
Am Fam Physician. 2007;76(4):565-566
Author disclosure: Nothing to disclose.
A 48-year-old woman presented with a two-week history of progressively decreasing vision in her right eye. Her medical history included systemic lupus erythematosus, severe arthritis, hypertension, and diabetes mellitus. She had been taking oral prednisone, azathioprine (Imuran), amlodipine (Norvasc), and insulin. Her most recent A1C level was 10 percent.
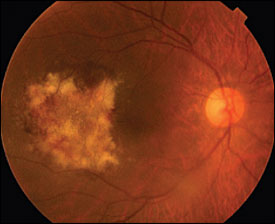
The patient's blood pressure was 145/90 mm Hg. On visual examination, the best corrected acuity was 20/30 in her right eye and 20/20 in her left eye. No afferent pupillary defect (i.e., Marcus Gunn pupil) was noted. Confrontation visual field testing showed a paracentral scotoma in her right eye. Dilated fundus examination revealed a yellow-white retinal lesion in the temporal macula of the right eye. Scattered intraretinal hemorrhages also were noted within the lesion (see accompanying figure). Examination showed that the left eye was normal. Mild anemia and leukopenia were detected on laboratory testing.
Question
Discussion
The answer is B: Cytomegalovirus (CMV) retinitis. CMV retinitis typically occurs in immunocompromised patients and is the most common opportunistic eye infection in those with acquired immunodeficiency syndrome (AIDS).1 CMV likely spreads hematogenously to the retina.
CMV retinitis may affect the central retina (macula) or the peripheral retina.2 In the former, the retinitis is characterized by well-demarcated white areas of retinal necrosis, usually occurring along the retinal vascular arcades. Hemorrhage may develop within or along the leading edge of the retinitis, giving a “pizza pie” appearance. In the peripheral form, the retinitis has a less well-demarcated, more granular appearance. Retinal detachment may develop in both forms as the retinitis worsens and results in a thin, atrophic retina.
Treatment involves induction and maintenance phases. Intravenous ganciclovir (Cytovene), foscarnet (Foscavir), or cidofovir (Vistide) is used in the induction phase.3 Oral formulations of ganciclovir and valganciclovir (Valcyte) are available, allowing for maintenance treatment without the need for intravenous access.4 Furthermore, valganciclovir is effective as an induction and maintenance agent for patients with AIDS-related CMV retinitis.5
Intravitreal injection of ganciclovir, foscarnet, or fomivirsen (Vitravene; brand not available in the United States) allows for direct delivery of the drug to the affected site and is often used, with oral valganciclovir, in the acute phase of CMV retinitis. An intravitreal ganciclovir implant is also available; the device is placed surgically in the vitreous cavity to allow sustained release of the medication over seven to eight months.5 In patients who develop retinal detachment from CMV retinitis, pars plana vitrectomy using silicone oil tamponade with or without the placement of the ganciclovir implant is the treatment of choice.
Branch retinal vein occlusion is characterized by dilated and tortuous veins, flame-shaped and dot and blot hemorrhages, and retinal edema. Cotton-wool spots (i.e., fluffy white areas of microinfarcts) may be observed.
In diabetic and hypertensive retinopathies, the findings usually are bilateral. In patients with diabetic retinopathy, hard yellow exudates result when lipoproteins leak from incompetent retinal vessels. In hypertensive retinopathy, retinal arteriolar constriction occurs in response to increased blood pressure. Over time, arteriosclerosis with vessel wall thickening may occur. These changes tend to occur at the arteriovenous crossings. Hard exudates and fluffy white cotton-wool spots may develop in patients with severe, accelerated hypertension.
Toxoplasmic retinochoroiditis usually causes moderate to severe vitreous inflammation, which may obscure the view of the retina.
| Condition | Characteristics |
|---|---|
| Branch retinal vein occlusion | Cotton-wool spots may be observed; the predominant features are dilated, tortuous retinal veins and intraretinal hemorrhages |
| Cytomegalovirus retinitis | Yellow-white, well-demarcated or granular lesions representing retinal necrosis, often along retinal vessels; retinal hemorrhages may be found within the retinitis or along itsleading edge |
| Diabetic retinopathy | Hard exudates with a yellow, waxy appearance |
| Hypertensive retinopathy | Retinal arteriolar constriction and arteriosclerosis causing vessel wall thickening, especially at arteriovenous junctions; cotton-wool spots may develop |
| Toxoplasmic retinochoroiditis | Yellow retinal lesions with indistinct borders, often adjacent to a retinal scar; moderate to severe vitreous inflammation may be present, possibly obscuring the view of theretina |