
Am Fam Physician. 2008;78(3):379-384
Author disclosure: Nothing to disclose.
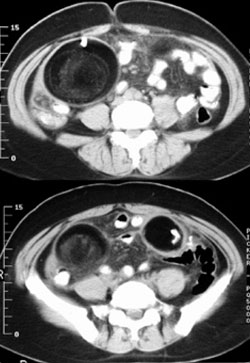
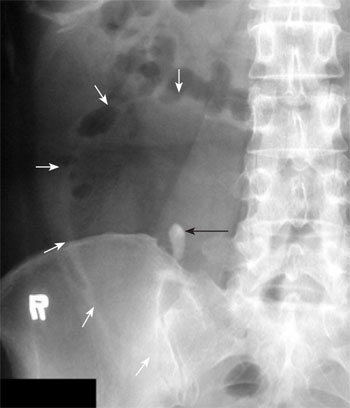
A 42-year-old woman presented with sudden onset of pain in the right lower quadrant after heavy exercise. The pain was accompanied by nausea and four episodes of vomiting. On physical examination, her temperature was 100.4°F (38°C), her pulse rate was 98 beats per minute, and her blood pressure was 98/60 mm Hg. She had direct and rebound tenderness in the right lower quadrant. Her white blood cell count was 10,900 per mm3 (10.9 × 109 per L) with 84.9 percent neutrophils. Urinalysis revealed 10 red blood cells per mm3 and 5 white blood cells per mm3. Plain abdominal radiography (Figure 1) and computed tomography (Figure 2) were performed.

Question
Discussion
The answer is D: torsion of an ovarian cystic teratoma. Abdominal radiography shows a tooth-like object in the right lower abdomen and calcification in the left lower abdomen. In a close-up view of the right lower abdomen, the object is seen more clearly within a well-demarcated, round-shaped area of peripheral radiolucency (Figure 3); this is indicative of a fat component. Computed tomography (CT) shows two masses containing tooth-like calcifications, hypoattenuated areas consistent with fat, and a whirlpool-like appearance suggestive of tufts of hair (Figure 2). Oophorectomy confirms bilateral ovarian cystic teratomas with torsion of the right tumor.
Mature cystic teratomas are composed of three germ layers (ectoderm, mesoderm, and endoderm) and usually occur in the sacrococcygeal region or in the gonads, particularly the ovaries. These teratomas account for 11.2 to 20 percent of all ovarian tumors, and 80 percent of mature cystic teratomas occur during the reproductive period.1 They are usually asymptomatic and are often an incidental finding on physical examination or imaging or during unrelated abdominal or pelvic surgery. When symptoms occur, they commonly include abdominal pain or swelling, an abdominal mass, or abnormal uterine bleeding. Torsion is the most common complication, and it occurs more frequently in patients with medium-sized tumors than in those with small or extremely large tumors.2 Simple cystectomy or salpingo-oophorectomy is recommended if complications occur.
On plain radiography, a tooth within a fatty density is the key finding for a mature cystic teratoma. However, CT is the preferred imaging modality because of its ability to evaluate complex components (e.g., teeth and other calcifications, tufts of hair, fat, hemorrhage, signs of malignant change).1,2 Magnetic resonance imaging is an alternative modality.
Plain radiography is neither specific nor cost-effective in the diagnosis of acute appendicitis. A radiopaque fecalith is visible in the right lower quadrant in fewer than 5 percent of patients with acute appendicitis.3 The most suggestive CT findings of appendicitis are an inflamed appendix (larger than 6 mm in diameter), appendiceal wall thickening with wall enhancement, and periappendiceal inflammatory changes.3
Gastrointestinal bezoar (poorly digested fruit or vegetable fiber, hair, or both) may occasionally cause intestinal obstruction. Plain radiography usually shows mottled radiolucencies in the interstices of a solid mass. A CT finding of an intraluminal mass with a mottled air pattern is characteristic of the condition. CT is also more effective than plain radiography for visualizing concomitant gastric and intestinal bezoars.4
Plain radiography is usually unreliable for diagnosing nonmetallic foreign bodies that may have perforated the gastrointestinal tract. CT may show the foreign body itself, as well as signs of inflammation following perforation (e.g., intestinal wall thickening, localized pneumoperitoneum, regional fat stranding, intestinal obstruction).5
A calcified shadow in the right lower abdomen visible on plain radiography may suggest ureterolithiasis in a patient with hematuria and abdominal pain. However, nonenhanced CT is the test of choice for renal stones because it can rule them in or out.6 Nonenhanced ultra–low-dose CT has a reported sensitivity of 97 percent and specificity of 95 percent for the diagnosis of renal and ureteral stones; the dose of radiation is within the range used in plain radiography.7
| Condition | Characteristics of radiologic findings | |
|---|---|---|
| Plain radiography | Computed tomography | |
| Acute appendicitis | Nonspecific; a radiopaque fecalith is visible in fewer than 5 percent of patients | Inflamed appendix (larger than 6 mm in diameter), appendiceal wall thickening with wall enhancement, and periappendiceal inflammatory changes |
| Gastrointestinal bezoar | Mottled radiolucencies in the interstices of a solid mass | Intraluminal mass with a mottled air pattern (characteristic) |
| Ingested foreign body | Usually unreliable for nonmetallic foreign bodies | May show the foreign body itself; signs of perforation, such as intestinal wall thickening, localized pneumoperitoneum, regional fat stranding, and intestinal obstruction |
| Ovarian cystic teratoma | A tooth or other calcifications Within fatty density | Complex tumor components (e.g., teeth and other calcifications, tufts of hair, fat, hemorrhage, signs of malignant change) |
| Ureterolithiasis | Radiopaque spots along the presumed course of the ureter | Ureteral calculi |