
Am Fam Physician. 2007;76(8):1197-1198
Author disclosure: Nothing to disclose.
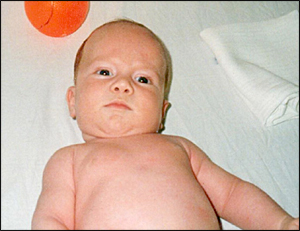
A woman brought her three-month-old infant to the physician for an examination because she was concerned about the position of the infant's head. The pregnancy and delivery were unremarkable. Physical examination revealed that the head and body were in an asymmetrical position (see accompanying figure); otherwise, the infant appeared normal. Passive range of motion in the neck was almost normal with no tightness. There was no palpable tumor of the sternocleido-mastoid muscle. Neurologic examination and an ultrasound scan of the neck muscles were normal.
Question
Discussion
The answer is D: postural torticollis. A typical clinical feature of postural torticollis is the head tilted toward the affected sternocleido-mastoid muscle with the face rotated in the opposite direction. Postural torticollis is a variant of congenital muscular torticollis.
Patients may be classified as having congenital muscular torticollis with or without a sternocleidomastoid tumor or with postural torticollis.1 Patients with a sternocleidomas-toid tumor present with a palpable mass, whereas patients with congenital muscular torticollis without a tumor have tightness and thickening of the sternocleidomastoid muscle, but no palpable mass. Patients with postural torticollis do not have a tumor or tightness of the muscle.2
Postural torticollis is a painless condition that typically presents during infancy.2 The condition usually resolves within a few months without the need for operative treatment.1 Potential complications include cervical scoliosis with compensatory thoracic scoliosis, facial asymmetry, and plagiocephaly.3
After a child is diagnosed with postural torticollis, the family may be educated about a home stretching program and positional cues to encourage functional stretching and use of the muscle. Stretching helps resolve torticollis, but follow-up is needed to assess progress.2
Common home stretching programs focus on sustaining side-to-side and ear-to-shoulder stretches and positioning the child to look toward the unaffected side to see and play with toys. The mean duration of treatment is longer in children who have congenital muscular torticollis with a sternocleidomastoid tumor (7.31 months) compared with those who have muscular torticollis without a tumor (3.85 months) or postural torticollis (2.34 months).4
Benign, paroxysmal torticollis of infancy presents between two and eight months of age as recurrent episodes of head tilting. The condition usually is accompanied by vomiting, pallor, irritability, ataxia, and drowsiness.
Neurogenic torticollis presents as an acute episode in a child with a previously normal head and neck position. This condition usually occurs in older children with neurologic abnormalities.
Osseous torticollis is caused by a congenital malformation of the cervical spine. Passive range of motion in the neck is limited without tightness and thickening of the sternocleidomastoid muscle. Manipulation should be avoided until radiography is performed.
| Condition | Characteristics |
|---|---|
| Benign, paroxysmal torticollis | Recurrent episodes of head tilting, usually accompanied by vomiting, pallor, irritability, ataxia, and drowsiness |
| Congenital muscular torticollis | Tightness and thickening of the sternocleido-mastoid muscle, with or without a muscle tumor |
| Neurogenic torticollis | An acute episode of torticollis that usually occurs in older children with neurologic abnormalities |
| Osseous torticollis | Congenital cervical spine malformations |
| Postural torticollis | No tightness or tumor of the sternocleidomastoid muscle |