
Am Fam Physician. 2008;78(5):615-622
Patient information: See related handout on Hodgkin lymphoma, written by the author of this article.
Author disclosure: Nothing to disclose.
Approximately 8,200 new cases of Hodgkin lymphoma are diagnosed annually in the United States. Common presenting features include painless lymphadenopathy (usually above the diaphragm), cough, fever, night sweats, and weight loss. To decrease late complications, treatment has gradually evolved toward shorter-duration chemotherapy with use of lower-dose, shorter-duration radiation therapy. ABVD (a chemotherapy regimen consisting of doxorubicin, bleomycin, vinblastine, and dacarbazine) is now more commonly used than MOPP (a regimen consisting of mechlorethamine, vincristine, procarbazine, and prednisone) in patients with Hodgkin lymphoma. Many significant complications of therapy (e.g., cardiovascular conditions, infertility, premature menopause, secondary neoplasms) directly reflect the choice of primary treatment and may be reduced by more current treatment strategies. Recurrences of Hodgkin lymphoma are most common in the first few years after diagnosis and treatment. Prognosis is related to the stage of lymphoma, disease bulk, and age of the patient. Currently, more than 80 percent of patients with newly diagnosed Hodgkin lymphoma are expected to be long-term survivors.
Hodgkin lymphoma is a form of cancer that originates in the lymphatic system. The etiology remains uncertain, although some cases are associated with, and perhaps caused by, the Epstein-Barr virus.1 The risk of developing Hodgkin lymphoma following infectious mononucleosis caused by Epstein-Barr virus is only about one case per 1,000 persons.1 Other factors must be involved in the etiology.
Patients with immunosuppressive conditions have an increased risk of Hodgkin lymphoma. Those with human immunodeficiency virus (HIV) infection and acquired immunodeficiency syndrome are approximately 10 times more likely than the general population to develop Hodgkin lymphoma.2 In patients who are HIV-positive, Hodgkin lymphoma is associated with an advanced stage of disease at presentation, unusual sites of disease, and a poorer outcome.
Familial factors may also play a role in the etiology of Hodgkin lymphoma. Same-sex siblings of patients have been found to have a 10-fold higher risk of developing the disease. Also, a monozygotic twin of a patient with Hodgkin lymphoma is at higher risk than a dizygotic twin.3
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| In patients with stage III or IV Hodgkin lymphoma, ABVD is currently considered the treatment regimen of choice. | C | 12, 14 |
| After treatment of Hodgkin lymphoma, chest radiography should be performed at six, 12, and 24 months, and thereafter as clinically indicated. | C | 24 |
| After neck irradiation, evaluation of thyroid function with TSH level should be performed at one, two, and five years. | C | 24 |
Epidemiology
Hodgkin lymphoma accounts for about one seventh of all lymphomas, with approximately 8,200 cases expected to be diagnosed in the United States in 2008.4 Hodgkin lymphoma has a bimodal incidence pattern, with one peak in persons 15 to 34 years of age, and the other in persons older than 60 years.5 Cases rarely occur in children younger than five years. Men are slightly more likely than women to develop Hodgkin lymphoma.4 Although death rates have substantially decreased in the past 30 years, an estimated 1,070 persons died from Hodgkin lymphoma during 2007.4 Table 1 illustrates survival rates following treatment.4
| Years from treatment | Approximate survival rate (%) |
|---|---|
| 1 | 94 |
| 5 | 85 |
| 10 | 82 |
| 15 | 74 |
| 20 | 63 |
Classification and Pathology
World Health Organization classification divides Hodgkin lymphoma into two distinct groups: classical Hodgkin lymphoma and nodular lymphocyte–predominant Hodgkin lymphoma (Table 26). Classical Hodgkin lymphoma is subdivided into four groups: nodular sclerosis, mixed cellularity, lymphocyte rich, and lymphocyte depleted. Nodular lymphocyte–predominant Hodgkin lymphoma is uncommon.6,7
| Classification | % of patients | Characteristics | |
|---|---|---|---|
| Classical | 92 to 97 | ||
| Nodular sclerosis | 60 to 80* | Tends to affect adolescents and young adults; usually presents as localized disease; generally good prognosis | |
| Mixed cellularity | 15 to 30* | More prevalent in children and older adults; often diagnosed at a more advanced stage (therefore, has a somewhat poorer prognosis); associated with HIV infection | |
| Lymphocyte rich | 2 to 7* | Reed-Sternberg cells have a more classical immunophenotype; tends to present at an early stage; good prognosis | |
| Lymphocyte depleted | 1 to 6* | Mainly in older adults; often diagnosed at advanced stage; poor prognosis | |
| Nodular lymphocyte–Predominant | 3 to 8 | Lacks typical Reed-Sternberg cells; shows atypical lymphocytic and histiocytic cells; usually localized disease with indolent course; good prognosis | |
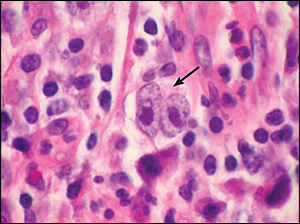
The diagnosis of Hodgkin lymphoma is confirmed by biopsy of lymph node or extra-nodal tissue showing the Reed-Sternberg cell (Figure 1) within the appropriate cellular environment of lymphocytes, eosinophils, histiocytes, neutrophils, plasma cells, fibroblasts, and collagen fibers.6 In contrast with other lymphomas, these tumor cells comprise the minority (1 to 10 percent) of the cellular population of the node. Reed-Sternberg cells, usually of B-cell origin, are not absolutely specific for Hodgkin lymphoma. They have been noted in other lymphomas as well as in carcinomas and sarcomas, and in some benign conditions such as infectious mononucleosis.
Non-Hodgkin lymphomas are classified based on the cell of lineage (i.e., B, T, or natural killer cells) and can be difficult to diagnose because malignant lymphoid cells may resemble benign lymphocytes. Diagnosis of non-Hodgkin lymphoma is often determined by a combination of abnormal cellular architecture, abnormal immunophenotype, and lymphoid monoclonality.8
Presenting Symptoms
The most common presenting symptom of Hodgkin lymphoma is painless lymphadenopathy, often involving cervical, supraclavicular, or axillary nodes. The nodes tend to be freely moveable with a rubbery consistency. In contrast to non-Hodgkin lymphoma, lymphadenopathy in Hodgkin lymphoma generally has a predictable contiguous spread.9 Individual lymph nodes may wax and wane in size. The classic symptom of alcohol ingestion causing enlarged nodes to become painful is actually uncommon.10
Approximately one third of patients with Hodgkin lymphoma present with unexplained fever, night sweats, and recent weight loss, collectively known as “B symptoms.” These symptoms occur more frequently in patients older than 60 years and tend to signify a poorer prognosis. Other common symptoms include cough, chest pain, dyspnea, or superior vena caval obstruction caused by adenopathy in the chest and mediastinum. Some patients may present with more non-specific symptoms, such as fatigue and poor appetite. Dermatologic manifestations include generalized pruritus, erythema nodo-sum, new onset of eczema,11 mycosis fungoides, and ichthyosis. Splenic involvement is present in about one fourth of patients. Other common extranodal sites of involvement are the lungs, liver, bones, and bone marrow.
Laboratory and Imaging Evaluation
Staging is essential to determine the extent and anatomic location of the disease.12 A variety of tests may be useful to diagnose and stage Hodgkin lymphoma to select the optimal treatment strategy. One such staging system is provided in Table 3.12,13 Tests measuring complete blood count, erythrocyte sedimentation rate, electrolytes, renal and liver function, and serum albumin and lactate dehydrogenase levels7 are often performed initially. The complete blood count may show leukocytosis, lymphocytopenia, eosinophilia, or anemia, and the erythrocyte sedimentation rate is often significantly elevated. Serum electrolytes and renal function may be adversely affected by chemotherapy. Liver function tests can indicate the extent of disease involvement. Likewise, low serum albumin and elevated lactate dehydrogenase levels may be negative prognostic factors.
| Stage | Involvement | Five-year relative survival rates (%) |
|---|---|---|
| I | Single lymph node region (I) or one extranodal site (IE) | 90 to 95 |
| II | Two or more lymph node regions, same side of the diaphragm (II) or local extralymphatic extension plus one or more lymph node regions same side of the diaphragm (IIE) | 90 to 95 |
| III | Lymph node regions on both sides of the diaphragm (III), which may be accompanied by local extralymphatic extension (IIIE) | 85 to 90 |
| IV | Diffuse involvement of one or more extralymphatic organs or sites | 80 |
Imaging tests are important in defining the extent of a tumor mass and detecting possible extension into extranodal sites. Appropriate radiographic evaluation may include chest radiography (i.e., posteroanterior and lateral views) and computed tomography (CT; chest, abdomen, pelvis, neck). Positron emission tomography scans are increasingly used in staging because they may reveal disease not detected by other modalities. They can also assist in distinguishing residual non-neoplastic masses from persistent lymphoma.14,15
Although bone marrow aspirate and biopsy may be of benefit in some circumstances, the probability of a positive marrow biopsy in the absence of B symptoms or below-normal blood counts (i.e., anemia, leukopenia, or thrombocytopenia) is less than 0.5 percent, making a bone marrow biopsy unnecessary for most patients. Traditionally, open lymph node biopsy has been the diagnostic procedure of choice, although the diagnosis of Hodgkin lymphoma may also be established by needle biopsy of the node. Preferably, tissue from the most accessible lymph node is used for diagnosis; however, inguinal and axillary nodes are generally avoided because they often show reactive changes. Staging laparotomy is now rarely performed.
Treatment
Treatment strategies (Table 416 ) are determined by the stage of the disease and established prognostic features. International expert groups vary in recommendations, but a broad consensus can be recognized (Tables 58 and 68 ). Toxicity from high-dose radiation and older chemotherapy regimens may be significantly reduced without compromising effectiveness by the increasingly utilized lower-dose, limited-field radiation17 and shorter courses of newer chemotherapy regimens.18 Use of ABVD (a chemotherapy regimen consisting of doxorubicin, bleomycin, vinblastine, and dacarbazine) has been shown to be more effective and less toxic than the previously used MOPP (a chemotherapy regimen consisting of mechlorethamine, vincristine, procarbazine, and prednisone).18,19 A combination of chemotherapy and involved-field radiotherapy is more effective and less toxic than high-dose extended-field radiother-apy.19 Ongoing studies are designed to determine how far treatment may be reduced without compromising effectiveness.
| Stage | Therapy recommendations |
|---|---|
| IA: nodular lymphocyte predominant | Involved-field radiotherapy (35 Gy) |
| I and II (favorable*) | Chemotherapy (ABVD × 2 to 3 cycles) followed by involved-field radiotherapy (30 Gy) |
| I and II (unfavorable*) | Chemotherapy (ABVD × 4 to 6 cycles) followed by involved-field radiotherapy (30 to 35 Gy) |
| III and IV | Chemotherapy (ABVD × 6 to 8 cycles) followed by involved-field radiotherapy (30 to 35 Gy) for initial sites of bulky disease (maximum tumor diameter ≥ 10 cm) |
| North America (United States and Canada) |
| Mediastinal mass ratio > 0.33 |
| Nodal mass > 10 cm |
| Presence of B symptoms (i.e., unexplained fever, night sweats, and recent weight loss) |
| European Organisation for Research and Treatment of Cancer |
| Mediastinal mass ratio > 0.35 |
| Age > 50 years |
| More than three nodal regions |
| Elevated ESR |
| German Hodgkin Study Group |
| Mediastinal mass ratio > 0.35 |
| Extranodal disease |
| More than two nodal regions |
| Elevated ESR |
| Risk factors | ||
|---|---|---|
| Stage IV disease | ||
| Male sex | ||
| Age ≥ 45 years | ||
| Hemoglobin < 10.5 g per dL (105 g per L) | ||
| WBC ≥ 15,000 per μL (15.0 × 109 per L) | ||
| Lymphocyte count < 600 per μL (0.60 × 109 per L) or < 8 percent | ||
| Albumin < 4 g per dL (40 g per L) | ||
| Number of risk factors | Population (%) | Freedom from progression at five years (%) |
| 0 | 7 | 84 |
| 1 | 22 | 77 |
| 2 | 29 | 67 |
| 3 | 23 | 60 |
| 4 | 12 | 51 |
| 5 to 7 | 7 | 42 |
Alternative therapies include Stanford V (a chemotherapy regimen consisting of mechlorethamine, doxorubicin, vinblastine, vincristine, bleomycin, etoposide, and prednisone) and dose-intense regimens such as BEACOPP (bleomycin, doxorubicin, cyclophosphamide, vincristine, procarbazine, prednisone, and gemcitabine). Monoclonal antibody therapy shows promise, particularly two anticluster designation (CD)30 agents—SGN-30 and MDX-060—and the anti-CD20 antibody rituximab (Rituxan).17,18
Outcomes
About 5 to 10 percent of patients are refractory to initial treatment.7 Of those who achieve an initial remission, approximately 10 to 30 percent subsequently relapse.7 In these patients, high-dose chemotherapy sometimes followed by autologous stem cell transplantation (ASCT) may be useful. Patients with progression of disease after ASCT usually have a poor outcome.
Follow-up
Hodgkin lymphoma is the main cause of death for patients who have been diagnosed with a relapse during the first 10 to 15 years after treatment.20 Most relapses occur within the first five years.20 The majority of relapses are discovered by history, with a new lump as the most commonly reported symptom.20 Fever, weight loss, night sweats, cough, and pain may also occur. According to a small study from Canada, 45 percent of relapses were first suspected because of patient-reported symptoms, and 18 percent because of signs detected by the physician.20,21 Similarly, in patients followed by a California center, 14 percent of relapses were detected by physical examination.20,22 Chest radiography has been reported to detect relapses in 5 to 23 percent of patients.20,22,23
The leading international expert groups vary in their recommended follow-up protocols. The Cotswolds Committee recommends that patients be seen at three-month intervals during the first and second years after initial treatment; four-month intervals during the third year; six-month intervals in the fourth and fifth years; and annually thereafter. At each visit, obtaining a complete blood count, erythrocyte sedimentation rate, biochemical profile, and chest radiography is recommended.16 The European Society for Medical Oncology (ESMO) recommends chest radiography at six, 12, and 24 months after therapy, then as clinically indicated.24 The National Comprehensive Cancer Network practice guidelines for Hodgkin lymphoma recommend chest imaging (CT or radiography) every three to six months during the first three years after treatment, and annually beginning with the fourth year.16
However, few data are available on the role of routine blood work or imaging in detecting relapses. Studies suggest that the yield from routine tests in asymptomatic patients is low. In one retrospective study, only one of 157 relapses was detected by routine blood work. The rate of relapse detection was highest for a combination of history and physical examination (78 of 10,000 examinations) followed by chest radiography (26 of 10,000 examinations).16,22 In another study, two of 22 relapses were detected by CT alone, whereas the remaining relapses were discovered clinically.16,21
Secondary Neoplasms and Hematologic Complications
Patients who survive Hodgkin lymphoma are at risk for subsequent neoplasms, especially of the breast and lung. Breast cancer typically occurs after a long latency period (10 to 15 years). The highest risk is in patients who received radiation when younger than 30 to 35 years, and those who received a high dose of radiation.20 Mammography has been shown to be useful in these patients. Both radiation and chemotherapy exposure (especially alkylating agents such as procarbazine [Matulane], mechlorethamine [Mustargen], and dacarbazine [DTIC-Dome]) increase the risk of lung cancer in a dose-dependent fashion. Because tobacco use seems to be a multiplicative risk factor for the development of lung cancer, the importance of smoking cessation should be emphasized. Unlike that of breast cancer, the prognosis for lung cancer after Hodgkin lymphoma is poor, with a median survival of approximately one year.20
The malignancies most often associated with chemotherapy are acute myeloid leukemia and myelodysplastic syndromes.25 The incidence of leukemia appears to be approximately 1 to 3 percent, usually occurring within 10 years of treatment.16 The risk plateaus at 10 to 15 years after therapy.26 The major risk factor for leukemia is exposure to alkylating agents, such as mechlorethamine and procarbazine, both of which were used in the old MOPP regimen. The risk is increased by exposure to wide-field radiation (no longer as commonly done). Chemotherapy with ABVD is associated with a lower risk of leukemia.
Cardiovascular Complications
A wide spectrum of radiation-induced cardiovascular abnormalities may occur in patients who survive Hodgkin lymphoma. These include coronary artery disease, pericardial conditions, cardiomyopathy, valvular abnormalities, and conduction disturbances.27 The main contributor to excess cardiac mortality after having Hodgkin lymphoma is coronary artery disease.28 The strongest risk factor is mediastinal radiation, but patients who were exposed to doxorubicin (Adriamycin) are also at risk for long-term cardiac toxicity. Studies suggest that the current use of lower doses of radio-therapy will likely decrease the incidence of cardiovascular problems.26 Doxorubicin-related cardiomyopathy is associated with female sex, cumulative high doses, younger age at exposure, and increased time from exposure.26 The ability of cardiac screening tests to reduce mortality is presently unproven.
Reproductive Problems
The risks of ovarian failure and infertility increase with age at treatment. Ovarian failure is also associated with higher doses of abdominopelvic radiotherapy and the use of alkylating agents. Hormone therapy may be useful to reduce the risks associated with premature menopause.
In men, spermatogenesis is highly sensitive to mechlorethamine, procarbazine, and cyclophosphamide (Cytoxan). Rates of azoospermia can reach 86 percent.26 The use of ABVD has resulted in lower rates of male infertility. The degree and permanency of radiotherapy-induced damage to the male reproductive system depend on dose, field, and schedule. For men, cryopreservation of sperm before treatment is an effective method of circumventing the sterilizing effect of therapy.
Other Late Complications
Irradiation to the neck and upper mediastinum can result in thyroid abnormalities, especially hypothyroidism. The risk of hypothyroidism is greatest during the first five years after treatment, but new cases can occur even 20 years after irradiation.26 ESMO recommends evaluation of thyroid function at one, two, and five years after treatment in those who have had neck irradiation.24 Neck or pharyngeal radiation may cause decreased salivation, which can lead to dental problems. Prompt dental attention and preventive care may improve dental outcomes.
Pulmonary dysfunction may be a late effect of Hodgkin lymphoma treatment. Lung compromise is a function of the radiation dose and volume of lung exposed, as well as the use of bleomycin (Blenoxane).26 Bleomycin-associated pulmonary fibrosis most commonly occurs after doses of more than 200 U per m2.25
Fatigue is commonly reported by patients following recovery. Possible associations include cardiac disease and hypothyroidism, although one study associated fatigue primarily with pulmonary dysfunction.28
Because Hodgkin lymphoma and its treatment are associated with an increased risk of infections, patients should receive annual influenza immunization and appropriate pneumococcal immunization. Patients who have undergone splenectomy or splenic radiation should also be considered for meningococcal (Menomune) and Haemophilus influenzae (ActHIB; PedvaxHIB; HibTITER [brand no longer available in the United States]) vaccines.