
Am Fam Physician. 2007;75(6):869-873
Author disclosure: Financial support for Dr. Diaz was provided by the State of Louisiana Board of Regents Health Education Fund.
There are more than 30,000 species of spiders, most of which cannot inflict serious bites to humans because of their delicate mouthparts and impotent or prey-specific venoms. However, some spiders produce toxic venoms that can cause skin lesions, systemic illnesses, and neurotoxicity. One of the more common bites is inflicted by the widow spiders (Latrodectus species). A bite from a widow spider results in muscle spasms and rigidity starting at the bite site within 30 minutes to two hours. Another common bite is inflicted by the recluse spider (Loxosceles species). Most bites from these spiders occur early in the morning and are initially painless. These bites usually progress to ulcerating dermonecrosis at the bite site. Spider bites can be prevented by simple measures. Early species identification and specific management can prevent most serious sequelae of spider bites.
Arthropod bites and stings are common in the United States, where more than 50,000 exposures occur each year.1 Less than one half of these exposures are spider bites.1 An arthropod bite is defined as a skin lesion produced by the oral elements used for catching and consuming prey or for blood feeding.1 Although spiders cannot transmit communicable diseases, some spiders produce toxic venom that can cause skin lesions, systemic illnesses, and neurotoxicity. The epidemiologic analysis of spider bites is confounded by several factors, including recall bias, the extensive differential diagnosis of dermonecrotic bite-like lesions, suspected versus confirmed bites and stings, and lack of entomologic identification of biting arthropods2–7 (Table 1).
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Antivenin is recommended for all patients with significant latrodectism following widow spider bites. | B | 10–12 |
| Appropriate and timely tetanus prophylaxis is recommended following all envenoming spider bites. | C | 10,13,14 |
| Wound cleansing and conservative debridement are recommended in managing necrotic arachnidism followingLoxosceles bites. | C | 13–16 |
| Referral to an ophthalmologist is recommended for patients with ophthalmia nodosa caused by ocular-embedded tarantula hairs. | C | 20–26 |
| Arthropod bites and stings | Infectious diseases | Other conditions |
| Bee | Chagas' disease | Allergic contact dermatitis |
| Beetle | Dermatomycosis | Angioneurotic edema |
| Centipede | Erysipelas | Autoimmune vasculitides |
| Flies | Furuncles or boils | Chemical burns |
| Hornet | Herpes simplex | Chemical contact dermatitis |
| Mosquito | Herpes zoster | Diabetic ulcers |
| Reduviid bug (triatomid) | Impetigo | Erythema multiforme |
| Scorpion | Lyme disease | Lymphomatoid papulosis |
| Tick | Pyoderma gangrenosum | Poison ivy, oak, or sumac |
| Wasp | Sporotrichosis | Venous stasis ulcers |
| Yellow jacket | Syphilis |
Online Table A details the diagnosis and management of caterpillar stings.
Diagnostic findings
|
Widow Spiders
The five species of widow spiders in the United States include Latrodectus bishopi, Latrodectus geometricus, Latrodectus hesperus, Latrodectus variolus, and Latrodectus mactans (Figure 1). Females are darker, more venomous, and significantly larger than males (leg spans of 30 to 40 mm compared with 16 to 20 mm). Males also are capable of biting but rarely inflict severely envenoming bites.7,8 Most females are dark gray or black with red or orange hourglass or geometric patterns, spots, or stripes on their ventral abdomens. Latrodectus spiders are most abundant and active during the warmer months.

Systemic toxicity from widow spider bites (i.e., latrodectism) is caused by α-latrotoxin, a neurotoxic component of Latrodectus venom that causes massive presynaptic release of most neurotransmitters, including acetylcholine, norepinephrine, dopamine, and glutamate. The signs and symptoms of Latrodectus and Loxosceles (i.e., recluse spiders) bites are compared in Table 2.8–18
| Bite characteristics | Widow spider (Latrodectus)bites | Recluse spider (Loxosceles)bites |
|---|---|---|
| Initial bite symptoms | Moderately to severely painful; little or no surrounding inflammation | Painless or minimally painful; localized inflammation that subsequently spreads |
| Presumed mechanism of envenomation | Massive presynaptic discharge of all autonomic neurotransmitters | Local cytotoxicity with subsequent ulcerating dermonecrosis |
| Predominant toxin | α-Latrotoxin | Sphingomyelinase D |
| Potential for systemic toxicity | Present; usually atypical and rarely full-blown (latrodectism) | Present but rare (loxoscelism) |
| Incubation period from bite to systemic toxicity | Rapid (i.e., 30 minutes to two hours) | Delayed (i.e., three to seven days) |
| Most common signs of systemic toxicity | Muscular spasm and rigidity beginning at bite site and spreading proximally to abdomen and face; rebound tenderness mimicking acute appendicitis is possible. | Arthralgias, fever, chills, maculopapular rash, nausea, vomiting |
| Potential associated signs of systemic toxicity | Arthralgias, bronchorrhea, regional or generalized diaphoresis, fever, hypertension, hyperreflexia, regional lymphadenopathy, nausea, vomiting, paresthesias, priapism, ptosis, restlessness, salivation | Febrile seizures, hemoglobinuria, myoglobinuria, acute renal failure |
| Outcomes of most bites | Resolution of all manifestations over two or three days; death rarely occurs | Most necrotizing ulcers will heal over one to eight weeks with a 10 to 15 percent incidence of major scarring. One study found no deaths in 111 patients with entomologist-confirmedLoxosceles reclusa bites.15 |
Local wound care of Latrodectus bites should include thorough wound cleansing and ice pack application. Other treatments include oral or parenteral analgesics, benzodiazepines for muscular spasm and rigidity, and tetanus prophylaxis. Latrodectus antivenin is indicated for patients manifesting severe regional or systemic toxicity, and for patients with uncontrolled hypertension, seizures, or respiratory arrest.10,11 One vial of antivenin diluted in 100 to 250 mL of saline should be infused intravenously over two hours; this process should be repeated for patients with persistent muscular spasms.10,11 In severe envenomations, especially in children, antivenin may be effective in reversing latrodectism up to 90 hours after the bite occurs.12
Symptomatic children, pregnant women, and elderly patients with hypertension or coronary artery disease should be hospitalized and observed for seizure activity, threatened abortion, and myocardial ischemia, respectively.10 In severe cases, the initial laboratory evaluation should include complete blood count and urinalysis to rule out peritonitis and urinary tract infections, and measurement of serum creatine phosphokinase and lactic dehydrogenase to detect rhabdomyolysis from muscular spasm and rigidity.
Recluse Spiders
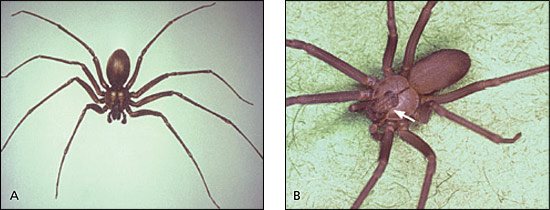
The six species of recluse spiders in the United States include Loxosceles arizonica, Loxosceles deserta, Loxosceles devia, Loxosceles laeta, Loxosceles rufescens, and Loxosceles reclusa (Figure 2). Loxosceles spiders are most abundant and active at night during the warmer months.7 All Loxosceles spiders in the United States may cause bites characterized by necrotic arachnidism with dermonecrotic ulceration at bite sites, presumably because of autoimmune responses from cytokines and lymphocytes and cytotoxicity from venom components (mainly sphingomyelinase D). All Loxosceles spiders are brown, often have no unique identifying markings (except for female brown recluse spiders [L. reclusa]), and often are simply described as brown spiders.13,14 Female recluses are more venomous and generally larger than males (leg spans of 20 to 30 mm compared with 10 to 35 mm), and they have distinctive, darker brown patterns on the dorsal cephalothorax.13,14 These patterns resemble a violin, fiddle, or cello (with the base at the head end), bordered by three pairs of eyes13–15 (Figure 2B).
Most Loxosceles bites in humans occur in the early morning; bites cluster wherever bed linens, bedclothes, or other garments squeeze the female spider between fabric and the victim's skin, particularly under the arms, at the waist, or on the lower extremities under socks, stockings, or pants. Immediate wound care should include thorough cleansing, cold compresses, elevation of the bitten extremity, immobilization, oral or parenteral analgesics and antihistamines, and tetanus prophylaxis.13–15 Early excision of bite lesions and intralesional injection of corticosteroids could extend the dermonecrosis and are contraindicated.13–15
Wound care also should include debridement of necrotic tissues, culture-directed antibiotic therapy for secondary infections, and delayed excision of eschars, with split-thickness skin grafting as indicated.13–15 With proper wound management, necrotic wounds will heal over one to eight weeks with a 10 to 15 percent incidence of major scarring.13–16
Hyperbaric oxygenation has been recommended to reverse the expanding dermonecrosis of loxoscelism, but it has shown mixed treatment outcomes and is not supported by controlled trials.17 In the past, oral leukocyte microtubular inhibitors such as dapsone or colchicine were recommended to halt expanding dermonecrosis, presumably from leukocyte migration, degranulation, and cytokine release.13–18 However, the effectiveness of leukocyte inhibitor therapy was not supported by controlled trials and posed a substantial risk of toxicity.
Tarantulas
Most tarantulas in the United States live in the Desert Southwest but commonly are found as far east as the Mississippi River and as far north as Arkansas. Tarantula envenomation in humans usually causes mild stinging with minimal surrounding inflammatory reaction, no dermonecrosis, and no serious systemic sequelae.19 Although tarantula bites usually are innocuous in humans, they often are lethal in domestic animals and pets, particularly dogs.19 The management of tarantula bites should be conservative and symptomatic, with thorough wound cleansing, tetanus prophylaxis, elevation of the bitten extremity, immobilization, and oral analgesics as needed.
Four genera of New World tarantulas (i.e.,Acanthoscurria, Brachypelma, Grammostola, and Lasiodora) and many tarantula species have urticating hairs on their dorsal abdomens, which can be flicked off by the thousands to irritate and incapacitate pursuing aggressors. In humans, these hairs can penetrate the skin and cause severe pruritic reactions; they also can lodge in the cornea, causing foreign body keratoconjunctivitis or ophthalmia nodosa, which appears as a nodular, granulomatous inflammatory lesion in the ocular area.20–26 Any patient with a history of tarantula exposure and suspected ophthalmia nodosa should be referred immediately to an ophthalmologist for corneal slit-lamp examination, immediate conservative treatment, and follow-up care.20–26 If left untreated, ophthalmia nodosa can lead to keratitis, anterior or posterior uveitis, chorioretinitis, and orbital cellulitis.
Prevention and Control
Most spider bites are inflicted by spiders of minor medical importance (Table 3); these bites generally occur outdoors or indoors during daytime activities in the spring and summer, when the potential for human-spider encounters is greatest. Spider bites may be prevented by wearing gloves, long-sleeved shirts, and long pants tucked into socks when outdoors, especially when gathering firewood and clearing brush. Spraying clothing with synthetic pyrethroids and applying insect repellant containing N, N-diethyl-m-toluamide (DEET) to nonmucosal exposed areas may offer additional protection. Indoor spider bites may be prevented by properly insulating homes, especially windows and exterior doors, attics, and basement crawl spaces; by removing spiderwebs with brooms or vacuum cleaners; and by applying safe indoor insecticides, such as synthetic pyrethroids or natural pyrethrins.
| Genus | Common name |
|---|---|
| Araneus | Orb weaver |
| Argiope | Argiopes, garden spider |
| Bothriocyrtum | Trap door spider |
| Drassodes | Gnaphosid spider, mouse spider |
| Herpyllus | Parson spider |
| Heteropoda | Huntsman spider |
| Liocranoides | Running spider |
| Lycosa | Wolf spider |
| Misumenoides | Crab spider |
| Neoscona | Orb weaver, barn spider |
| Peucetia | Green lynx spider |
| Phiddipus | Jumping spider |
| Steatoda | False black widow spider |
| Ummidia | Trap door spider |
Tarantulas should not be handled near the face, and gloves and eye protection should be worn. Tarantula owners and zookeepers also should wear gloves, surgical masks, and eye protection when cleaning tarantula terrariums. If necessary, nuisance or threatening spiders of any species should be killed or sprayed from a distance and away from face level to avoid contact with skin, eyes, and the upper respiratory tract. Patients should be counseled that the safest way to prevent a spider bite is to gently flick the spider with a finger, rather than crushing the spider against the skin, which serves only to open the chelicerae by reflex, causing the fangs to spring into biting position.