
Am Fam Physician. 2007;75(5):695-700
Author disclosure: Nothing to disclose.
Erythema nodosum, a painful disorder of the subcutaneous fat, is the most common type of panniculitis. Generally, it is idiopathic, although the most common identifiable cause is streptococcal pharyngitis. Erythema nodosum may be the first sign of a systemic disease such as tuberculosis, bacterial or deep fungal infection, sarcoidosis, inflammatory bowel disease, or cancer. Certain drugs, including oral contraceptives and some antibiotics, also may be etiologic. The hallmark of erythema nodosum is tender, erythematous, subcutaneous nodules that typically are located symmetrically on the anterior surface of the lower extremities. Erythema nodosum does not ulcerate and usually resolves without atrophy or scarring. Most direct and indirect evidence supports the involvement of a type IV delayed hypersensitivity response to numerous antigens. A deep incisional or excisional biopsy specimen should be obtained for adequate visualization. Erythema nodosum represents an inflammatory process involving the septa between subcutaneous fat lobules, with an absence of vasculitis and the presence of radial granulomas. Diagnostic evaluation after comprehensive history and physical examination includes complete blood count with differential; erythrocyte sedimentation rate, C-reactive protein level, or both; testing for streptococcal infection (i.e., throat culture, rapid antigen test, antistreptolysin-O titer, and polymerase chain reaction assay); and biopsy. Patients should be stratified by risk for tuberculosis. Further evaluation (e.g., purified protein derivative test, chest radiography, stool cultures) varies based on the individual. Erythema nodosum tends to be self-limited. Any underlying disorders should be treated and supportive care provided. Pain can be managed with nonsteroidal anti-inflammatory drugs.
Erythema nodosum is a type of panniculitis that affects subcutaneous fat in the skin, usually first evident as an outcropping of erythematous nodules that are highly sensitive to touch.1 Most nodules are located symmetrically on the ventral aspect of the lower extremities. Although erythema nodosum usually has no specific documented cause, it is imperative to investigate possible triggers. Streptococcal infections are the most common identifiable etiology, especially in children. Drug and hormonal reactions, inflammatory bowel disease, and sarcoidosis are other common causes among adults.1,2 Often, erythema nodosum is a sign of a serious disorder that potentially is treatable; management of an underlying etiology is the most definitive means of alleviating erythema nodosum.
Overall, erythema nodosum occurs in approximately one to five per 100,000 persons. In adults, it is more common among women, with a male-to-female ratio of 1:6.3,4 In children, the sex ratio is 1:1.2 Peak incidence occurs in persons between 20 and 30 years of age, although erythema nodosum can occur at any age.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| The most important step in the management of erythema nodosum is treatment of the underlying disorder. | C | 1, 3 |
| Antitubercular therapy should be started presumptively for erythema nodosum in patients with a positive purified protein derivative skin test result with or without a positively identified focus of infection. | C | 11, 12 |
| In patients with erythema nodosum, pain can be managed with nonsteroidal anti-inflammatory drugs. | C | 1, 3 |
| Systemic steroids at a dosage of 1 mg per kg daily may be used until resolution of erythema nodosum if underlying infection, risk of bacterial dissemination or sepsis, and malignancy have been excluded by a thorough evaluation. | C | 1, 3 |
| Colchicine may be considered in patients with erythema nodosum and coexistent Behçet's syndrome. | C | 30 |
Clinical Manifestations
Erythema nodosum nodules vary from 0.4 to 4 inches (1 to 10 cm) in diameter and are poorly demarcated, reflecting their subcutaneous anatomic location (Table 11–4 ; Figure 1). Pretibial involvement is most common, although the extensor surfaces of the forearm, the thighs, and the trunk also may be affected. Initially, erythema nodosum nodules can be firm, but they usually become more fluctuant during the clinical evolution. Individual nodules may last for two weeks; new outcroppings may continue to arise for up to six weeks. These nodules often take approximately one to two months to heal completely and may assume a bruise-like appearance as they fade. They do not tend to ulcerate and usually resolve without atrophy or scarring.1–4
| Painful, symmetric, red nodules |
| Anterior legs most common location |
| Involutes in weeks with bruise-like appearance |
| Does not ulcerate; tends to heal completely |

A prodrome commonly occurs as early as one to three weeks before the onset of erythema nodosum, regardless of the etiology. Specific symptoms may include weight loss, malaise, low-grade fever, cough, and arthralgia with or without arthritis.1–4 Arthralgias have been known to persist for up to two years after the resolution of erythema nodosum. They are seronegative for rheumatoid factor and cause nonspecific destructive joint changes. Abnormal laboratory findings may include leukocytosis in excess of 10,000 per mm3 and elevated erythrocyte sedimentation rate and C-reactive protein levels.4
Erythema nodosum migrans, subacute nodular migratory panniculitis, and chronic erythema nodosum, disorders classically considered distinct from erythema nodosum, now are considered to be variants in the same disease spectrum. Erythema nodosum migrans, although persistent, is minimally symptomatic and typically is first evident as unilateral nodules that tend to migrate centrifugally. Subacute nodular migratory panniculitis is characterized by nodules on the legs that may coalesce into plaques up to 8 inches (20 cm) in diameter. Chronic erythema nodosum can join to form larger plaques as well, although they are less inflamed compared with those of typical erythema nodosum. These variants constitute a small minority of erythema nodosum cases.
Pathophysiology and Histopathology
Erythema nodosum is a nonspecific cutaneous reaction pattern to a variety of antigens, with many immune-mediated mechanisms implicated. Most direct and indirect evidence supports the involvement of a type IV delayed hypersensitivity response to numerous antigens. Erythema nodosum often occurs in association with granulomatous disease, including sarcoidosis, tuberculosis, and granulomatous colitis.
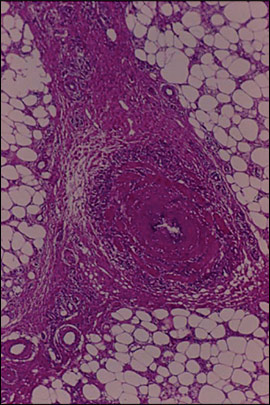
A deep incisional or excisional biopsy specimen should be obtained for best visualization because a punch biopsy is likely to produce an inadequate sample. Erythema nodosum represents an inflammation of the septa in the subcutaneous fat tissue: a septal panniculitis1–5 (Figure 2). A neutrophilic infiltrate around proliferating capillaries results in septal thickening in early lesions that may be associated with hemorrhage. Actinic (Miescher's) radial granulomas—small, well-defined nodular aggregates of tiny histiocytes around a central stellate cleft—are a characteristic finding.6 Erythema nodosum is not associated with vasculitis, although small vessel inflammation and hemorrhage can occur.
Causes of Erythema Nodosum
Erythema nodosum usually is idiopathic,2,4,7 but there are many possible causes (Table 2). Physicians should consider all possible etiologies of erythema nodosum and take a comprehensive history. A summary of the steps for diagnosing erythema nodosum is provided in Table 3,1–4,6,8 and a differential diagnosis is presented in Table 4.1,3,4,6
| Common | |
| Idiopathic (up to 55 percent) | |
| Infections: streptococcal pharyngitis (28 to 48 percent), Yersinia spp. (in Europe), mycoplasma, chlamydia, histoplasmosis, coccidioidomycosis, mycobacteria | |
| Sarcoidosis (11 to 25 percent) with bilateral hilar adenopathy | |
| Drugs (3 to 10 percent): antibiotics (e.g., sulfonamides, amoxicillin), oral contraceptives | |
| Pregnancy (2 to 5 percent) | |
| Enteropathies (1 to 4 percent): regional enteritis, ulcerative colitis | |
| Rare (less than 1 percent) | |
| Infections | |
| Viral: herpes simplex virus, Epstein-Barr virus, hepatitis B and C viruses, human immunodeficiency virus | |
| Bacterial: Campylobacter spp., rickettsiae, Salmonella spp., psittacosis, Bartonella spp., syphilis | |
| Parasitic: amoebiasis, giardiasis | |
| Miscellaneous: lymphoma, other malignancies | |
| Complete blood count with differential; erythrocyte sedimentation rate and C-reactive protein levels |
| Evaluation for streptoccocal infection (i.e., throat culture for group A streptococci, rapid antigen test, antistreptolysin-O titer, and polymerase chain reaction assay) |
| Excisional biopsy (when clinical diagnosis is in doubt); key histologic findings are septal panniculitis, lymphocytic infiltrate with neutrophils, actinic (Miescher's) radial granulomas, absence of vasculitis, and no organisms |
| Clinical suspicion of chronic disease (e.g., sarcoidosis, tuberculosis); purified protein derivative test, chest radiography |
| Stool culture and evaluation for ova and parasites in patients with diarrhea or gastrointestinal symptoms; consider evaluation for inflammatory bowel disease |
STREPTOCOCCAL PHARYNGITIS
Beta-hemolytic streptococcal infections are the most common identifiable cause of erythema nodosum. Streptococcal infections account for up to 44 percent of cases in adults and 48 percent of cases in children.2,4 Erythema nodosum eruptions may appear two to three weeks after an episode of streptococcal pharyngitis2; therefore, patients with erythema nodosum should have throat culture evaluation for group A streptococci, as well as streptococcal antistreptolysin-O (ASO) titers or polymerase chain reaction (PCR) assays, or both. ASO titers should be taken at the time of diagnosis and then again within four weeks to assess for streptococcal infection.
Real-time PCR assays have become an attractive option for the evaluation of group A streptococcal throat infections. One PCR assay is reported to have a sensitivity of 93 percent, a specificity of 98 percent, and positive and negative predictive values of 88 and 99 percent, respectively. This assay is advocated as an effective stand-alone alternative to rapid antigen immunoassays in the evaluation of streptococcal pharyngitis.8
| Most common |
| α1-antitrypsin deficiency |
| Cytophagic histiocytic panniculitis (a lymphoma) |
| Lupus erythematosus profundus (lupus panniculitis) |
| Nodular fat necrosis |
| Occasional |
| Necrobiosis lipoidica |
| Necrobiotic xanthogranuloma |
| Scleroderma |
| Subcutaneous granuloma |
| Rare |
| Cold panniculitis |
| Infectious panniculitis |
| Leukemic fat infiltrates |
| Lipodystrophies |
| Poststeroid panniculitis |
| Povidone panniculitis |
| Scleroderma neonatorum |
| Sclerosing panniculitis |
| Subcutaneous fat necrosis of the newborn |
TUBERCULOSIS AND ATYPICAL MYCOBACTERIAL INFECTIONS
Tuberculosis has long been linked with erythema nodosum.1,3,9,10 Erythema nodosum may occur with primary tuberculosis and may even manifest before the development of a skin-test reaction to tuberculin. The bacille Calmette-Guérin vaccination and the tuberculin skin test have been associated with the development of erythema nodosum. Furthermore, erythema nodosum may be found in patients with highly positive reactions to the Mantoux skin test but no detectable focus of tubercular infection.
All patients with erythema nodosum should be stratified by risk for tuberculosis exposure. Appropriate measures include tuberculin skin test, chest radiography, and acid-fast bacilli sputum analysis. Antitubercular therapy should be initiated for erythema nodosum in patients with positive Mantoux skin test reactions with or without a positively identified focus of infection.11,12
Culture identification from primary sites of infection also may be valuable in identifying an atypical nontuberculous mycobacterium as a cause of erythema nodosum. Several atypical mycobacteria have been associated with erythema nodosum, including Mycobacterium marinum, which may be found in swimming pools.1,12 Identification of the species is important because treatment should be tailored to the specific organism.
SYSTEMIC MYCOSES
The patient's geographic location and travel history should be considered. Histoplasma capsulatum, Blastomyces dermatitidis, Paracoccidioides brasiliensis, and Coccidioides immitis have been implicated in the development of erythema nodosum.13 In western and southwestern areas of the United States, erythema nodosum commonly is caused by coccidioidomycosis, also known as San Joaquin Valley fever. The incidence of erythema nodosum in patients with symptomatic coccidioidomycosis is approximately 5 percent. In these instances, erythema nodosum is preceded by upper respiratory symptoms, and its onset tends to occur before immunoglobulin M antibody serology for Coccidioides becomes positive.13,14 Patients who develop coccidioidomycosis while pregnant experience dissemination and life-threatening disease more often than others. However, erythema nodosum in pregnant women with coccidioidomycosis can be considered a favorable prognostic sign because dissemination of the organism beyond the lungs is less likely in these patients than in other patients with coccidioidomycosis.14
OTHER INFECTIONS
Other infectious etiologies of erythema nodosum are summarized in Table 2. Infectious causes of erythema nodosum occasionally involve the gastrointestinal tract,1,7,15–17 and reports indicate that the incidence of gastrointestinal infections may be increasing.17 Therefore, a thorough patient evaluation, including stool cultures, should be considered in patients with erythema nodosum and diarrhea.
MEDICATIONS
Hypersensitivity reactions to medications have been recognized as a cause of 3 to 10 percent of erythema nodosum cases.1,2,4 Oral contraceptives and numerous antibiotics, including amoxicillin and especially sulfonamides, have been associated with erythema nodosum.1–4,18 Proton-pump inhibitors and leukotriene modifiers also have been implicated, although evidence is limited to case reports.19,20 If possible, all causative medications should be discontinued once erythema nodosum is diagnosed.
SARCOIDOSIS
Sarcoidosis causes up to one fourth of erythema nodosum cases.2,4,7 Radiographic imaging often reveals bilateral hilar adenopathy, with one study reporting chest radiography or computed tomography findings of bilateral hilar adenopathy or mediastinal lymphadenopathy in all patients with erythema nodosum caused by sarcoidosis.21 Traditionally, erythema nodosum has been regarded as a good prognostic indicator in patients with sarcoidosis, although this may be true only for patients of northern European descent.3
Sarcoidosis with hilar adenopathy, polyarthritis, and erythema nodosum is called Löfgren's syndrome and has a good prognosis. Löfgren's syndrome tends to be acute and self-limited, resolving in six to eight weeks, whereas sarcoidosis can be chronic and progressive.7
ENDOCRINE-HORMONAL
Erythema nodosum occurs in up to 4.6 percent of women who are pregnant, possibly as a result of estrogen production or relative levels of estrogen and progesterone.1,7,18 Estrogen also has been proposed as the implicating factor behind the adult male-to-female incidence ratio of 1:6.4 Combination estrogen and progesterone oral contraceptive medications have been associated with erythema nodosum for decades. Hormone therapy also has been implicated.18 Since the introduction of low-dose oral contraceptives in the 1980s, the number of oral contraceptive–related cases of erythema nodosum has decreased. This decline may be a result of current at-or-below physiologic levels of 20 to 50 mcg ethinyl estradiol in oral contraceptives, although a well-defined association between estrogen and erythema nodosum has not been established. Furthermore, there have been no reported cases of estrogen-secreting obstetric malignancies causing erythema nodosum. The relative concentration of estrogen and progesterone in oral contraceptives and hormone therapy as well as during pregnancy may be more directly associated with erythema nodosum than estrogen levels alone.18
CHRONIC INFLAMMATORY AND AUTOIMMUNE DISORDERS
In addition to infectious colitis, other gastrointestinal diseases, such as ulcerative colitis and Crohn's disease, are associated with erythema nodosum. Erythema nodosum with abdominal pain and diarrhea may reflect acute flare-ups. Firm control of colitis may prevent further erythema nodosum; suppression of erythema nodosum in the patient may be considered an indicator for disease management.22 As many as 50 percent of patients with Behçet's syndrome have associated erythema nodosum.4 The biopsy-proven coexistence of Sweet's syndrome and erythema nodosum has been documented.23
MALIGNANCY
Erythema nodosum may be a cutaneous marker of malignancy, most often lymphoma or leukemia.24–27 Rarely, other malignancies may be associated with erythema nodosum, including carcinoid and colorectal and pancreatic cancers.25,26 Erythema nodosum also can indicate disease progression. For example, in a patient with a history of Hodgkin's disease, the development of erythema nodosum may reflect recurrence.3,27 A work-up should be considered, especially when erythema nodosum is accompanied by clinical suspicion for malignancy.
Treatment
Although erythema nodosum can be exquisitely tender, it tends to be self-limited. The most common approach is treatment of any underlying disorders and supportive therapy, including bed rest and avoidance of contact irritation of affected areas. Pain can be managed conservatively with nonsteroidal anti-inflammatory drugs (NSAIDs). More aggressive pain management is reserved for clinical situations that become recurrent or unusually prolonged.
Oral potassium iodide prepared as a supersaturated solution in a dosage of 400 to 900 mg per day for one month is a therapeutic option. Potassium iodide therapy is more likely to be effective in providing symptomatic relief if begun at the onset of the erythema nodosum.28 Caution must be taken to avoid hyperthyroidism, a risk with prolonged use.
Systemic steroids have been advocated as a relatively safe therapeutic option if underlying infection, risk of bacterial dissemination or sepsis, and malignancy have been excluded by a thorough evaluation. Oral prednisone at a dosage of 60 mg every morning is typical. A general rule is 1 mg per kg body weight per day.1,3
Treatment also may be tailored to disease-specific regimens: steroids used in combination with hydroxychloroquine (Plaquenil), cyclosporin A (Sandimmune), or thalidomide (Thalomid) have been used to treat inflammatory bowel disease–associated erythema nodosum. NSAIDs should be avoided in treating erythema nodosum secondary to Crohn's disease because they may trigger a flare-up or worsen an ongoing acute bout.29 Colchicine has been used in patients with erythema nodosum and coexisting Behçet's syndrome, with varying results.30