
Am Fam Physician. 2007;76(11):1614-1618
Author disclosure: Nothing to disclose.
to the editor: We appreciated the article on cutaneous melanoma that appeared in the July 15, 2005, issue of American Family Physician, especially the excellent color photos.1 According to estimates made by the American Cancer Society, there will be 59,940 new cases of melanoma and 8,110 melanoma-related deaths in the United States in 2007.2 Melanoma cases are increasing by slightly less than 3 percent annually.2
A particularly dangerous form of melanoma is colorless or amelanotic melanoma. Approximately 2 to 8 percent of all melanoma cases are amelanotic melanoma.3 Because of a lack of pigment, amelanotic melanomas are more difficult for patients to recognize, are significantly more challenging to diagnose, and have a significantly higher mortality rate than pigmented melanomas.4
We present three cases of amelanotic or lightly colored melanoma occurring on the lower extremities. All three cases presented in a single year to the same podiatry practice.
The first patient is a 68-year-old black woman with a chronic wound on the posterior left heel, which developed following spur removal surgery several months earlier. The left posterior heel had a growing mass (2 cm × 2 cm × 1.5 cm) that was pedunculated, multilobulated, and acanthotic; with marginal dehiscence and granulation; and an excoriated macule with satellite lesions (Figure 1A). Differential diagnoses included foreign body granuloma, infected ulceration, and melanoma. Excision and biopsy of the mass indicated lightly colored malignant melanoma penetrating 6 mm deep. The patient was referred to an oncologist for further care and is still alive one year later.
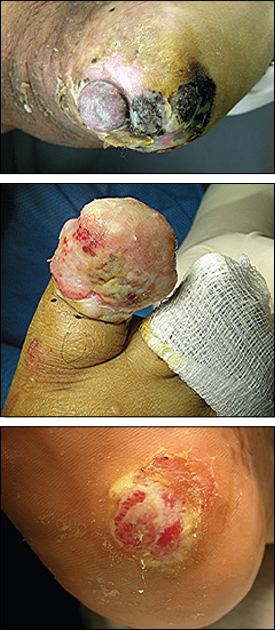
The second patient is a 48-year-old Hispanic woman with a right hallux mass. The patient was first diagnosed with paronychia with granuloma, and a biopsy was not initially performed. The patient subsequently developed a growing and nonpigmented bleeding mushroom cap mass of the right hallux. The mass appeared as a lobulated, pedunculated granuloma (5 cm × 4 cm × 4 cm) with a maximal penetration of 10 mm (Figure 1B). A biopsy of the excised right hallux mass indicated amelanotic malignant melanoma involving skin and soft tissue. The surgical wound healed well, and the patient was sent to an oncologist for further care. However, the patient did not follow up and died six months after the mass was removed.
The third patient is a 70-year-old Hispanic woman with pain on ambulation from a four-year-old enlarging mass on the right plantar heel. Previous physicians had diagnosed verruca plantaris, foreign body granuloma, and callus. The tumor appeared as a mosaic, raised, lobulated macule with granuloma formation (Figure 1C). Wide surgical excision resulted in a mass that measured 3.8 cm × 2.6 cm × 1 cm. Lesion biopsy indicated amelanotic malignant melanoma penetrating to a depth of 15 mm. Further surgery was performed and the patient is well 18 months after surgery.
These three cases illustrate that amelanotic melanomas on the feet occur in many forms and are often difficult to diagnose. Family physicians must be vigilant for amelanotic melanoma and recommend biopsy or sub-specialist referral for suspicious skin lesions, especially when located on the foot.