
Am Fam Physician. 2007;76(7):975-983
Author disclosure: Nothing to disclose.
Chronic foot pain is a common and often disabling clinical complaint that can interfere with a patient's routine activities. Despite careful and detailed clinical history and physical examination, providing an accurate diagnosis is often difficult because chronic foot pain has a broad spectrum of potential causes. Therefore, imaging studies play a key role in diagnosis and management. Initial assessment is typically done by plain radiography; however, magnetic resonance imaging has superior soft-tissue contrast resolution and multiplanar capability, which makes it important in the early diagnosis of ambiguous or clinically equivocal cases when initial radiographic findings are inconclusive. Computed tomography displays bony detail in stress fractures, as well as in arthritides and tarsal coalition. Bone scanning and ultra-sonography also are useful tools for diagnosing specific conditions that produce chronic foot pain.
Approximately 40 percent of adults in the United States experience foot problems.1 Plain radiography is an important diagnostic tool in the initial evaluation of patients with chronic foot pain. It is the most commonly used modality because of its wide availability and low cost. Radiography using the oblique view shows articulation of the calcaneus, talus, navicular, and cuboid bones, and it can be helpful in patients with foot pain who have no obvious diagnosis.
Although not routinely indicated, magnetic resonance imaging (MRI) can play a significant role in making a precise diagnosis, guiding treatment decisions, and determining response to therapy. Bone scanning, ultrasonography, and computed tomography (CT) also are useful tools in the diagnosis of specific conditions. The multidetector row CT, one of the newest modalities, significantly improves scan speed and utilization of the available radiographic power. This advanced CT is indicated for the evaluation of cortex and trabecular bone detail.
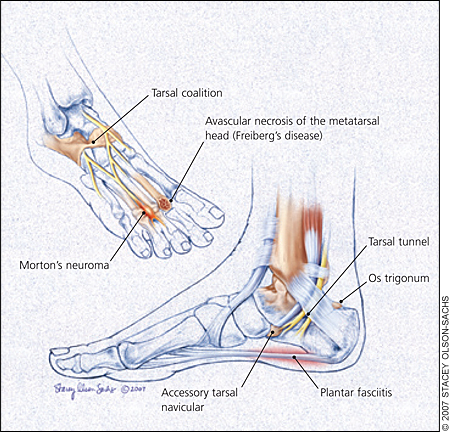
This review discusses causes of chronic foot pain (Table 12,3; Figure 1), their clinical presentations, and their radiologic findings (Table 24), and explains the American College of Radiology (ACR) Appropriateness Criteria Scale for chronic foot pain imaging (Table 35). The scale ranges from 1 to 9, with 1 meaning it is the least appropriate test and 9 meaning it is the most appropriate test.
| Common |
| Arthritis |
| Morton's neuroma |
| Plantar fasciitis |
| Stress fracture |
| Less common |
| Painful accessory bones |
| Reflex sympathetic dystrophy |
| Tarsal tunnel syndrome |
| Rare |
| Avascular necrosis of the metatarsal head (Freiberg's disease) |
| Tarsal coalition |
| Condition | Clinical presentation | Radiologic findings |
|---|---|---|
| Arthritis | Fatigue; joint deformity; joint pain that is often symmetrical; swelling | Erosion; fragmentation; joint space narrowing; soft-tissue swelling |
| Avascular necrosis of the metatarsal head (Freiberg's disease) | Pain, tenderness, swelling, and limitation of motion in the affected metatarsophalangeal joint | Collapse, cystic changes, and flattening of the metatarsophalangeal joint; sclerosis |
| Morton's neuroma | Often asymptomatic; pain in the involved web space that often radiates to the toes | Mass in intermetatarsal space |
| Painful accessory bones | Accessory tarsal navicular bones occur at the medial and posterior margins of the tarsal navicular, and os trigonum occurs adjacent to the posterior margin of the talus; pain and tenderness in the affected area | Marrow edema; presence of ossicle |
| Plantar fasciitis | Plantar heel pain | Fascial tear; marrow edema; plantar calcaneal spur |
| Reflex sympathetic dystrophy | Diminished motor function; pain and tenderness; swelling; vasomotor instability | Diffuse osteopenia; increased tracer uptake |
| Stress fracture | Limitation of motion; pain and tenderness in affected area | Callus formation; fracture line; periosteal reaction |
| Tarsal coalition | Bilateral in 50 percent of patients; restricted subtalar motion; rigid, painful flatfoot; valgus deformity of the hindfoot | C sign; flattening and broadening of the lateral talar process; narrowing of the talocalcaneal joint; talar breaking |
| Tarsal tunnel syndrome | Diffuse burning pain and paresthesias along the plantar surface of the foot and toes | Mass in the tarsal tunnel; synovial hypertrophy in tarsal tunnel |
| Variant | Radiologic examination | Appropriateness rating |
|---|---|---|
| Arthritis | Plain radiography; AP, lateral, and oblique | 9 |
| Plain radiography; AP and lateral | 2 | |
| CT | 2 | |
| MRI | 2 | |
| Nuclear medicine imaging; bone scan | 2 | |
| Ultrasonography | 2 | |
| Avascular necrosis of the metatarsal head (Freiberg's disease) | Plain radiography; AP and lateral with or without oblique | 9 |
| CT | 2 | |
| MRI | 2 | |
| Nuclear medicine imaging; bone scan | 2 | |
| Ultrasonography | 2 | |
| Morton's neuroma | Plain radiography; AP and lateral | 9 |
| MRI | 9 | |
| Ultrasonography (can be used in place of MRI, with proper expertise) | 9 | |
| CT | 2 | |
| Nuclear medicine imaging; bone scan | 2 | |
| Painful accessory bones | MRI | 9 |
| Nuclear medicine imaging; bone scan | 3 | |
| CT | 2 | |
| Ultrasonography | 2 | |
| Plantar fasciitis | Plain radiography; AP and lateral | 9 |
| MRI | 9 | |
| Ultrasonography (can be used in place of MRI, with proper expertise) | 8 | |
| Nuclear medicine imaging; bone scan | 2 | |
| CT | 2 | |
| Reflex sympathetic dystrophy | Plain radiography; AP, lateral, and oblique | 9 |
| Nuclear medicine imaging; bone scan (if plain films are not diagnostic) | 8 | |
| Plain radiography; AP and lateral | 2 | |
| CT | 2 | |
| MRI | 2 | |
| Ultrasonography | 2 | |
| Stress fracture | MRI | 9 |
| CT (especially for follow-up of healing fractures) | 6 | |
| Nuclear medicine imaging; bone scan (if MRI cannot be performed) | 2 | |
| Ultrasonography | 2 | |
| Tarsal coalition | Plain radiography; AP, lateral, oblique, and Harris-Beath view | 9 |
| CT | 9 | |
| Plain radiography; AP and lateral | 2 | |
| MRI | 2 | |
| Nuclear medicine imaging; bone scan | 2 | |
| Ultrasonography | 2 | |
| Tarsal tunnel syndrome | Plain radiography; AP, lateral, and oblique | 9 |
| MRI | 9 | |
| Ultrasonography (can be used in place of MRI, with proper expertise) | 8 | |
| Nuclear medicine imaging; bone scan | 2 | |
| CT | 2 |
Illustrative Cases
CASE 1
A 60-year-old woman presented with pain in the second toe of her right foot. The pain has progressed with weight bearing or flexion at the metatarsophalangeal joint. The initial plain radiographs showed subtle lucency with cortical interruption over the distal shaft of the second metatarsal, which was initially interpreted as a stress fracture (Figure 2A). The patient has had limited weight bearing. A follow-up plain radiograph taken four months later reveals a fusiform expansion of the cortex with callus formation (Figure 2B).

CASE 2
A 15-year-old female cross-country runner presented with right foot and ankle pain most prominent over the anterior side of the ankle and plantar arch. The clinical impression at that time was a stress fracture. The initial plain radiograph was not helpful and was interpreted as negative (Figure 3A). T2-weighted MRI taken two days later clearly demonstrates bone marrow edema of increased signal intensity in the tarsal navicular, which is associated with osseous stress reaction (Figure 3B).

Arthritis and Tendinopathy
All common forms of arthritides affect the feet and can cause chronic foot pain. Most arthritides are best evaluated with plain radiography. Radiographic findings include joint space narrowing, osteophyte formation, subchondral sclerosis, and cyst formation. The most common site for gout is the foot, especially the first metatarsophalangeal joint. As the tophi enlarge, they erode the para-articular bone, producing sharp, punched-out erosions with well-defined cortical margins. Calcium pyrophosphate deposition disease is the most common form of crystal-induced arthropathy. With this disease, the talonavicular joint can sometimes be involved.
Rheumatoid arthritis also typically involves the foot. Radiographic findings include periarticular soft-tissue swelling, marginal erosion (where the bone is not protected by overlying cartilage), periarticular osteopenia, and uniform joint space narrowing. There is evidence that gadolinium-enhanced MRI can be helpful in detecting early rheumatoid arthritis.6 Radiography in seronegative arthritis is more likely to show new bone formation and fusion. Bilateral heel pain is suggestive of seronegative arthritides.
Neuropathic arthropathy is destructive joint changes caused by diminished pain sensation and proprioception that leaves the joint without protection from repeated microtrauma during continued activity.7 Neuropathic changes are still best detected by plain radiography, although early changes may be more easily diagnosed with MRI or suggested with bone scanning. Neuropathic arthropathy in patients with diabetes involves the forefoot (metatarsophalangeal and interphalangeal joints), tarsometatarsal joint (Lisfranc's joint), and hindfoot (subtalar and ankle joints).7,8 Fracture-dislocation of Lisfranc's joint is one of the most common features of neuropathic arthropathy in patients with diabetes. MRI reveals myositis, bone edema, and foot ulcers associated with diabetes before revealing other features of neuropathic osteoarthropathy. Most importantly, MRI can diagnose superimposed infection by identifying ulcers, cellulitis, sinus tracts, and soft-tissue abscesses. Abnormal marrow in osteomyelitis and neuropathic reactive bone edema also can be assessed on MRI.
Tendinopathy of the foot, ranging from tendinosis or tendon degeneration to a complete tear, can result in significant pain and disability. The most commonly affected tendons are the Achilles, posterior tibial, and peroneal. All MRI sequences visualize ankle tendons as low-signal–intensity structures. T1-weighted images provide good anatomic detail, whereas T2-weighted images are useful for evaluating the abnormal increased signal intensity that occurs in most pathologic conditions. MRI can also depict and characterize the morphologic features of the tendon pathology (e.g., tear, split, retraction), as well as the adjacent soft tissue abnormalities.
MRI findings for tendinosis include a fusiform shape and areas of increased signal intensity on T1-weighted images and variable-signal–intensity alteration on T2-weighted images. In persons with tenosynovitis, MRI will reveal fluid accumulation within the tendon sheath. Tendon rupture is depicted as disruption of the tendon fibers. Avulsion of the posterior calcaneal tuberosity at the insertion of the Achilles tendon is fairly common and is sometimes pathognomonic of diabetes mellitus.9 Achilles tendon avulsion of the calcaneal tuberosity can also occur in trauma and renal osteodystrophy.
Morton's Neuroma
Morton's neuroma is a non-neoplastic, perineural, fibrous proliferation involving a plantar digital nerve. Clinical symptoms include pain in the involved web space that often radiates to the toes. These neuromas occur more often in women and typically involve the three-four (or less commonly, the two-three) inter-metatarsal space.10 They are best detected on MRI using T1-weighted inversion recovery or T1-weighted, fatsuppressed images with gadolinium enhancement and T2-weighted images in the coronal plane. The diagnosis of Morton's neuroma with MRI becomes relevant only when transverse diameter of the lesion is at least 5 mm and can be correlated with the clinical findings.10 High-resolution ultrasonography also has been used to successfully diagnose Morton's neuroma.
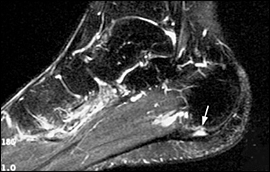
Plantar Fasciitis
Plantar fasciitis is the most common cause of plantar heel pain. It is thought to be a chronic traction type injury, and it may occur in isolation or as a manifestation of a systemic disease such as seronegative spondyloarthropathies, rheumatoid arthritis, gout, or systemic lupus erythematosus. In athletes, plantar fasciitis typically produces foot pain and is attributed to mechanical stresses, presumably caused by repetitive trauma that creates microtearing of the plantar fascia at its origin, as well as fascial and perifascial inflammation. Plantar fasciitis is common in patients who are obese and in those who have flatfoot. The diagnosis is usually made on clinical grounds.
Typically, plain radiography is not helpful, but it is always done to rule out other conditions. Radiography may reveal a plantar calcaneal spur, but because this type of spur is commonly observed in asymptomatic adults, it is not a sign of any one specific condition. Bone scanning and MRI have been shown to be helpful in determining a diagnosis11; however, MRI is rated 9 on the ACR Appropriateness Criteria Scale, whereas bone scanning is rated 2 because MRI could show more detailed findings. MRI findings include thickening of the proximal plantar fascia (7 to 8 mm; normal is 3 to 4 mm), inflammation in the plantar aponeurosis, adjacent soft-tissue edema, reactive calcaneal marrow edema and fluid-filled fascia, and rupture at mid or proximal segments (Figure 4). One study showed that ultrasonography is effective in differentiating normal plantar fascia from those involved in plantar fasciitis.12
Stress Fractures
Stress fractures can be categorized into three types: stress reactions, fatigue fractures, and insufficiency fractures.9,13 A stress reaction occurs when microfractures are healing and a complete fracture has not yet developed. A fatigue fracture is caused by the prolonged cyclical application of abnormal mechanical stresses to a bone that has normal elastic resistance. Activities that produce fatigue fractures include running, marching, and dancing. Insufficiency fractures occur with normal or physiologic stresses on a weakened skeleton that is deficient in mineral or elastic resistance. The second and third metatarsals (Figure 2), the tarsal navicular, and the calcaneus are the most common sites for stress fractures.9,13 Although rare, stress fractures also have been described in the fifth metatarsal,14 the first metatarsal, and medial sesamoid bones of the great toe.
Plain radiography may be entirely normal early on, but with time, a fracture line can be identified. Only one cortex may be involved; a hint of periosteal reaction with some endosteal new bone may develop. It can take three to four weeks for changes to occur in the metaphyseal area of bone, and four to six weeks for them to occur in the diaphysis. During the healing phase, new periosteal and endosteal bone are incorporated in the cortex, resulting in a fusiform expansion of the cortex (Figure 2B). Occasionally more than one stress fracture is present in the same foot. In the tarsal navicular, stress fractures are oriented in the sagittal plane and occur in the central third of the bone. They start as partial fractures involving only the dorsal portion of the tarsal navicular.
Although plain radiography is not listed in the original ACR Appropriateness Criteria Scale for stress fracture, it is typically ordered first. Initially, plain radiography (Figure 3A) and CT can be negative. In this case, the next best test could be MRI. MRI is a good imaging choice if radiography is negative and if there is suspicion of early injury.15 It detects the bone marrow edema associated with osseous stress reactions that may be present before a fracture line is visualized (Figure 3B).
Before the advent of MRI, bone scanning was the first-line option for evaluating stress fractures. Bone scanning demonstrates abnormal findings early in the continuum of the stress response by detecting the increased bone metabolism and osteoblastic activity associated with osseous remodeling. Bone scanning shows abnormalities early in the course of a stress fracture, which is often days to two weeks before the radiographic changes become obvious.
Ultrasonography can be used to evaluate superficial bone cortices such as feet and distal tibia. It can also depict periosteal and muscle edema, cortical fracture lines, and callus.
Painful Accessory Bones
Potentially painful normal variants, such as accessory tarsal navicular and os trigonum, have been described with chronic foot pain.16,17 The accessory tarsal navicular is situated adjacent to the medial and posterior margins of the tarsal navicular and has a prevalence of 4 to 14 percent.16 Os trigonum is located adjacent to the posterior margin of the talus and has a prevalence of 14 to 25 percent.16
The mechanism of pain in the presence of an accessory tarsal navicular has been attributed to traumatic or degenerative changes at the synchondrosis or to soft-tissue inflammation. Symptomatic accessory tarsal navicular bones have been studied with bone scanning and MRI. Symptomatic lesions are reported to show increased radiotracer uptake or marrow edema across the synchondrosis.
For a painful os trigonum, fluoroscopy-guided contrast injection of the synchondrosis followed by local anesthetic injection localizes the source of pain.17
Reflex Sympathetic Dystrophy
Complex regional pain syndrome (CRPS) type 1, also known as reflex sympathetic dystrophy (RSD), is characterized clinically by pain, tenderness, swelling, diminished motor function, and vasomotor instability. The term CRPS describes abnormally intense and prolonged pain that is not related to tissue damage and that is sometimes a sequela of injury.18 CRPS is a clinical entity that includes pain combined with autonomic dysfunction, atrophy, and functional impairment. There are two types of CRPS: type 1 (RSD), in which there is no identifiable peripheral nerve lesion; and type 2 (causalgia), in which an identifiable peripheral nerve injury is present.18 Early diagnosis favorably affects outcome.
Diffuse osteopenia of the involved part, which can be demonstrated on radiography, occurs in 69 percent of patients with RSD.19 The osteopenia patterns are not pathognomonic and can occur as a result of disuse. Three-phase radionuclide scans have been used to diagnose RSD.19,20 In the three-phase bone scan, the first phase (the blood-flow phase) imaging is performed by acquiring dynamic two- to five-second images over the area of clinical concern for 60 seconds after the bolus intravenous injection. In the second phase (the blood-pool or soft-tissue phase), imaging is acquired within five minutes after injection. In the final phase (the delayed-skeletal phase), the images should be acquired approximately two to four hours after injection to maximize clearance of the radiopharmaceutical from the overlying soft tissues. Three-phase bone scans do not provide pathognomonic evidence of RSD.18 Delayed bone-scan pattern, which consists of diffuse increased tracer throughout the foot and juxta-articular accentuation of tracer uptake, has been reported.20 Although there are no specific findings,21 MRI appears to be useful in demonstrating soft-tissue abnormalities and ruling out other conditions in patients with RSD.22
Tarsal Tunnel Syndrome
The tarsal tunnel is located deep to the flexor retinaculum, posterior and inferior to the medial malleolus. It contains the posterior tibial nerve; the tibialis posterior, flexor digitorum longus, and flexor hallucis longus tendons; and the posterior tibial artery and vein. In most cases, the posterior tibial nerve divides into terminal branches (the medial and lateral plantar nerves) within the tarsal tunnel.
Tarsal tunnel syndrome is a compressive entrapment neuropathy of the posterior tibial nerve or one of its branches. Patients typically complain of poorly localized, burning pain and paresthesias along the plantar surface of the foot and toes. Causes of tarsal tunnel syndrome include varicosities, trauma, fibrosis, accessory muscles, ganglion cysts, lipoma, and nerve sheath tumors. Such lesions are best visualized using MRI.23 Plain radiography is useful for evaluating fracture or osteophytes that cause tarsal tunnel syndrome, and ultrasonography is helpful in patients with mass lesions in the tarsal tunnel.
Avascular Necrosis of the Metatarsal Head (Freiberg's Disease)
Freiberg's disease is characterized by pain, tenderness, swelling, and limitation of motion in the affected metatarsophalangeal joint.24 The second metatarsal is most commonly affected, although the third and fourth can occasionally be involved. The disease is usually detected in adolescents and is more common in adolescent females than males by a ratio of three or four to one. Radiographic changes are characteristic; they show increased density of the metatarsal head and flattening, collapse, cysticchanges, and widening of the metatarsophalangeal joint.
The cause of Freiberg's disease is controversial and is probably multifactorial. A traumatic insult in the form of acute or repetitive injury and vascular compromise are the most popular theories.25 Bone scanning shows photopenia, decreased uptake in early stages, and increased uptake as the metatarsal head is reconstituted. MRI is helpful for the preoperative evaluation to show the full extent of the lesion.
Tarsal Coalition
Tarsal coalition is deformity that results from abnormal bridging across two or more tarsal bones. Three types of coalition exist: fibrous (syndesmosis), cartilaginous (synchondrosis), and osseous (synostosis) fusion. The true incidence of tarsal coalition in the general population is unknown, but it is less than 1 percent.26 The coalition is bilateral in about one half of patients. Calcaneonavicular coalition is the most common, with a relative incidence of about 53 percent. Approximately 37 percent of patients with tarsal coalition have talocalcaneal (subtalar) coalition, which most commonly involves the middle facet at the level of the sustentaculum tali.
Calcaneonavicular coalition may be detected on oblique anteroposterior radiography of the foot (Figure 5). Talocalcaneal coalition is often associated with severe valgus deformity of the hindfoot, rigid painful flatfoot, and restricted subtalar motion. It is often overlooked on plain radiographs because of overlapping structures; however, secondary signs on the lateral view could be suggestive of talocalcaneal coalition (Figure 6). These signs include talar beaking,27 flattening and broadening of the lateral talar process, positive C sign,28–30 absent middle facet sign,31 and narrowing of the posterior talocalcaneal joint. The term “talar beak” refers to a flaring of the superior margin of the talar head visible on lateral radiographs.27 The C sign refers to the presence of a C-shaped line formed by the medial outline of the talar dome and the posteroinferior outline of the sustentaculum tali on lateral radiographs.29 The C sign is related to abnormal talocalcaneal orientation and is observed in patients with flatfoot.30 Absent middle facet sign refers to the obscured middle facet of the subtalar joint on standing lateral radiographs.31 A well-penetrated axial view (Harris-Beath view) can demonstrate the posterior and middle subtalar joints.


Although CT and MRI are not the imaging studies of choice for tarsal coalition, CT of the subtalar joint is usually diagnostic,32 and MRI has been shown to be effective in depicting all types of coalition. Inversion-recovery MRI may reveal bone marrow edema along the margin of the abnormal articulation, which is an important clue to the diagnosis.
Final Comments
Physicians should be aware of the various imaging modalities available for diagnosing and managing chronic foot pain. Careful analysis of imaging findings and correlating them with the patient's history and physical examination, as well as considering the anatomic location of the injury, can help physicians prescribe the appropriate treatment. Plain radiography is the most cost-effective modality and is the standard initial imaging technique for many conditions of chronic foot pain such as arthritis, Freiberg's disease, or RSD. For other conditions, such as Morton's neuroma, painful accessory bones, or tarsal tunnel syndrome, MRI and ultrasonography could be useful.