
Am Fam Physician. 2007;75(4):509-512
A more recent article on common oral lesions is available.
This is part II of a two-part article on oral lesions. Part I, “Superficial Mucosal Lesions,” appears in this issue of AFP on page 501.
Certain common oral lesions appear as masses, prompting concern about oral carcinoma. Many are benign, although some (e.g., leukoplakia) may represent neoplasia or cancer. Palatal and mandibular tori are bony protuberances and are benign anomalies. Oral pyogenic granulomas may appear in response to local irritation, trauma, or hormonal changes of pregnancy. Mucoceles represent mucin spillage into the oral soft tissues resulting from rupture of a salivary gland duct. Oral fibromas form as a result of irritation or masticatory trauma, especially along the buccal occlusal line. Oral cancer may appear clinically as a subtle mucosal change or as an obvious mass. Oral leukoplakia is the most common premalignant oral lesion. For persistent white or erythematous oral lesions, biopsy should be performed to rule out neoplastic change or cancer. Most oral cancers are squamous cell carcinomas. Tobacco and heavy alcohol use are the principal risk factors for oral cancer. Family physicians should be able to recognize these lesions and make appropriate referrals for biopsy and treatment.
Physicians regularly encounter oral health issues in practice. Part I of this two-part series discusses superficial mucosal lesions such as candidiasis and herpes labialis.1 This article reviews common oral lesions that may appear as masses or represent neoplastic change (Table 1).2–8 Many of these are benign conditions. Neoplastic or cancerous oral lesions may appear as white or erythematous patches, ulcerated lesions, or masses. Family physicians should be able to recognize these lesions and make appropriate referrals for biopsy and treatment. Differentiating benign from worrisome lesions and providing appropriate counseling regarding risk factors (e.g., tobacco use) is central to achieving national oral health goals.9
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Observation is appropriate for pregnancy-related oral pyogenic granulomas because they have a high recurrence rate with excision and often resolve after parturition. | C | 4, 13 |
| For persistent erythematous or white oral lesions, biopsy should be performed. | C | 7 |
| Condition | Clinical presentation | Treatment | Comment |
|---|---|---|---|
| Palatal and mandibular tori2,3 | Bony protuberances of the palate or lingual aspect of the mandible | Removal required only if interferes with function or denture fabrication, or is subject to recurrent trauma | Developmental anomaly |
| Pyogenic granuloma4 | Rapidly growing, red, lobulated mass | Refer for surgical excision; observe in pregnancy unless excision warranted (e.g., excessive bleeding) | Possible postpartum regression |
| Mucocele5 | Bluish, fluctuant mucosal swelling, often with a history of periodic rupture | Excision of lesion and adjacent “feeder” minor salivary glands | Pathologic examination of specimen required |
| Fibroma6 | Firm, pink, smooth-surfaced nodule | Excision | Pathologic examination required |
| Leukoplakia7 | White patch that does not wipe off | Refer for biopsy and surgical excision | No evidence that surgical excision prevents malignant transformation |
| Erythroplakia7 | Red patch without obvious cause | Refer for biopsy and surgical excision | No evidence that surgical excision prevents malignant transformation |
| Squamous cell carcinoma8 | Nonhealing ulcer or mass | Refer for biopsy, staging, surgery, and treatment | — |
Palatal and Mandibular Tori
Tori are benign, nonneoplastic, bony protuberances that arise from the cortical plate. They sometimes are mistaken for malignancies. These exostoses are considered developmental anomalies, although they usually do not appear until adulthood. A torus located along the midline of the hard palate is called a palatal torus, or torus palatinus (Figure 1), and a torus located along the lingual aspect of the mandible is called a mandibular torus, or torus mandibularis (Figure 2). Palatal tori are reported in 20 to 35 percent of the U.S. population, whereas mandibular tori are reported in 7 to 10 percent.2,3 Removal is required only if a torus interferes with function or denture fabrication, or is subject to recurrent traumatic surface ulceration.10


Pyogenic Granuloma
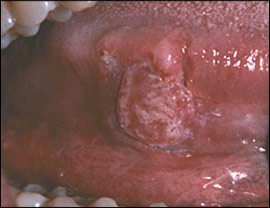
A pyogenic granuloma is a rapidly growing lesion that develops as a response to local irritation (e.g., poor hygiene, overhanging dental fillings), trauma, or increased hormone levels in pregnancy.11 It is an erythematous, non-painful, smooth or lobulated mass that often bleeds easily when touched (Figure 3). Oral pyogenic granulomas most often develop on the gingiva, but less common locations include the lip, tongue, and buccal mucosa.12 They may vary in diameter from a few millimeters to several centimeters. Surgical excision usually is adequate because recurrence is uncommon unless the lesion or local sources of irritation are inadequately removed. Observation is more appropriate in pregnant women because many pyogenic granulomas resolve after the birth.13 Excessive bleeding or other considerations may prompt excision. However, lesions excised during pregnancy are more likely to recur (because of the hormone effect).4

Mucocele
A mucocele is an area of mucin spillage in soft tissue resulting from rupture of a salivary gland duct. Children and young adults are most commonly affected, although this lesion may occur at any age. There is often a history of local trauma (e.g., biting). Many patients describe episodes of recurrent swelling with periodic rupture. The typical clinical presentation is a bluish, dome-shaped, fluctuant mucosal swelling (Figure 4). However, if the area of mucin spillage is deeper, the overlying mucosa may be normal in color.5 Long-standing lesions may become fibrotic and therefore be firm rather than fluctuant upon palpation. The lower labial mucosa is the most common location, although any oral site with salivary gland tissue may be affected.14

Appropriate treatment consists of local surgical excision, including the removal of adjacent minor salivary glands. Pathologic examination of the excised tissue is needed to rule out neoplasia.5
Fibroma
A fibroma is a focus of hyperplastic fibrous connective tissue representing a reactive response to local irritation or masticatory trauma.6 Fibromas occur in approximately 1.2 percent of adults.10 The most common location is along the occlusal line of the buccal mucosa—an area subject to masticatory trauma—although other locations, such as the tongue, labial mucosa, and gingiva, are possible. Fibromas manifest as asymptomatic, moderately firm, smooth-surfaced, pink, sessile or pedunculated nodules (Figure 5).6 They are treated by surgical excision, and recurrence is rare.10 The removed tissue should undergo pathologic examination to rule out the possibility of neoplasms that may have a similar appearance.6

Leukoplakia, Erythroplakia, and Oral Cancer

Oral leukoplakia, the best-known pre-malignant oral lesion, is defined by the World Health Organization as “a white patch or plaque that cannot be characterized clinically or pathologically as any other disease.”15 Analogous red lesions are called erythroplakia, and combined red and white lesions are known as speckled leukoplakia or erythroleukoplakia. Erythroplakia and speckled leukoplakia are more likely than leukoplakia to exhibit dysplasia or carcinoma microscopically.16
In the United States, cancers of the oral cavity and oropharynx are the ninth most common cancer, accounting for approximately 3 percent of malignancies among men and 2 percent of malignancies among women.17 Prevalence increases with age. Approximately 90 percent of oral cancers are squamous cell carcinomas. They occur most commonly on the tongue, floor of the mouth, and vermilion border of the lower lip. Sixty percent of oral carcinomas are advanced by the time they are detected, and about 15 percent of patients have another cancer in a nearby area such as the larynx, esophagus, or lungs. Tobacco use and heavy alcohol consumption are the two principal risk factors, accounting for 75 percent of oral carcinomas.18
The evidence regarding the sensitivity, specificity, and impact of screening on morbidity and mortality is limited. Pending better evidence to guide clinical screening and intervention, a prudent course of action would be to refer patients with unclassified red or white lesions persisting longer than two weeks to an oral and maxillofacial surgeon or pathologist, or to an otolaryngologist, for evaluation, biopsy, and treatment.7
Precancerous lesions should be surgically removed, if possible. Cryotherapy and laser ablation have been used, although these methods do not allow for tissue preservation or microscopic examination. Treatment of oral squamous cell carcinoma is guided by clinical staging.8 The overall five-year survival rate for oral cancer is 50 to 55 percent.19 Long-term follow-up is advised because of the potential for recurrence or additional lesions.