
Am Fam Physician. 2005;72(12):2517-2518
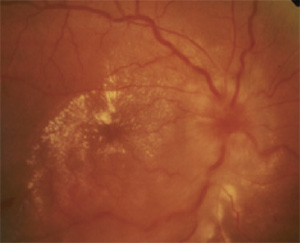
A 47-year-old woman developed sudden-onset disturbances in color and brightness perception in her right eye. Her medical and ocular histories were unremarkable. She denied any preceding illness and had no history of recent exposure to cats or other animals. On examination, visual acuity was 20/40 in her right eye and 20/20 in her left eye. Color desaturation was present in her right eye. There was no afferent pupillary defect. Visual field examination by confrontation showed an enlarged blind spot in her right eye. Right optic disc swelling with congested vessels and hard exudates at the macular area were found (Figure 1). The left fundus was normal (Figure 2), and the remaining eye examinations revealed no other abnormalities.
The patient's blood pressure was 150/90 mm Hg; otherwise the physical examination was normal. Complete blood count, erythrocyte sedimentation rate, glucose, and liver and renal function tests were all within normal limits. Tests for antinuclear antibodies, rheumatoid factor, syphilis, toxoplasmosis, and Lyme disease were negative. Results of chest radiography were normal.
Question
Discussion
The correct answer is D: neuroretinitis. Optic disc swelling and star-shaped macular exudates describe the findings of neuroretinitis. In this case, it was idiopathic and the patient made a complete recovery by one year without specific treatment.
Most cases of neuroretinitis are idiopathic; however, the diagnosis requires excluding the most common infectious causes: syphilis, toxoplasmosis, cat-scratch disease, and Lyme disease.1 Hepatitis B and tuberculosis also have been reported to cause neuroretinitis. The differential diagnosis for unilateral optic disc swelling with macular star includes hypertensive retinopathy, diabetic optic neuropathy, papillophlebitis, anterior ischemic optic neuropathy, optic neuritis of infectious and noninfectious origin, optic nerve head tumors, and neuroretinitis.1,2
In 1916, Leber3 described patients with unilateral vision loss, optic disc edema, and macular stars. These patients had no identifiable causes for these symptoms and their vision recovered spontaneously. The pathogenic locus of this syndrome later was found to be at the optic nerve head, and the observed exudate resulted from leakage of the disc capillaries that had extended into the macular area along the plane of the outer plexiform layer.4 The serous component of the exudate resorbed, whereas the residual lipids and proteins formed the characteristic macular star.
Neuroretinitis usually occurs in children and young adults; both sexes are involved equally. The initial visual acuity typically ranges from 20/50 to 20/200, and there can be an afferent pupillary defect.4 Most cases are unilateral, with bilateral involvement reported in 5 to 33 percent of patients.1 Affected persons usually are healthy. Neuroretinitis is believed to be caused by a non-specific viral infection because associated flu-like symptoms occur in about one half of patients. Optic disc swelling is the earliest sign and usually is diffuse. The macular star may be present at the onset of disease or may not be apparent until one to two weeks later.
The visual prognosis generally is good. Unlike optic neuritis, the chance of developing multiple sclerosis is very low.2 Treatment is not necessary in most cases with the exception of appropriate antibiotics if an infectious cause is identified. The role of corticosteroids and immunosuppressive agents is not clear, but these agents may be considered in recurrent cases.5
The other differential diagnoses are not compatible with the clinical presentation. Hypertensive papilledema, brain tumor, or any other etiologies resulting in high intracranial pressure commonly are associated with bilateral optic disc swelling. Optic neuritis has prominent relative afferent pupillary defect of the involved eye, and it seldom causes any macular exudates or macular star. Ischemic optic neuropathy also has a remarkable relative afferent pupillary defect. Disc swelling may not be uniform or may be pale in color if the underlying disease is giant cell arteritis.
| Condition | Characteristics |
|---|---|
| Brain tumor | Good visual acuities, optic disc swelling often bilateral and symmetric |
| Optic neuritis | Positive relative afferent pupillary defect, not associated with macular exudates |
| Hypertensive papilledema | Enlarged blind spot, flame-shape hemorrhage, cotton wool spot, bilateral involvement |
| Neuroretinitis | Macular star, hyperemic disc, congested retinal vein |
| Anterior ischemic optic neuropathy | Prominent relative afferent pupillary defect, disc swelling may be sectorial or pale in case of giant cell arteritis |