
Am Fam Physician. 2004;70(7):1315-1320
In cases of facial trauma, nasal fractures account for approximately 40 percent of bone injuries. Treatment in the primary care setting begins with evaluating the injury, taking an accurate history of the situation in which the injury occurred, and ascertaining how the face and nose appeared and functioned before the injury occurred. Serious injuries should be treated, then nasal inspection and palpation may be performed to assess for airway patency, mucosal laceration, and septal deformity. A thorough examination of the nose and surrounding structures, including the orbits, mandible, and cervical spine, should be completed. Imaging studies are necessary for facial or mandibular fractures. Patients with septal hematomas, cerebrospinal fluid rhinorrhea, malocclusion, or extraocular movement defects should be referred to a subspecialist. Treatment in the primary care setting consists of evaluation, pain and infection management, minimal debridement and, when the physician is appropriately trained, closed reduction. If an immediate referral is not indicated, close follow-up, possibly with a subspecialist, should be arranged within three to five days after the injury.
Injuries to the nose are relatively common; in cases of facial trauma, nasal fractures account for approximately 40 percent of bone injuries.1 Fights and sports injuries account for most nasal fractures in adults, followed by falls and vehicle crashes. Play and sports account for most nasal fractures in children. Physical abuse should be considered in children and women, and should be appropriately ruled out.2
Nasal fractures may occur in isolation or in association with other facial injuries. Furthermore, many nasal fractures go undiagnosed and untreated because some patients do not seek medical care.3 Though seen occasionally in family practice, patients with nasal fractures are more likely to present to emergency departments or urgent care settings. Fractures that are more than two days old will have substantial edema and should be referred urgently for subspecialty evaluation.
Anatomy
The nose is easily exposed to trauma because it is the most prominent and anterior feature of the face. The nose is supported by cartilage anteriorly and inferiorly, and by bone posteriorly and superiorly (Figure 1). The paired nasal bones, the nasal process of the frontal bone, and the maxilla form a framework to support the cartilaginous skeleton. Although most of the nasal structures are cartilaginous, the nasal bones usually are fractured in an injury.
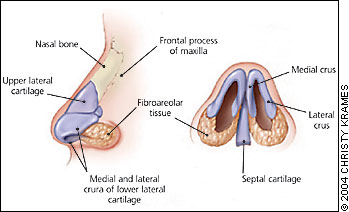
Overlying this framework are soft tissues, mucous glands, muscles, and nerves responsible for sensation and function of the nose. By virtue of its natural taper, the supporting nasal septum becomes increasingly thin and is therefore subject to fracture toward the tip of the nose.
The relative ease by which epistaxis can occur with minor trauma is explained by the dense and redundant vascular network that supplies the nose. This plexus, known as Kiesselbach’s area, is responsible for the vast majority of normal epistaxis.4 However, bleeding as a result of nasal fracture usually originates from other locations within the nose. For example, profuse anterior bleeding may originate from the anterior ethmoid artery (a branch of the ophthalmic artery), while posterior bleeding is more likely to arise from a branch of the sphenopalatine artery. Arterial ligation may be necessary if packing fails to control bleeding. In such cases, early consultation with an otolaryngologist is indicated.5,6
Assessment
HISTORY
Understanding the mechanism of trauma is helpful to the physician in determining the extent of the injury. It is useful to know the responsible object, the direction from which it came, and the strength of force sustained by the nose. For example, a direct frontal blow can depress the dorsum of the nose, causing the fractured bones to telescope posteriorly. Likewise, a laterally directed injury can cause a depression on the side of the impact, often with a corresponding outward displacement on the opposite side of the nose. Traction and torsion injuries, though rare, also can cause cartilaginous disruption.7
The patient should be asked about the timing and extent of any bleeding associated with the injury. The history also should include information regarding previous surgeries, injuries, and a subjective assessment of baseline nasal function and appearance. Finally, because alcohol use frequently is associated with such trauma, physicians may wish to determine whether the patient had been drinking before the injury. This point may have implications for selection of pain medications, potential for repeat injury, and the ability to assess for mental status changes associated with head injury.
PHYSICAL EXAMINATION
Most nasal fractures are the result of minor trauma such as being punched or elbowed. However, when assessing a patient with an acute nasal injury, the physician should avoid focusing solely on the obviously traumatized nose. This is particularly important if the patient has experienced a violent traumatic event such as a motor vehicle crash or an assault. A substantial direct blow to the mid-face area can result in cervical spine injury, and the physician must therefore exercise clinical judgment in using appropriate precautions until a cervical spine injury is ruled out. During the initial assessment, the physician should be certain that the patient has an adequate airway and is ventilating appropriately.
A nasal injury may be associated with other head and neck trauma that could compromise the patency of the trachea. Furthermore, given the close proximity of the nose to other facial structures, the physician must consider the possibility of an associated facial or mandibular fracture.3 Therefore, all bony structures of the face, including the malar eminences, orbital rims, zygomatic arches, mandible, and teeth, should be carefully inspected and palpated for irregularity or tenderness. All facial lacerations, swellings, and deformities should be noted, and the eyes should be examined for symmetry and mobility of gaze.8 If a facial or mandibular fracture is suspected, radiologic assessment with computed tomography (CT) is indicated.9
A deformity of the nose usually will be evident when a nasal fracture has occurred. However, epistaxis without obvious nasal deformity may be the only clinical finding in some nasal fractures. Edema and ecchymosis of the nose and periorbital structures ordinarily will be present, particularly if examination is performed more than several hours after the injury. Palpation of the nasal structures should be done to elicit any crepitus, indentation, or irregularity of the nasal bone. Uncommon findings such as a cerebrospinal fluid (CSF) leak posing as clear rhinorrhea, subcutaneous emphysema, mental status changes, new malocclusion, or limited extraocular movement should prompt immediate subspecialty referral.3,10
Knowledge of the shape and appearance of the patient’s nose before the injury will aid in comprehending the severity of the nasal injury. This is best accomplished by viewing a good quality photograph of the patient taken before the injury. If a photograph is not available, the photo on a driver’s license or identification card also may be used. Photographs of the injured nose also may be obtained for legal purposes and to measure treatment success.11
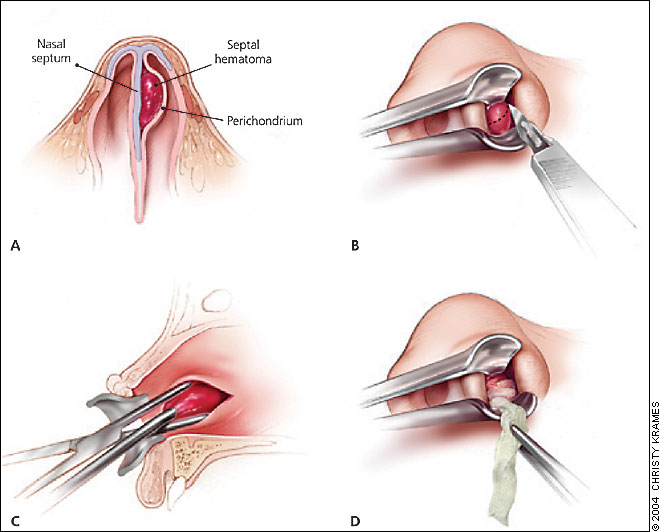
External and internal examination may be difficult following nasal injury because of ecchymoses, edema, and dried blood, especially if more than three hours have passed.6 If this is the case in a patient with an uncomplicated acute nasal fracture, it is appropriate to prescribe pain medication and release the patient with instructions to rest, apply ice, and maintain head elevation. Because no clinical evidence exists to mandate early fracture reduction,6,12 follow-up evaluation and management can be safely scheduled after the swelling resolves, usually within three to five days.7 Reduction should be accomplished between the fifth and 10th day after the injury, and before the nasal bones start to fixate.5 However, before releasing a patient with any type of nasal trauma, it is critical to rule out septal hematomas. These may appear as slightly white or purple areas of fluctuance lying on one or both sides of the nasal septum (Figure 2). Failure to identify and treat a septal hematoma can result in a saddle deformity of the septum, which will require surgical repair.

A thorough internal examination is facilitated with good lighting, suction, anesthesia, and vasoconstrictive nasal sprays. A nasal speculum and a headlamp will improve visualization, as will a fiberoptic endoscope, if available. The initial internal inspection usually will reveal the presence of large blood clots, which should be removed with warm saline irrigation, suction, and cotton-tipped applicators.
Adequate anesthesia and vasoconstriction should be obtained before the complete internal examination. This is best achieved with topical agents administered as sprays, impregnated cotton-tipped applicators, or local injections. Cocaine in a 5 or 10 percent solution, though often difficult to obtain, is a highly effective single therapy appropriate for both vasoconstriction and analgesia. Alternatives for anesthesia include intranasal topical lidocaine (Xylocaine), bupivacaine (Marcaine), and pontocaine (Opticaine) spray. Topical vasoconstrictors, such as oxymetazoline (Afrin) and phenylephrine hydrochloride (Neo-Synephrine) are useful adjuncts for controlling bleeding and decreasing intranasal edema.7,11 Some experts report that a 1:1 mixture of the topical decongestant oxymetazoline or phenylephrine and 4 percent topical lidocaine (liquid) is as effective as cocaine.
During the internal examination, the physician should assess nasal airway patency and should determine if ongoing epistaxis or septal deformities are present. The turbinates and inferior meatus should be visualized bilaterally, and the septum must be carefully inspected for septal hematomas. Finally, any mucosal lacerations should be noted because they may suggest an underlying fracture.
IMAGING STUDIES
When an uncomplicated nasal fracture is suspected, plain radiography rarely is indicated. In fact, because of poor sensitivity and specificity, plain radiography may serve only to confuse the clinical picture.4 Plain radiography will not allow identification of cartilaginous disruptions, and physicians may misinterpret normal suture lines as nondisplaced fractures. However, when findings such as CSF rhinorrhea, extraocular movement abnormalities, or malocclusion are present, radiologic imaging by CT is indicated to assess for facial and mandibular fractures.9
Management
Treatment begins with management of external soft tissue injuries. If an open wound is present and appears to be contaminated with foreign matter, copious irrigation will be required. Some debridement also may be necessary. However, debridement should be done judiciously because tissue will be needed to cover any exposed cartilage.
Reduction of acute nasal fractures in the primary care setting is confined largely to the closed reduction of mild unilateral fractures. However, on rare occasions, open reduction in an operating room is necessary. It is worthwhile for family physicians to understand how closed reduction of a nasal fracture is performed, although it is not considered a standard family medicine procedure. Physicians who anticipate performing open or closed reductions should gain experience and training before attempting these procedures.
The goal of closed reduction is to realign cartilaginous and bony structures to their locations before the injury to decrease discomfort and maximize airway patency. The aesthetic outcomes of closed reduction techniques are often less than optimal, and patients should be counseled that nasal reconstruction might eventually be necessary.4 Given the obvious anxiety and pain associated with reduction, pretreatment with anxiolytic and pain medications should be considered.
Manual realignment is the easiest method of closed reduction. A few simple instruments can vastly improve outcomes in nasal fracture reduction (Figure 3). Two instruments, the Asch and the Walsham forceps, are designed to reduce the displaced septum and impacted nasal bones, respectively, although these instruments often are used interchangeably. An important drawback with these instruments is the possibility of mucosal crushing injuries and resulting hematomas that may occur between their tines.

The Boies elevator (Figure 3) offers more precision than the aforementioned forceps. When used correctly, the Boies elevator is inserted into the nostril deeply to an internally or externally displaced fracture. The blade of the elevator opposes the physician’s thumb on the outside of the nose. The physician then gently attempts to raise or depress the misaligned bones to their original configuration. The reduction may be felt as the fractured bone returns to its proper alignment.
A septal hematoma is a blood-filled cavity between the cartilage and the supporting perichondrium. If left untreated, these pockets of blood easily become infected. The resulting necrosis of the underlying cartilaginous support may result in permanent saddle nose deformity.7 When a septal hematoma is identified, it should be aspirated immediately or incised with the aid of local anesthesia (Figure 4). To prevent reaccumulation of blood, a sterile drain may be left in place. However, there is conflicting evidence regarding the benefit of using a drain.13 Splints (Figure 5) or sutures may be applied to both sides of the septum to provide pressure and support, or anterior nasal packing also may be used.1 If improperly managed, a septal hematoma may have a disastrous outcome. Therefore, the treating physician should consult with an otolaryngologist or plastic surgeon when feasible.

The physician should complete a final external and internal (endoscopic, if possible) examination before releasing a patient who has undergone manipulation and reduction of a nasal fracture. This examination should ensure alignment of the nose and the absence of significant epistaxis or hematomas. When completed, an external splint or cast should be applied to the nasal dorsum for about one week. If nasal packing is required, the physician should remember that nasal packing rarely has been associated with toxic shock syndrome.14 Accordingly, packing material should be impregnated with an antistaphylococcal ointment.
The tetanus status of all patients should be determined and managed appropriately; prophylactic antibiotics may be prescribed when indicated, such as in a grossly contaminated open fracture.5
Although most family physicians routinely will not perform closed reduction of nasal fractures, it is still important to understand the preliminary assessment and basic management principles. Furthermore, because of the uncertainty of functional and cosmetic outcomes following a nasal fracture reduction,15 referral to an otolaryngologist or plastic surgeon within three to five days post-reduction, while not absolutely necessary, usually is appropriate. Ideally, the referral should be arranged before the family physician releases the patient.