
Am Fam Physician. 2005;71(10):1984-1986
A 22-year-old man presented with complaints of a worsening cough and shortness of breath. The cough was nonproductive and he had experienced increasing dyspnea with exertion for the past four months. The symptoms had worsened despite treatment for an upper respiratory infection and a completed course of macrolide antibiotics for presumed community-acquired pneumonia. He denied having fever, night sweats, or tuberculosis exposure, but he had lost weight. He did not use tobacco. Physical examination findings were significant for cachexia, decreased breath sounds in the right middle and lower lung fields without audible wheezing or stridor, and a room-air pulse oximetry reading in the mid 90s. His thyroid and testicular examinations were normal, and no clubbing or lymphadenopathy was noted. Chest radiography revealed a large anterior mediastinal mass (Figures 1 and 2).


Question
Discussion
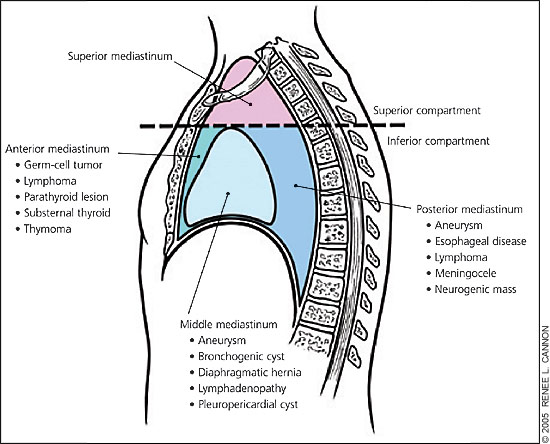
The answer is C: histoplasmosis. Histoplasmosis is one of the many infectious causes of middle mediastinal lymphadenopathy. The mediastinum is divided anatomically into inferior and superior compartments. The inferior compartment is further subdivided into three main compartments1: anterior,2 middle,3 and posterior mediastinum2 (Figure 3). The most common causes of anterior mediastinal masses are the four Ts: thymomas, teratomas, “terrible” lymphomas, and thyroid.
Thymomas are the most common primary tumors of the anterior mediastinum. They are found most often in patients 40 to 60 years of age and rarely occur in patients younger than 20 years. They have an equal prevalence in men and women.3 Most often located in the upper anterior mediastinum, thymomas typically are slow-growing, non-aggressive tumors. Size varies from very small tumors to large masses, which rarely are calcified (7 percent). Approximately 35 to 50 percent of patients present asymptomatically, with incidental discovery on routine chest radiography.4 Approximately 25 to 30 percent of patients present with symptoms of parathymic syndromes such as myasthenia gravis, pure red cell aplasia (21 to 50 percent), or hypogammaglobulinemia (10 to 15 percent). The final 35 percent of patients present with symptoms associated with compression or invasion of thoracic structures, such as chest pain, dyspnea, or cough.5 Treatment consists of surgical excision with radiation and chemotherapy depending on tumor stage.
Teratomas are germ-cell neoplasms and account for 15 percent of anterior mediastinal tumors in adults and 25 percent in children.2 They are composed of several different embryonic cell layers. Benign (mature) teratomas contain three tissue types undergoing differentiation: ectoderm (skin, squamous epithelium), mesoderm (bone, cartilage, muscle, teeth), and endoderm (gastrointestinal, respiratory, mucous glands). These tumors make up the majority (75 percent) of mediastinal germ-cell tumors and usually present in young adults. The prevalence is the same in men and women.2 The tumors usually are large, round, and lobulated with sharp marginations. Up to 60 percent of tumors are asymptomatic and discovered incidentally.2 Therapy consists of surgical excision with a five-year survival rate approaching 100 percent.
Malignant (immature) teratomas make up only 1 percent of mediastinal teratomas and usually are found in children and adolescents.1 Seminomas are the most common malignant germ-cell tumor. Usually occurring in men older than 30 years, these tumors have a much better prognosis than nonseminomatous tumors. All men with mediastinal lung masses require a careful testicular examination. Tumor markers such as human chorionic gonadotropin (choriocarcinoma) and alpha fetoprotein (embryonal cell carcinoma, yolk sac tumor) may aid in diagnosis.1
Thyroid and parathyroid masses commonly present as tumors in the superior aspect of the anterior compartment. They usually cause tracheal deviation at the thoracic outlet noted on chest radiography. Computed tomography (CT) and thyroid scans are helpful in localization and diagnosis. Treatment is surgical excision, which has an excellent prognosis.
Lymphomas account for 10 to 20 percent of all anterior mediastinal masses. They are the most common primary mediastinal tumors in adults between 30 and 40 years of age, but are also the second most common anterior mediastinal masses noted in children.4 Lymphomas are subclassified further into Hodgkin’s and non-Hodgkin’s lymphomas. Hodgkin’s disease is also the most common lymphoma affecting the middle mediastinum.
Radiographically, lymphomas appear to be indistinguishable from the other anterior mediastinal masses. A helpful tip is that pleural effusions are common in lymphomas but rare in the other common masses.6 Calcifications are also a rare finding in lymphomas unless the patient was treated previously for lymphoma. Diagnosis is suggested by the finding of a lobulated mass on CT and confirmed by tissue samples. Treatment consists of chemotherapy and/or radiotherapy with five-year survival rates approximating 75 percent.
In this patient, CT scan confirmed the presence of an anterior mediastinal mass with a right-sided pleural effusion. Cytopathology of the pleural fluid showed mesothelial cells with abundant lymphoid cells. The final diagnosis was lymphoma.
| Condition | Characteristics |
|---|---|
| Thymoma | Upper anterior mediastinum, slow growing, size varies, most often found incidentally |
| Teratoma | Large, round, lobulated, often an incidental finding |
| Thyroid, parathyroid | Superior anterior mediastinum, tracheal deviation at the thoracic outlet |
| “Terrible” lymphoma | Pleural effusion common, calcifications rare |