angle. When a fracture is visible, appropriate treatment may be instituted.
Initial radiographs do not always detect scaphoid fractures. In one prospective trial,8 the sensitivity of initial radiographs was 86 percent. However, a great deal of variability in the sensitivities (higher and lower) of radiographs is found in the literature. Nondisplaced fractures of this bone are known to be difficult to see on initial radiographs. In these cases, one treatment option includes placing the patient in a cast and performing a follow-up physical examination and repeat radiography in two weeks. Recent improvements in technology may allow alternate approaches in this situation.
MAGNETIC RESONANCE IMAGING
Although MRI is not indicated in the initial evaluation of patients with suspected scaphoid fractures, it can be helpful if the initial plain film is negative. Results of one study9 showed that with the use of dedicated-extremity MRI, scaphoid fractures could be diagnosed earlier—without waiting the usual two weeks to repeat the plain films. In this study, interobserver reliability was high.
Other studies have shown that MRI might be better than scintigraphy because the former is more sensitive and specific.10 One clinical study11 did find that early MRI after negative plain radiographs of suspected scaphoid fractures changed management strategies 90 percent of the time. The cost for the early MRI approach appears to be equivocal, but there have been no controlled studies concerning outcomes.12 Because nondisplaced fractures heal well, a study would be needed to confirm if early MRI adds anything to the treatment of nondisplaced fractures.
ULTRASONOGRAPHY
Ultrasound examination with routine equipment is not appropriate in the initial evaluation of suspected scaphoid fractures. High–spatial-resolution ultrasonography has been shown to be reliable and accurate in identifying occult scaphoid fractures.13
BONE SCINTIGRAPHY
Historically, the bone scan has been used to look for occult fractures of the scaphoid and other bones. In a study comparing bone scan with MRI,10 the authors found the two methods to be equivalent. In this study, 59 patients with clinical suspicion of scaphoid fracture and negative radiographs at presentation had a bone scan and MRI. Both methods found all fractures, but the MRI found some significant ligamentous and carpal instabilities. A Cochrane review14 of the data found that bone scintigraphy was a cost-effective and accurate method for assessing occult scaphoid fractures compared with repeat plain radiography.
Treatment Options
As a basic rule, in a patient with a clinically suspected scaphoid fracture but negative initial radiographs (Figure 3), it is reasonable to apply a short arm thumb spica and reevaluate the patient in two weeks. If a cast is not applied, the fracture can worsen over the following months (Figure 4). MRI or bone scintigraphy may be used initially if the patient desires an alternative approach. At the two-week visit, the patient should be free of pain, and a follow-up radiograph should be obtained.


The fractured scaphoid exhibits certain behavior that inhibits healing. Fracture fragments are inherently unstable and prone to displacement, and require motionless contact to achieve union.15 As mentioned before, the blood supply of the scaphoid is tenuous. For therapeutic decision making, the scaphoid is divided into three anatomic sections: proximal, medial, and distal. Fractures are further subdivided into displaced and non-displaced types.
NONDISPLACED FRACTURES
Nondisplaced distal fractures heal well with strict immobilization in a well-molded short arm thumb spica. Controversy exists over whether to use a long arm or a short arm cast. One comparison16 found that nondisplaced fractures healed well regardless of the type of cast that was used. Current treatment for this type of fracture is a thumb spica, but some evidence suggests that the thumb could be omitted from the cast. A randomized prospective trial17 found that immobilization of the thumb did not improve outcomes for nondisplaced fractures. Screw fixation may speed recovery to pre-injury activities; referral for surgery may be indicated, depending on the needs of the patient.18 As the fracture line moves proximally, there is more risk of displacement and nonunion; therefore, it would be appropriate to refer these patients for orthopedic consultation. If conservative treatment is attempted, a long arm cast with thumb immobilization is appropriate.
DISPLACED FRACTURES
Fractures with even small amounts of displacement are prone to nonunion, and operative treatment is recommended.19 Splinting and referral are indicated.