
Am Fam Physician. 2008;78(10):1155-1162
Patient information: See related handout on chronic pain, written by the authors of this article.
Author disclosure: Nothing to disclose.
A systematic approach to chronic nonmalignant pain includes a comprehensive evaluation; a treatment plan determined by the diagnosis and mechanisms underlying the pain; patient education; and realistic goal setting. The main goal of treatment is to improve quality of life while decreasing pain. An initial comprehensive pain assessment is essential in developing a treatment plan that addresses the physical, social, functional, and psychological needs of the patient. One obstacle to appropriate pain management is managing the adverse effects of medication. Opioids pose challenges with abuse, addiction, diversion, lack of knowledge, concerns about adverse effects, and fears of regulatory scrutiny. These challenges may be overcome by adherence to the Federation of State Medical Boards guidelines, use of random urine drug screening, monitoring for aberrant behaviors, and anticipating adverse effects. When psychiatric comorbidities are present, risk of substance abuse is high and pain management may require specialized treatment or consultation. Referral to a pain management specialist can be helpful.
Pain is an unpleasant sensory and emotional experience primarily associated with tissue damage or described in terms of such damage. More than 50 million Americans have chronic pain.1 Chronic nonmalignant pain is pain unrelated to cancer that persists beyond the usual course of disease or injury. It may or may not be associated with a pathologic process.1,2 The estimated annual costs related to chronic pain are $85 to $90 billion.3
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Assessing for risk of abuse should be an integral part of chronic pain management. | C | 5, 6, 28 |
| A written plan for treating chronic pain should state objectives to determine success, state if further diagnostic tests are indicated, address psychosocial and physical function, adjust therapy to meet the needs of the patient, and use nondrug treatment modalities in addition to medication. | C | 2 |
| Patients taking long-acting opioids for chronic nonmalignant pain should be started on long-term preventive therapy with a combination stimulant/softener laxative for constipation. | B | 37 |
Evaluation
Evaluating patients with chronic non-malignant pain requires a systematic approach that encompasses the pathophysiologic, as well as the social and psychological aspects of the condition.2,4 Identifying the pain as nociceptive (tissue injury), neuropathic (a neurologic response to neural or nonneural injury), or mixed; and, if possible, quantifying the pain using visual analog scales will aid in treatment decisions. A thorough social and psychiatric history may alert the physician to issues, such as current or past substance abuse, developmental history, depression, anxiety, or other factors, that may interfere with achieving treatment goals. Validated risk assessment tools for persons at higher risk of opioid abuse include the Opioid Risk Tool (http://www.emergingsolutionsinpain.com/index.php?option=com_content&task=view&id=101&Itemid=100) and the Screener and Opioid Assessment for Patients with Pain–Revised (http://www.painedu.com/soap.asp).5,6 These tools should not be used to deny a patient pain medication, but to help develop a plan for medication monitoring. Pain contracts and visual analog scales can be found at http://www.ohsu.edu/ahec/pain/form.html.5–7 By identifying patients at risk of possible opioid misuse (e.g., persons with past or current substance abuse, persons with psychiatric issues), physicians can choose to modify the monitoring plan or to refer the patient to a pain specialist. Table 1 provides definitions for the terminology used to describe medication dependence and abuse.2
| Term | Definition |
|---|---|
| Addiction | Neurobiologic, multifactorial disease characterized by impaired control, compulsive drug use, and continued use despite harm |
| Physical dependence | Normal adaptive state that results in withdrawal symptoms if the drug is abruptly stopped or decreased |
| Pseudoaddiction | Relief-seeking behaviors misinterpreted as drug-seeking behaviors that resolve upon institution of effective analgesic therapy |
| Substance abuse | Use of any substance for purposes that are non-therapeutic or are not those for which it is prescribed |
| Tolerance | Physiologic state from regular drug use in which an increased dosage is needed to produce the same effect |
Nonverbal patients require modified assessment techniques. Nonverbal patients may communicate pain by moaning, screaming, crying, or making painful facial expressions during manipulation. They may have swelling, may not use the (affected) body part, or may not move the body in a specific way.8 Verbal and nonverbal patients with cognitive or intellectual disabilities can have sensory integration or more global communication disorders; therefore, they may not exhibit this type of non-verbal communication. Instead, chronic nonmalignant pain could present as behavioral challenges or as a gradual decline in function. Appropriate treatment can greatly improve patient quality of life and caregiver stress.
When long-term opioid therapy is considered in a patient with chronic nonmalignant pain, the initial pain assessment note should provide a complete and focused summary of the circumstances leading to the decision to treat with long-term opioids. To provide baseline information for future assessment, the note should cover the diagnosis, quality of the pain (e.g., what palliates and provokes it, radiation, severity, type, temporal sequence), region of the pain, treatments (current and previous), referrals, studies ordered, patient risk factors, and any psychiatric or social considerations.2,4,9
Management of Chronic Nonmalignant Pain
TREATMENT PLAN
Figure 15–7,9 describes a general approach to assessing chronic nonmalignant pain. Management guidelines for specific pain disorders, such as chronic musculoskeletal pain, neuropathic pain, fibromyalgia, and low back pain, have been developed; therefore, a specific diagnosis should be pursued when possible.10–13 Treatment goals focus on the improvement of the social, occupational, psychological, interpersonal, and physical disabilities caused by chronic pain, which adversely affect the patient's quality of life.14 Patient education and setting realistic goals are keys to successful management; these will vary from patient to patient.15 For example, total elimination of pain is rarely a realistic goal, whereas goals to increase pleasurable activities may be achievable.
TREATMENT OPTIONS
Evidence of the effectiveness of most treatment options is lacking or inconsistent. Treatment options are listed in Table 2.16–25 Most chronic pain disorders respond best to a combination of treatment modalities or a multidisciplinary plan. Treatment with nonpharmacologic options, with or without the addition of medication, should be tried initially. Nonpharmacologic modalities require patient participation and motivation, and improve physical mobility, fitness, mood, sleep, and general health.26,27 Treatment of comorbid conditions, depression, anxiety, and sleep issues that commonly accompany chronic pain disorders can improve overall function.26,27 Pharmacologic choices depend upon the diagnosis and whether the mechanism of pain is characterized as neuropathic, nociceptive, or mixed. Neuropathic pain disorders involve abnormal nerve conduction and neuropathies, whereas nociceptive pain includes muscular, inflammatory, or mechanical compression disorders.9 Online Figure A describes the management of chronic nonmalignant pain by mechanism.
| Treatment type | Options |
|---|---|
| Nonpharmacologic | |
| Lifestyle | Cessation of tobacco products, weight loss |
| Physical | Exercise*, manipulation, physical therapy, stretching and yoga, surgical therapies (nerve blocks, trigger point injections, spinal infusion or stimulation), transcutaneous electric nerve stimulation |
| Psychologic | Biofeedback, cognitive behavior therapy†, counseling, hypnosis, music‡, relaxation† |
| Complementary or alternative | Acupuncture, herbal remedies, massage, mindfulness meditation, reflexology |
| Occupational | Occupational therapy, work conditioning programs |
| Pharmacologic | |
| Nonopioid analgesics | Acetaminophen, NSAIDs, salicylates (aspirin) |
| Opioid medications (nonsynthetic, synthetic)§‖ | Combination opioid and nonopioid medications (codeine, hydrocodone [Hycodan], or oxycodone [Roxicodone] plus acetaminophen, aspirin, or an NSAID) |
| Noncombination or “strong” opioid medications, such as morphine (MS Contin) and its derivatives (butorphanol [Stadol], codeine, fentanyl [Duragesic], hydrocodone, hydromorphone [Dilaudid]¶, levorphanol [Levo-Dromoran], methadone, oxycodone) | |
| Tramadol (Ultram) | |
| Adjuvant medications | Anticonvulsant medications (carbamazepine [Tegretol]**, gabapentin [Neurontin]**, lamotrigine [Lamictal], phenytoin [Dilantin], pregabalin [Lyrica], valproic acid [Depakene]) |
| Antidepressants (selective serotonin reuptake inhibitors, tricyclic††) | |
| Atypical antidepressants (duloxetine [Cymbalta], venlafaxine [Effexor]††) | |
| Topical lidocaine (Xylocaine)‡‡ | |
| Others (topical capsaicin, cyclobenzaprine [Flexeril], lidocaine patches) | |
The well-accepted concept of rational polypharmacy, where medications with variable mechanisms are combined, enhances medication effectiveness, reduces required doses, increases quality of life, and addresses sleep and mood.10,28 An example of this is the use of the tricyclic antidepressant amitriptyline for its analgesic and sedating properties (to help with insomnia). Nonopioid medications, such as acetaminophen, nonsteroidal anti-inflammatory drugs, and salicylates, should be tried initially. If ineffective, opioid/nonopioid combinations may be required, but are limited by the maximal dose of the nonopioid component. If moderate or severe pain is present, the use of long-acting opioids may be indicated, and has been shown to improve pain.20–22
OPIOID MEDICATIONS
Reluctance to use long-term opioids is generally because of concerns about abuse, addiction, diversion, and adverse effects; inadequate knowledge; and fear of regulatory scrutiny.2,29 With the increased appropriate use of opioid medications for chronic nonmalignant pain in the United States, there has been an increase in the abuse or nonmedicinal use of opioids.30 This increase is small compared with the benefits of appropriate pain management and the use of other illicit substances (e.g., cocaine, marijuana, heroin).30 There are many resources that provide detailed discussions regarding the safe, effective, and appropriate use of long-term opioids.11,15,21,31
The Federation of State Medical Boards provides guidelines for evaluating pain treatment, including appropriate chronic opioid medication use (Table 3).2 When followed carefully, these guidelines may help alleviate physician concerns. The decision to use long-term opioids requires careful consideration and is not without risk. The ineffectiveness of nonopioid options should be clearly documented, and there must be a legitimate medical purpose for opioid use. The anticipated benefits must outweigh the risks. Risk assessment tools can be used to identify patients that may be at risk of misuse. Opioid agreements are commonly used, with the intent to deter misuse and to outline patient responsibilities for obtaining opioids.31 Using an opioid agreement also provides an opportunity for a documented discussion about medication adverse effects, complications, and risks.
| Step | Description | |
|---|---|---|
| Evaluation | Perform and document a medical history and physical examination that includes: | |
| Nature and intensity of pain | ||
| Current and past treatment for pain | ||
| Underlying and coexisting disease or conditions | ||
| Effect of pain on function (physical and psychiatric) | ||
| History of substance abuse | ||
| Documentation if a controlled substance is indicated medically | ||
| Treatment | A written treatment plan should: | |
| State objectives to determine success | ||
| State if further diagnostic tests are indicated | ||
| Address psychosocial and physical function | ||
| Adjust therapy to meet needs of patient | ||
| Informed consent and agreement for treatment | Discuss risks and benefits of drug therapy with patient or surrogate | |
| Patient should receive prescriptions from one physician and pharmacy whenever possible | ||
| High-risk patients should have a written agreement that includes: | ||
| Urine drug screens when requested | ||
| Written documentation of refill numbers and frequency | ||
| Reasons for which drug therapy may be discontinued (violations of agreement) | ||
| Consultation | Be willing to refer; special attention should be given to patients at risk of medication misuse, abuse, or diversion | |
| Consultation may be required in patients with psychiatric disorders or substance abuse issues (past or present) | ||
| Periodic review | Periodically review the course of pain treatment and any new information about the etiology of the pain | |
| Evaluate and modify drug treatment based upon patient response and objective evidence of improved or diminished function; if progress is unsatisfactory, assess the appropriateness of continuing or modifying therapy | ||
| Medical records | Medical records should include: | |
| Medical history and physical examination | ||
| Diagnostic tests and laboratory results | ||
| Evaluations and consultations | ||
| Treatment objectives and treatments | ||
| Informed consent and discussion of risks and benefits | ||
| Medication and refill documentation | ||
| Instructions and agreements | ||
| Periodic reviews | ||
| Records are to be current and easily accessible for review | ||
| Compliance with controlled substances laws and regulations | State and federal regulations must be met | |
| Refer to U.S. Drug Enforcement Administration and state medical boards for relevant documents | ||
The initial medication choice depends on the pain condition, severity, comorbid disorders, and physician preference. Initial treatment requires upward dose titration to optimal effect with minimal adverse effects. Long-acting opioids are preferred because they provide consistent pain control levels. Although many authors discourage the use of short-acting opioids for chronic nonmalignant pain, breakthrough pain and acute exacerbations of pain can be addressed with short-acting opioids. Table 4 provides the six A's for monitoring patients with chronic nonmalignant pain who are taking controlled substances.11
| Analgesia (assess pain relief) |
| Affect (evaluate mood) |
| Activities (evaluate activities of daily living, function, and quality of life) |
| Adjuncts (nonpharmacologic or nonopioid treatments) |
| Adverse effects (side effects of treatments) |
| Aberrant behavior (tolerance, dependence, and addiction) |
PERIODIC REVIEW
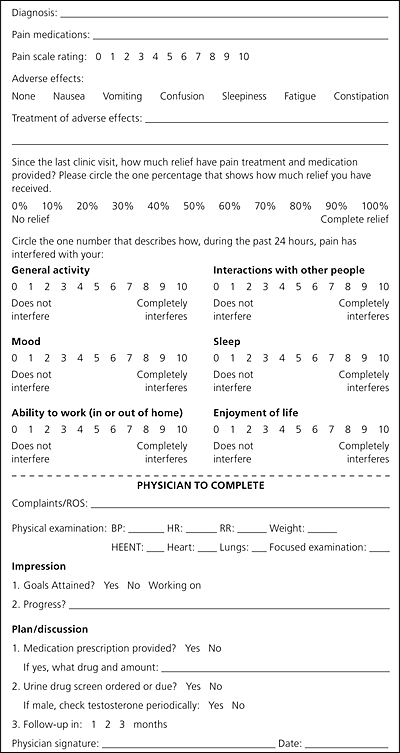
Periodic review (follow-up visits) allows for the monitoring of treatment effectiveness, nonpharmacologic therapy compliance, and patient behaviors that may indicate violation of the opioid agreement or medication misuse. Periodic review also provides direction for further treatment and goal revision. Figure 2 is a sample of a tool that may be used for periodic review.11 Accurate documentation and adherence to state and federal drug regulations are essential for appropriate management (Table 3).2
DIVERSION AND ABUSE
For patients at high risk of diversion and abuse, consider the routine use of random urine drug screens to assess for presence of prescribed medications and the absence of illicit substances. Prescriptions should be appropriately written to decrease the incidence of medication misuse (e.g., write out pill count, limit to one pharmacy).32
URINE DRUG SCREENS
Urine drug screening is not legally required, but it is recommended in many guidelines.2,11 When used appropriately, urine drug screening can assist in the management of opioid therapy by uncovering illicit drug use and confirming compliance with treatment, even in the absence of behaviors suggestive of medication misuse. The urine drug screen can help solidify physician-patient trust by establishing the presence of the prescribed controlled substance in urine, thus alleviating any concerns about diversion or trafficking. Screening should be performed randomly.
Morphine can be detected in the urine for 1.0 to 1.5 days.32 Testing for synthetic controlled substances (opioids) must be done separately because standard urine drug screens only test for opiates (e.g., heroin, codeine, morphine [MS Contin]), tetra-hydrocannabinol, cocaine, phencyclidine, barbiturates, and amphetamines/methamphetamines. When interpreting urine drug screens, knowledge of metabolites and breakdown products is essential in order to avoid false-positive results (taking an unprescribed drug). For example, codeine is broken down to smaller amounts of morphine, thus the screen will be positive for both if the patient takes codeine. Hydrocodone (Hycodan) is metabolized to hydromorphone (Dilaudid). Codeine, if taken in high quantities, can also be metabolized to small amounts of hydrocodone.32 Before urine drug screening, physicians should explain their policy for a positive result to the patient (screen positive for non-prescribed or illicit substances, or absence of prescribed substance). A positive urine drug screen may not necessarily result in dismissal of the patient, but it must be addressed. Actions could include referral for substance abuse counseling or treatment and refusal to prescribe further controlled substances.
ABERRANT BEHAVIOR
Aberrant behavior that may suggest medication misuse includes use of pain medications other than for pain treatment, impaired control (of self or of medication use), compulsive use of medication, continued use of medication despite harm (or lack of benefit), and craving or escalation of medication use.26 Other aberrant behaviors include selling or altering prescriptions, stealing or diverting medications, calls for early refills, losing prescriptions, drug-seeking behavior (e.g., doctor shopping), or reluctance to try nonpharmacologic interventions.26
PSYCHIATRIC ISSUES
Psychiatric problems commonly occur with chronic nonmalignant pain. In one study, 77 percent of those with chronic nonmalignant pain secondary to low back pain have a lifetime psychiatric diagnosis compared with 46 percent of the general U.S. population.33,34 Fifty-nine percent had a current and active psychiatric diagnosis compared with 26 percent of the general U.S. population.33,35 Common psychiatric disorders in those with chronic nonmalignant pain include anxiety; mood, personality, and somatoform disorders; and substance abuse.36
MEDICATION ADVERSE EFFECTS
Finally, medication adverse effects, especially of opioids, need to be addressed and anticipated. The most common adverse effects are somnolence, nausea, sedation (tolerance or resolution usually develops within 10 days), and constipation (no tolerance or resolution develops).37 Those on long-acting opioids should be started on long-term preventive therapy with a combination stimulant/softener laxative and considered for short-term (10 days) therapy with antinausea medication.37 The main etiology for constipation in patients taking opioids is slowing of stool transit time; therefore, avoidance of stool bulking agents is prudent because they can worsen constipation.31
Referral
When pain problems remain intractable and unremitting, referral to a pain management specialist may be helpful.26,31 Consultation can help provide other approaches to assessment or management of complex pain problems or determine interventional procedures to relieve pain. Psychosocial indications for a pain consultation can include a history of substance abuse, as well as interpersonal dynamics that seem to complicate the treatment of pain.33,36