
Am Fam Physician. 2005;71(8):1587-1588
Clinical Question
Does this patient with shoulder pain have a rotator cuff tear?
Evidence Summary
As with many conditions, single physical examination maneuvers rarely are sensitive enough to rule out disease when absent or specific enough to rule in disease when present. By themselves, these maneuvers increase or decrease the likelihood of disease slightly, and it remains up to the physician to integrate a series of findings into an estimate of the probability of disease.
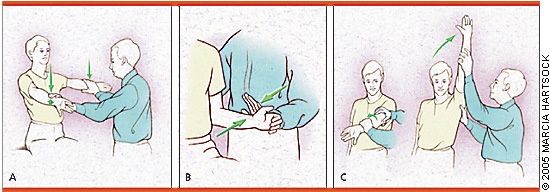
Clinical decision rules help physicians by integrating the most helpful findings into a single, easy-to-use algorithm, rule, or scoring system. Two systems for the evaluation of patients with shoulder pain are presented in this article. The authors of the first clinical rule1 began by assessing 23 maneuvers for evaluating the shoulder. They defined weakness as any score below 5 (full strength) on a 1 to 5 scale.1 All patients underwent arthros-copy as the reference standard. The authors then identified the first 100 patients with a partial- or full-thickness rotator cuff tear of any size and no other shoulder pathology, and the first 100 patients without a tear. Only three maneuvers distinguished between the two groups: supraspinatus weakness, weakness in external rotation, and a positive impingement sign1 (Figure 1). Next they evaluated these three physical findings in two larger groups of patients with shoulder pain: (1) a group of 200 patients with rotator cuff tear, including some who had additional shoulder pathology and (2) a group of 200 patients without a tear.1
The results of the second evaluation are shown in Table 1,1 stratified by the number of abnormal physical findings and patient age. Older patients were more likely to have a rotator cuff tear than younger patients. The probability of rotator cuff tear was high (98 percent) in patients of any age with all three findings or in patients with any two findings who were at least 60 years of age. The probability was 5 percent in the 97 patients who had none of the three findings.
| Number of positive symptoms or signs* | Age (years) | Number of patients in this group | Probability of rotator cuff tear (%) (95% CI) |
|---|---|---|---|
| All 3 | Any | 49 | 98 (89 to 100) |
| Any 2 | ≥ 60 | 49 | 98 (89 to 100) |
| Any 2 | < 60 | 40 | 64 (47 to 79) |
| Any 1 | ≥ 70 | 28 | 76 (56 to 90) |
| Any 1 | 40 to 69 | 112 | 45 (36 to 55) |
| Any 1 | < 40 | 25 | 12 (25 to 31) |
| None | Any | 97 | 5 (2 to 11) |
The second clinical decision rule2 used data from a retrospective chart review. Typically, this type of study is methodologically weak because of the inconsistent nature of most medical records; however, in this case, the orthopedic physicians used a standard form to record information about the history and physical examination. The methods were carefully described, and all patients underwent arthrography as a reference standard. The researchers developed a multivariate model using 191 patients, finding that the best predictors of rotator cuff injury were age older than 65 years, night pain, and weakness with external rotation.2 Then, they simplified the model into a five-point score and tested it on the remaining 216 patients. The final score and its interpretation are shown in Table 2.2 The mean age of patients in this study was 57 years, and 67 percent overall had a partial or complete rotator cuff tear.2
Both clinical decision rules relied on older age and weakness on external rotation. The first rule1 used prospective data collection, which generally is better than retrospective chart review, but the second rule2 used reliable methods for their chart review and did a more extensive validation of their decision rule. Although a prospective validation in a new population comparing the two rules would be ideal, given the poor performance of individual physical findings it is reasonable to use either or both of these rules when estimating the likelihood of rotator cuff tear.
Finally, the “painful arc sign” has high sensitivity (97.5 percent) as a single finding, making it helpful in ruling out rotator cuff tears when absent.2 The test is performed by having the examiner elevate the patient's arm passively to 180°. The patient is then asked to lower the arm actively. The sign is positive if the patient has minimal pain initially at full elevation, increasing pain between 70° and 120°, and then decreasing pain as the arm is lowered further.