
A more recent article on developmental dysplasia of the hip is available.
Am Fam Physician. 2006;74(8):1310-1316
Patient information: See related handout on hip problems in infants.
Author disclosure: nothing to disclose.
Developmental dysplasia of the hip refers to a continuum of abnormalities in the immature hip that can range from subtle dysplasia to dislocation. The identification of risk factors, including breech presentation and family history, should heighten a physician’s suspicion of developmental dysplasia of the hip. Diagnosis is made by physical examination. Palpable hip instability, unequal leg lengths, and asymmetric thigh skinfolds may be present in newborns with a hip dislocation, whereas gait abnormalities and limited hip abduction are more common in older children. The role of ultrasonography is controversial, but it generally is used to confirm diagnosis and assess hip development once treatment is initiated. Bracing is first-line treatment in children younger than six months. Surgery is an option for children in whom nonoperative treatment has failed and in children diagnosed after six months of age. It is important to diagnose developmental dysplasia of the hip early to improve treatment results and to decrease the risk of complications.
The term developmental dysplasia of the hip (DDH) has replaced congenital dislocation of the hip because it more accurately reflects the full spectrum of abnormalities that affect the immature hip. DDH can predispose a child to premature degenerative changes and painful arthritis. Careful physical examination is recommended as a screening tool; early diagnosis helps improve treatment results and decrease the risk of complications.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Risk factors for DDH should be identified in all children. | C | 12 |
| A careful physical examination is the basis for screening for DDH. | C | 12 |
| Ultrasonography should be ordered for infants six weeks to six months of age to clarify a clinical finding suggestive of DDH, assess a high-risk infant, and monitor DDH as it is observed or treated. | C | 12 |
Definitions
Hip dysplasia refers to an abnormality in the size, shape, orientation, or organization of the femoral head, acetabulum, or both. Acetabular dysplasia is characterized by an immature, shallow acetabulum and can result in subluxation or dislocation of the femoral head. In a subluxed hip, the femoral head is displaced from its normal position but still makes contact with a portion of the acetabulum. With a dislocated hip, there is no contact between the articular surface of the femoral head and the acetabulum. An unstable hip is one that is reduced in the acetabulum but can be provoked to subluxate or dislocate. Teratologic hip dysplasia, which is outside the scope of this discussion, refers to the more severe, fixed dislocation that occurs prenatally, usually in those with genetic or neuromuscular disorders.
Epidemiology and Etiology
The incidence of DDH is variable and depends on many factors. Approximately one in 1,000 children is born with a dislocated hip, and 10 in 1,000 may have hip subluxation.1–3 Factors contributing to DDH include breech presentation, female sex, positive family history, firstborn status, and oligohydramnios. Intrauterine position, sex, race, and positive family history are the most important risk factors.
A family history positive for DDH may be found in 12 to 33 percent of affected patients.4,5 The risk of DDH for a child has been documented at 6 percent when there is one affected sibling, 12 percent with one affected parent, and 36 percent if a parent and a sibling are affected.6 Eighty percent of children with DDH are females.7 This is postulated to be related to the effects of additional estrogen produced by the female fetus, which increases ligamentous laxity.
The left hip is affected in 60 percent of children, the right hip in 20 percent, and both hips in 20 percent.8 The left hip is more commonly involved because it is adducted against the mother’s lumbosacral spine in the most common intrauterine position (i.e., left occiput anterior).
DDH occurs more often in children who present in the breech position.9 It is believed that in utero knee extension of the infant in the breech position results in sustained hamstring forces around the hip and contributes to subsequent hip instability. First-born children are affected twice as often as subsequent siblings, presumably because of an unstretched uterus and tight abdominal structures in the mother. In utero postural deformities and oligohydramnios also are associated with DDH. For unknown reasons, DDH is less common in black persons.10
The postnatal extrauterine environment also plays a role in DDH. The incidence of DDH is high in Native American cultures that use swaddling, which forces the hips into adduction and extension.11
Physical Examination
No first-line method exists for diagnosing DDH during the newborn period. However, a careful physical examination is recommended as a screening tool, particularly for high-risk infants.12 Evaluation of the hip begins with observation of both lower extremities.12 The diaper should be removed and the infant relaxed. Provocative dynamic tests, such as the Ortolani and Barlow maneuvers, should be performed to assess its stability.13 Because these tests often are difficult to interpret, they should be performed routinely in children three months or younger.
Each hip must be examined separately. The child should be supine with the hips flexed to 90 degrees. The examiner should place his or her index and long fingers laterally over the child’s greater trochanter with the thumb medially along the inner thigh near the groin crease. The examiner stabilizes the child’s pelvis by holding the contralateral hip still while the opposite hand examines the hip. The examiner should gently abduct the hip being tested while simultaneously exerting an upward force through the greater trochanter laterally (Figure 1). The sensation of a palpable “clunk” is a positive Ortolani test and represents the reduction of a dislocated hip into the bony acetabulum.

To perform the Barlow test, the pelvis is stabilized and the patient is positioned similar to the Ortolani test position. The difference is that the examiner adducts the child’s hip and exerts a gentle downward force in an attempt to subluxate or dislocate an unstable hip posteriorly (Figure 1). These tests generally are only useful in infants three months or younger. Thereafter, soft-tissue contractures limit the motion of the hip, even if it is dislocated.
In the first few months of life, an unstable hip may be noted on physical examination. If the Ortolani or Barlow test is equivocal or inconclusive on examination at birth, the physician should have the newborn return for follow-up in two weeks.12
Asymmetric skinfolds or leg length inequality are common findings with unilateral hip dislocation (Figure 2), although asymmetric skinfolds are not specific to DDH. The Galeazzi sign is elicited by placing the child supine with both hips and knees flexed (Figure 3). An inequality in the height of the knees is a positive Galeazzi sign and usually is caused by hip dislocation or congenital femoral shortening. An infant with hip dislocation will develop limited hip abduction on the affected side by three months of age (Figure 4). Maximal abduction of the hips should be greater than 60 degrees, or a dislocated hip should be suspected.


Noting limited abduction is particularly important in identifying children with bilateral hip dislocations because the leg lengths (i.e., Galeazzi sign) are equal. In addition, in children who are walking, Trendelenburg’s symptom (a limp on the affected side) may be the first sign of a dislocated hip. In children with established dislocations, the action of the gluteus medius in pulling the pelvis downwards in the stance phase is ineffective or weak because of a lack of a stable fulcrum.
For a child with a right hip dislocation, the pelvis drops on the opposite side (i.e., left), causing instability. To restore the stability and prevent falls to the left, the body lurches to the right side and shifts the center of gravity over the stance side (i.e., right hip). The top of the greater trochanter telescopes upward and mechanically hitches on the ilium to stabilize the joint. This movement at every stance phase is called the Trendelenburg gait.14
Radiographic Examination
Radiographs of newborns with suspected DDH are of limited value because the femoral heads do not ossify until four to six months of age. Ultrasonography is the study of choice to evaluate for DDH in infants younger than six months because it is capable of visualizing the cartilaginous anatomy of the femoral head and acetabulum.15–17 It is useful in identifying dysplasia of the cartilaginous portion of the acetabulum, confirming subluxation of the hip, and documenting reducibility and stability of the hip in the infant undergoing treatment for known DDH. Ultrasonography is overly sensitive as a screening tool in the first six weeks of life, and in general should not be ordered until after that.18
Plain radiographs are useful after four to six months of age. Several reference lines and angles are useful in evaluating the anteroposterior radiograph of the infant’s pelvis (Figure 5). Hilgenreiner’s line is drawn horizontally through the triradiate cartilages of the pelvis. Perkin’s line is drawn perpendicular to Hilgenreiner’s line at the lateral edge of each acetabulum. The femoral head should lie within the inferomedial quadrant formed by Hilgrenreiner’s and Perkin’s lines. In a dysplastic hip, the lateral edge of the acetabulum may be difficult to identify, and the femoral head may lie in the superior or lateral quadrants.
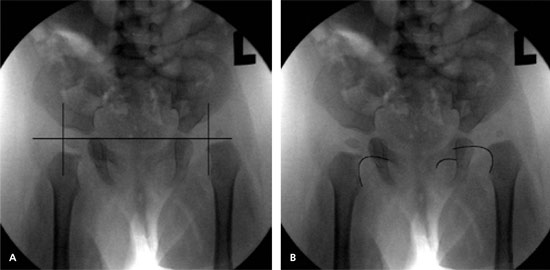
Shenton’s line is curvilinear. It is defined by the medial border of the femoral neck and the superior border of the obturator foramen. A break in Shenton’s line suggests displacement of the femoral head from the bony acetabulum (Figure 5).
The U.S. Preventive Services Task Force (USPSTF) recently concluded that evidence is insufficient to recommend routine screening for DDH in infants as a means to prevent adverse outcomes. Evidence shows that screening leads to earlier identification of DDH; however, the USPSTF concluded that 60 to 80 percent of the newborn hips identified by physical examination and more than 90 percent identified by ultrasonography as abnormal or as suspicious for DDH resolve spontaneously and require no intervention.19
Management
The goal of treatment in DDH is to achieve and maintain reduction of the femoral head in the true acetabulum by closed or open means. The earlier treatment is initiated, the greater the success and the lower the incidence of residual dysplasia and long-term complications.
Subluxation of the hip at birth often corrects spontaneously and may be observed for two weeks without treatment. The double- or triple-diaper technique, which theoretically prevents hip adduction, has not demonstrated improved results when compared with no intervention at all. When subluxation persists beyond two weeks of age, treatment is indicated and the appropriate referral should be made.12
In newborns and infants up to six months of age, closed reduction and immobilization in a Pavlik harness is the treatment of choice (Figure 6). The Pavlik harness dynamically positions the hips in flexion and abduction while allowing motion. Avascular necrosis of the femoral head has been reported with Pavlik harness treatment and may be related to hyperabduction.20 In addition, hyperflexion has the potential to cause femoral nerve palsies.

Reduction of the hip should be confirmed by ultrasonography within three weeks of harness placement. Treatment usually is continued for at least six weeks full-time and six weeks part-time in young infants, and possibly longer in older children. The end point of brace treatment is a stable hip with normal imaging studies. If a dislocated hip is not reduced within three weeks, the harness should be discontinued and an alternative treatment selected. This usually involves closed reduction under anesthesia with hip spica casting (Figure 7).21

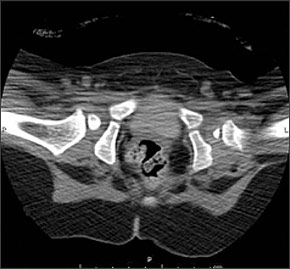
In children older than six months, closed reduction under general anesthesia and hip spica casting is the treatment of choice. Postoperative computed tomography or magnetic resonance imaging should be used to confirm concentric reduction (Figure 8).24,25 Immobilization in the hip spica cast after closed reduction usually continues for at least 12 weeks after closed reduction.26
If the hip is irreducible by closed means, or a concentric reduction is not achieved, successful treatment requires open reduction.27 Open reduction of the hip in a child with DDH involves lengthening tendons about the hip, removing obstacles to reduction, and tightening the hip capsule once reduction is obtained. Complications include femoral head osteonecrosis and redislocation.28 Surgery becomes more technically demanding in older children with established dislocations. By 18 months, femoral osteotomies with or without pelvic osteotomies may be necessary to reconstruct and safely maintain the hip in a reduced position.
The goal of operative treatment of DDH is to normalize the hip joint to delay or prevent the premature onset of osteoarthritis. Intervention in early childhood, when remodeling potential is greater, provides the best opportunity for the development of a normal joint.29 Children with untreated hip dysplasia have been shown to develop premature degenerative changes by the time they reach skeletal maturity, and develop painful arthritis in their thirties.30 Children with hip dysplasia who are diagnosed in adolescence and undergo surgical treatment fare somewhat better but often require secondary procedures as adults for painful arthritis.31
Joint-preserving salvage osteotomies and total hip arthroplasty are surgical options once a child has achieved skeletal maturity. Both procedures have mixed long-term results and are inferior to surgical treatment initiated at earlier ages.32,33 Children in whom Pavlik harness treatment is initiated before six months of age have excellent results, although long-term studies are lacking. The majority have no symptoms of arthritis, with mild radiographic abnormalities by skeletal maturity.34,35 A child with DDH usually requires long-term follow-up with radiographic evaluation until skeletal maturity is reached to ensure normal hip development.36–38
In general, the goal of the family physician in examining for DDH should be early diagnosis and referral. This is because treatment earlier in life, especially within the first six months, is safer and more successful than treatment after the child is walking.