
Am Fam Physician. 2004;70(7):1337-1338
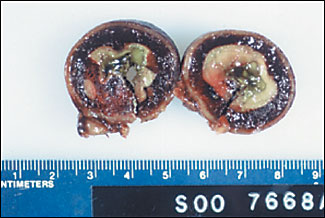
An 80-year-old woman was admitted with abdominal pain, vomiting, and generalized weakness lasting five days. The patient had no history of abdominal trauma or surgery. She was taking warfarin for chronic atrial fibrillation. On examination, her abdomen was tender and distended. Her serum potassium level was 2.4 mEq per L (2.4 mmol per L) and International Normalized Ratio (INR) was 3.17. All other laboratory parameters were within normal limits. Her abdominal radiograph revealed multiple fluid levels in the small bowel. A computed tomography (CT) scan of the abdomen was obtained (Figure 1). Normalization of serum potassium did not result in significant clinical improvement. She subsequently underwent laparotomy and bowel resection. The gross pathologic specimen of the resected bowel is shown in Figure 2.

Question
Discussion
The answer is B: intramural hematoma. Small intestinal obstruction caused by intramural hematoma is an uncommon, but well recognized, entity. In adults, approximately two thirds of these cases are preceded by abdominal trauma. The remaining one third are caused by a variety of problems, including coagulation abnormalities, pancreatic disease, alcoholism, complication from jejunal biopsy, and Henoch-Schönlein purpura.1 Spontaneous occurrence of intramural hematoma (Figure 1, arrow), usually is caused by warfarin toxicity.2 To date, more than 100 such cases of intramural hematoma have been reported in the medical literature.3 The sites most frequently involved are the duodenum and proximal jejunum, which have been attributed to the relative immobility of these parts of the small intestine.3 In children, blunt abdominal trauma, accidental or inflicted (child abuse), is the most common cause.4 Typical symptoms include abdominal pain, nausea, vomiting, and constipation. Laboratory tests should include measurement of the INR in any patient on anticoagulation therapy. Contrast-enhanced CT scan of the abdomen and pelvis may show thickening of the bowel wall.5 Medically stable patients with intramural hematoma usually are managed conservatively with bowel rest. Patients on anticoagulation should have their coagulation parameters normalized where possible.3,5 Should the patient fail to improve or deteriorate, surgical intervention may become necessary.2–5 In cases associated with trauma, prompt operative intervention is typical.6
Strangulation of a hernia results in compromise to the blood supply of the contents of the sac (e.g., omentum or intestine). Femoral hernias are the most likely type to be complicated by strangulation, which is a surgical emergency and requires urgent operative intervention.
Volvulus results from rotation of bowel loops about a fixed point resulting in partial or complete obstruction of the bowel lumen. It often is the consequence of congenital anomalies or acquired adhesions. Volvulus most commonly involves the sigmoid colon, though the cecum also may be involved. Most cases of sigmoid volvulus can be treated conservatively by barium enema or endoscopy to release the volvulus. Return of flatus and feces indicates a reversal of twist. Cecal volvulus is best treated by laparotomy and right hemicolectomy.
Intestinal obstruction secondary to adhesions is the most common cause of small bowel obstruction in adults. Adhesions usually are acquired from abdominal surgery or as a consequence of inflammatory conditions such as Crohn’s disease and endometriosis. Congenital bands may be a causal factor in children. Intestinal obstruction usually is treated conservatively, but surgical intervention may be required. Intramural hematoma would not be seen because of simple mechanical obstruction.
Mesenteric artery embolism most frequently is caused by a dislodged thrombus from the left atrium, left ventricle, or cardiac valves. The superior mesenteric artery is anatomically the most susceptible to embolic occlusion. Rapid diagnosis is essential to prevent intestinal infarction and its attendant sequelae. Unfortunately, the early signs and symptoms of mesenteric artery embolism may be nonspecific, and definitive diagnosis may not be possible without invasive testing. Available modes of treatment include bowel-sparing approaches such as surgical laparotomy with embolectomy or local infusion of thrombolytic agents via an abdominal aortic catheter. While this patient’s symptoms and advanced age could suggest mesenteric ischemia, the intramural hematoma seen on CT imaging would not be consistent.
| Condition | Characteristics |
|---|---|
| Strangulated hernia | Nonviable bowel in a hernial sac that also can compromise blood supply |
| Intramural hematoma | Spontaneous bleeding into the bowel wall usually caused by excessive anticoagulation |
| Volvulus | Twisted bowel most commonly involves sigmoid colon; usually treated with endoscopy or barium enema |
| Adhesions | Scar tissue causing “kinking” usually acquired from abdominal surgery or intra-abdominal inflammation |
| Mesenteric artery embolism | Thromboembolism commonly involving superior mesenteric artery causing massive edema or infarction of bowel; often in a patient with pre-existing cardiac thrombus |