
Am Fam Physician. 2008;77(1):89-90
Author disclosure: Nothing to disclose.
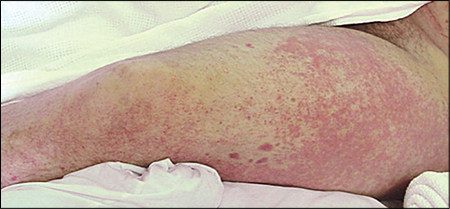
A 40-year-old man presented with a rash on his legs. Three days earlier, the patient had been evaluated in the emergency department for lower leg pain that developed after running. He was diagnosed with leg cramps and was told to stretch and put ice on his legs. Soon after applying the ice, his leg pain worsened and a rash abruptly appeared. The patient was otherwise healthy and had no recent history of illness or other medical problems, allergies, or new medication use.
Physical examination revealed that he was not in distress and had normal vital signs. However, he had patches of palpable, non-blanching, confluent, erythematous papules extending bilaterally from his feet to his thighs (Figures 1 and 2). The papules were not painful or pruritic. Complete blood count and chemistry panel findings were unremarkable.

Question
Discussion
The answer is B: essential mixed cryoglobulinemia. Essential mixed cryoglobulinemia is a multisystem disease caused by cryoglobulin deposition in small- and medium-size blood vessels. Cryoglobulins are antibodies that precipitate at low temperatures and redissolve when warmed. Cryoglobulin deposition causes a vasculitis that leads to petechiae and palpable purpura. Although there is no clear temperature association, exposure to cold temperature is thought to trigger essential mixed cryoglobulinemia in some patients.1,2
The initial clinical presentation of essential mixed cryoglobulinemia varies. Although a triad of purpura, arthralgia, and weakness is the classic presentation, it occurs in less than 30 percent of patients.3,4 Purpura is apparent in nearly one half of patients with essential mixed cryoglobulinemia at presentation and eventually develops in all patients with the condition.2 Other findings associated with essential mixed cryoglobulinemia include a history of Raynaud's phenomenon, multijoint arthritis, renal and liver impairment, and peripheral neuropathy. Diagnosis is based on history; presence of recurrent palpable purpura; and laboratory findings showing low complement levels, elevated rheumatoid factor, and high circulating cryoglobulin levels.4
The exact etiology of essential mixed cryoglobulinemia is unknown; however, it appears to be related to certain liver, autoimmune, and lymphoproliferative disorders. The most notable association is with hepatitis C infection; as many as 98 percent of patients with essential mixed cryoglobulinemia have concomitant hepatitis C infection.5 Thus, any patient being evaluated for essential mixed cryoglobulinemia should also be evaluated for hepatitis C infection.
Treatment depends on symptom severity, organ involvement, and concomitant disease. Arthralgias may respond to nonsteroidal anti-inflammatory drugs alone, whereas end-organ damage may require more aggressive therapy, including corticosteroids, plasmapheresis, or immunosuppressants. Patients with concomitant hepatitis C infection may also need antiviral therapy.6
Cold urticaria lesions are erythematous wheals with central pallor. Although the lesions are induced by exposure to cold temperature, they are pruritic and nonpetechial and fade quickly.
Henoch-Schönlein purpura is an immunoglobulin A–mediated systemic vasculitis that causes a purpuric rash on the lower legs and arms. Patients usually have constitutional symptoms such as arthralgias or abdominal pain. Although Henoch-Schönlein purpura is traditionally considered a childhood disease, it has also been reported in adults.7
Idiopathic thrombocytopenic purpura is caused by the autoimmune destruction of platelets, leading to a petechial, nonblanching rash.
Schamberg's disease is an uncommon, benign condition caused by hemosiderin deposition in the skin, leading to speckled, orange-brown discoloration.7
| Condition | Characteristics |
|---|---|
| Cold urticaria | Pruritic, erythematous, nonpetechial wheals with central pallor that are induced by exposure to cold temperature; positive cold-stimulation test result if wheal develops after skin has been rewarmed |
| Essential mixed cryoglobulinemia | Cryoglobulin deposition in small- to medium-size blood vessels causing vasculitis, petechiae, and palpable purpura |
| Henoch-Schönlein purpura | Immunoglobulin A–mediated systemic vasculitis causing a purpuric rash on the extremities; typically associated with arthralgias and abdominal pain; usually affects children |
| Idiopathic thrombocytopenic purpura | Autoimmune destruction of platelets causing a petechial, nonblanching rash; may present with easy bruising or bleeding |
| Schamberg's disease | Hemosiderin deposition from leakage of surface blood vessels; orange-brown, speckled discoloration; typically affects lower limbs |