
Am Fam Physician. 2005;72(7):1299-1300
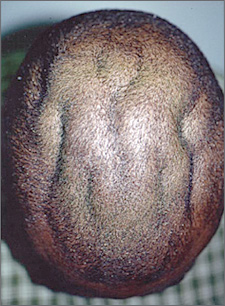
A 15-year-old adolescent presented with concerns about the appearance of his scalp (see accompanying figure). The patient wished to know what was causing the skinfolds because schoolmates were teasing him, calling him “Klingon Head.” The skinfolds first appeared in late childhood, and as he grew older, they grew in conjunction with his head size. Family history did not reveal any other family members with similar findings. On physical examination, the patient was obese but in good health.
Question
Discussion
The answer is A: cutis verticis gyrata. Cutis verticis gyrata is a descriptive diagnosis for an abnormal-appearing overgrowth of the scalp in relation to the skull. Biopsies usually show a thickened dermis with possible sebaceous hyperplasia, with or without collagen excess.1,2 No medical treatment is needed; the skin is simply too large for the head. Plastic surgery consultation can be considered for cosmetic reasons.
Primary cutis verticis gyrata almost always occurs in males. It may be genetic, although its mode of inheritance is uncertain.1 The skin findings may appear in late childhood or during puberty and slowly become more accentuated.
Cutis verticis gyrata can occur in genetically inherited syndromes such as pachydermoperiostosis (hypertrophic osteoarthropathy or Touraine-Solente-Golé syndrome) and Rosenthal-Kloepfer syndrome (acromegaloid phenotype with cutis verticis gyrata and corneal leukoma).3 Endocrine disorders associated with secondary cutis verticis gyrata include acromegaly, cretinism, and myxedema.4 Paraneoplastic syndromes can be another secondary cause.5
Most often, patients with cutis verticis gyrata are of normal intelligence, although its preponderance is greater in patients with intellectual disabilities. It affects 0.5 percent of the intellectually disabled populations in Scotland, Sweden, and the United States.1
Differential diagnosis includes, but is not limited to, nevus sebaceous, pilar cyst, lipoma, nevus of Ota, and cerebriform nevus. Nevus sebaceous usually develops earlier in life and appears as a papulated growth with a nevoid appearance. Pilar cysts and lipomas may form on the scalp, but typically are localized masses unlikely to cause uniform changes to the entire scalp. Nevus of Ota is a congenital hyperpigmented patch that usually is found in the ophthalmomaxillary region, hence the name nevus fuscoceruleus ophthalmomaxillaris. Cerebriform nevus appears at birth and does not present on the entire scalp.
| Condition | Characteristics |
|---|---|
| Cutis verticis gyrata | Excess skin on scalp |
| Pilar cyst (wen) | Cystic mass, moves freely |
| Nevus of Ota | Large hyperpigmented patch |
| Cerebriform nevus | Small to medium plaque |
| Lipoma | Firm, movable nodule |