
Am Fam Physician. 2009;79(2):109-116
A more recent article on pigmentation disorders is available.
Author disclosure: Nothing to disclose.
Common causes of hyperpigmentation include postinflammatory hyperpigmentation, melasma, solar lentigines, ephelides (freckles), and café-au-lait macules. Although most hyperpigmented lesions are benign and the diagnosis is straightforward, it is important to exclude melanoma and its precursors and to identify skin manifestations of systemic disease. Treatment options for postinflammatory hyperpigmentation, melasma, solar lentigines, and ephelides include the use of topical agents, chemical peels, cryotherapy, or laser therapy. Café-au-lait macules are amenable to surgical excision or laser treatment. Disorders of hypopigmentation may also pose diagnostic challenges, although those associated with health risks are uncommon and are usually congenital (e.g., albinism, piebaldism, tuberous sclerosis, hypomelanosis of Ito). Acquired disorders may include vitiligo, pityriasis alba, tinea versicolor, and postinflammatory hypopigmentation. Treatment of patients with widespread or generalized vitiligo may include cosmetic coverage, psoralen ultraviolet A-range therapy (with or without psoralens), or narrow-band ultraviolet-B therapy; whereas those with stable, limited disease may be candidates for surgical grafting techniques. Patients with extensive disease may be candidates for depigmentation therapy. Other acquired disorders may improve or resolve with treatment of the underlying condition.
Although most pigmentation disorders are benign or nonspecific, some disorders of skin pigmentation present cosmetic or psychological challenges to the patient, necessitating evaluation and treatment. Others may be indicators of underlying systemic disease or primary skin malignancy. Proper diagnosis of these common skin conditions will allow the physician to facilitate appropriate skin treatment and reassure the patient.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Postinflammatory hyperpigmentation may be improved with hydroquinone (Eldoquin Forte), azelaic acid (Azelex), retinoids, glycolic acid peels, and laser therapy; monotherapy is often unsatisfactory. | C | 4–6 |
| Treatment of epidermal melasma with triple therapy is more effective than treatment with hydroquinone, fluocinonide (Lidex, brand no longer available in the United States), or tretinoin (Retin-A) alone or in double combination. | B | 16, 17 |
| Chemical peels and brief cryotherapy are effective ablative treatments for solar lentigines. | C | 20–22 |
| For the treatment of localized and generalized vitiligo, high-potency steroids, topical or oral psoralens with psoralen ultraviolet A-range, and narrow-band ultraviolet-B therapies are beneficial. Vitiligo of the head and neck is most responsive to treatment. | B | 32, 36–44 |
Pathophysiology
Pigmentation of skin depends on the amount and type of melanin, degree of skin vascularity, presence of carotene, and thickness of the stratum corneum. Skin hyperpigmentation usually results from an increased number, or activity, of melanocytes. Epidermal increases in melanin usually enhance with a Wood lamp, whereas dermal increases do not. Some disorders, such as melasma, may have dermal and epidermal changes and can be classified as mixed.1 Hypopigmentation of skin may result from a reduction of melanocytes or from an inability of the melanocytes to produce melanin or properly transport melanosomes. Causes of hyper- and hypopigmentation are discussed in this article and are listed in Table 1. Certain skin pigmentation disorders are more common in certain skin types. The most commonly used system for identifying skin types is the Fitzpatrick system (Table 2).2,3
| Hyperpigmentation | |
| Postinflammatory hyperpigmentation (acne, psoriasis, atopic and contact dermatitis, lichen planus, trauma, drugs, and fixed-drug eruptions) | |
| Melasma | |
| Solar lentigines | |
| Ephelides (freckles) | |
| Café-au-lait macules | |
| Nevi | |
| Melanoma and precursors | |
| Hypopigmentation | |
| Acquired (common) | |
| Vitiligo | |
| Pityriasis alba | |
| Tinea versicolor | |
| Postinflammatory hypopigmentation | |
| Congenital (uncommon) | |
| Albinism | |
| Piebaldism | |
| Tuberous sclerosis | |
| Hypomelanosis of Ito | |
| Skin type | Skin color | Characteristics |
|---|---|---|
| I | White; very fair; red or blond hair; blue eyes; freckles | Always burns, never tans |
| II | White; fair; red or blond hair; blue, hazel, or green eyes | Usually burns, tans with difficulty |
| III | Cream white; fair with any eye or hair color; very common | Sometimes mild burn, gradually tans |
| IV | Brown; typically Mediterranean skin | Rarely burns, tans with ease |
| V | Dark brown; Middle-Eastern skin types | Very rarely burns, tans very easily |
| VI | Black | Never burns, tans very easily |
Hyperpigmentation Disorders
POSTINFLAMMATORY HYPERPIGMENTATION
Postinflammatory hyperpigmentation is a common consequence of an injury or inflammation to dark skin (Fitzpatrick types IV to VI), resulting in lesions that can persist for months or years. This can be psychologically devastating to some patients. Postinflammatory hyperpigmentation may also occur after laser therapy for other pigmented skin lesions, and may be transient or long lasting. A typical example can be seen in Figure 1

Postinflammatory hyperpigmentation presents as irregular, darkly pigmented macules and patches at sites of previous injury or inflammation. Treatment is often difficult, requiring prolonged courses of therapy and excellent patient compliance.
Available methods of treatment for postinflammatory hyperpigmentation include hydroquinone 3% or 4% (Eldoquin Forte) twice daily, azelaic acid 20% cream (Azelex) twice daily, salicylic or glycolic acid peels, retinoids, and laser therapy. However, monotherapy often produces unsatisfactory results. In one study, the addition of serial glycolic acid peels to a hydroquinone 2%/glycolic acid 10% combination twice daily and tretinoin 0.05% (Retin-A) at bedtime resulted in faster lightening without significant adverse effects.4 Additionally, retinoids such as tazarotene 0.1% cream (Tazorac) are well-tolerated and somewhat effective at reducing hyper-pigmentation and disease severity.5
Pretreatment with topical therapies has been studied in patients with skin types I to III undergoing carbon dioxide laser resurfacing. No conclusive benefit was noted in one limited trial involving patients at the lowest risk for postin-flammatory hyperpigmentation.6 At present, no preventative measures have proven beneficial in any skin type.
MELASMA
Melasma is a progressive, macular, nonscaling hypermelanosis of sun-exposed areas of the skin, primarily on the face and dorsal forearms. It is usually associated with pregnancy, oral contraceptives, or anticonvulsants (e.g., phenytoin [Dilantin]), or it may be idiopathic. Melasma affects women nine times more often than men, and it is more prominent in patients with skin types IV to VI (e.g., Asian, Middle Eastern, South American). It is usually asymptomatic, but it is often cosmetically distressing to the patient. Melasma typically presents in one of three patterns of distribution: centrofacial (63 percent), malar (21 percent), and mandibular (16 percent). It is usually, but not always, bilateral (Figure 2).

Three types of melasma exist: epidermal, dermal, and mixed. Epidermal melasma tends to be light brown, enhancing under Wood lamp examination. Dermal melasma is usually grayish in color and nonenhancing. Mixed types are dark brown with variable enhancement.
Topical treatment with hydroquinone 3% or 4%, glycolic acid 10% peel, azelaic acid 20% cream, and retinoids (e.g., tretinoin 0.05% or 0.1% cream; adapalene 0.1% or 0.3% gel [Differin]) all have some effectiveness. Combination products with hydroquinone and retinoids, glycolic acid, or topical steroids seem to be somewhat more effective. Typically, treatment must be continued indefinitely to maintain effect.7–15 In one drug-company-sponsored study, a triple-combination treatment of fluocinonide 0.01%/hydroquinone 4%/tretinoin 0.05% cream (Tri-Luma) showed significantly greater effectiveness at improving dyspigmentation than treatment with any two of these ingredients combined, with mild side effects.16,17 Epidermal and mixed types are not often responsive to laser therapies and frequently result in significant postinflammatory hyperpigmentation; therefore, their use cannot be recommended. However, several small studies suggest that dermal or refractory/mixed-type melasmas may be effectively treated with laser therapy or by a combination of intense pulsed-light therapy and hydroquinone with sunscreen.18,19
Prevention of melasma involves decreasing exposure of susceptible skin to ultraviolet (UV) rays. Opaque sunblocks with titanium dioxide or zinc oxide are most effective. There are transparent sunscreens containing these agents as well (e.g., Blue Lizard Sunscreen Sensitive SPF 30+, Neutrogena Sensitive Skin Sunblock 30+, Sol-bar Zinc Sunscreen SPF 38). Melasma that is induced by pregnancy or oral contraceptive use tends to fade within several months after delivery or medication cessation, so watchful waiting should be encouraged in these instances whenever possible.
SOLAR LENTIGINES
Solar lentigines (i.e., liver spots) are macular, 1- to 3-cm, hyperpigmented, well-circumscribed lesions on sun-exposed surfaces of the skin. They vary in color from light yellow to dark brown, and they often have a variegated appearance. The face, hands, forearms, chest, back and shins are the most common locations, erupting after acute or chronic UV exposure. White or Asian persons are most likely to develop solar lentigines, especially those with skin types I to III and a tendency to freckle (Figure 3).
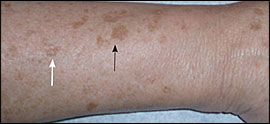
Solar lentigines result from a local proliferation of basal melanocytes and a subsequent increase in melanization, differing from freckles, which result from increased melanin production. Systemic disorders presenting with multiple lentigines may include Peutz-Jeghers syndrome (gastrointestinal hamartomas; buccal, lip, perioral, or digital macules; onset at birth or early childhood), LEOPARD syndrome (multiple lentigines, electrocardiogram abnormalities, ocular hypertelorism, pulmonic stenosis, abnormal genitalia, retarded growth, and sensorineural deafness), and LAMB syndrome (multiple lentigines, atrial and/or mucocutaneous myxomas, myxoid neurofibromas, ephelides, and blue nevi). Solar lentigines must be differentiated from premalignant lesions, such as pigmented actinic keratoses or lentigo maligna. Pigmented lesions with rapid growth or change, associated symptoms (e.g., pain, itching, easy or recurrent bleeding, poor healing), atypical lesions, or those with features suspicious for melanoma should be biopsied. Full thickness excisional biopsy or punch biopsy (for large lesions or those on the face or cosmetically sensitive area) is an acceptable method of biopsy in these instances. Solar lentigines can be distinguished clinically from flat seborrheic dermatoses or pigmented actinic keratoses by the absence of epidermal hyperkeratosis. Biopsy may facilitate diagnosis in uncertain cases.
Treatment of solar lentigines consists of ablative therapies (e.g., chemical peels, cryotherapy, laser therapy) or topical therapies (e.g., hydroquinone, retinoids), and is summarized in Table 3. Chemical peels with 30% to 35% trichloroacetic acid (Trichlor) solution or brief (i.e., less than 10 seconds) cryotherapy with liquid nitrogen have resulted in significant lightening of lentigines, but data are limited on long-term improvements, and recurrences are common. Additionally, cryotherapy can be painful, and prolonged treatment is associated with hypopigmentation.20–22 Laser therapy for solar lentigines has shown benefit in at least one small, randomized controlled trial, with effectiveness superior to liquid nitrogen cryotherapy. The frequency-doubled Q-switched neodymium-doped yttrium aluminum garnet (ND: YAG) laser produced the best cosmetic results and was tolerated best. Postinflammatory hyperpigmentation is a known complication of laser therapy, and must be considered when determining the best treatment option for each patient.22–24
| Treatment | Type/dose | Side effects |
|---|---|---|
| Chemical peels | 30% to 35% trichloroacetic acid (Trichlor) | Transient stinging, burning, pain |
| Cryotherapy | Liquid nitrogen | Pain, hypopigmentation with prolonged exposure |
| Laser therapy | Neodymium-doped yttrium aluminum garnet (ND: YAG) laser | Pain, postinflammatory hyperpigmentation, redness, textural changes, hypopigmentation |
| Hydroquinone (Eldoquin Forte) | 3% to 4% topical | Hypersensitivity, acne, ochronosis |
| Mequinol/tretinoin (Solage) | 2% mequinol/0.01% tretinoin topical solution | Redness, dryness, itching, sensitivity |
| Retinoids | Tazarotene 0.1% cream (Tazorac); adapalene 0.1% or 0.3% gel (Differin) | Redness, dryness, itching, sensitivity |
Topical therapies for solar lentigines are also available. Hydroquinone has been available for more than 30 years and is moderately effective. Adverse effects to hydroquinone include hypersensitivity, acneiform eruptions, and, rarely, ochronosis (i.e., blotchy hyperpigmentation).25,26 Additionally, the lightening effects of hydroquinone are slow (months), and relapse with medication discontinuation is the rule. More recently, a combination of mequinol/tretinoin (Solage) has been shown to be safe and effective in treating solar lentigines, and shows promise for prolonged maintenance.27,28 Retinoids such as tazarotene 0.1% cream and adapalene 0.1% or 0.3% gel may reduce the appearance of solar lentigines, but evidence is limited.29,30
Prevention of solar lentigines depends on limiting sun exposure, using sunscreen regularly (especially in patients with fair skin [types I to III] and those prone to freckling), and preventing sunburns, especially after 20 years of age.
EPHELIDES
Ephelides (i.e., freckles) are small, 1- to 2-mm, sharply defined macular lesions of uniform color, most often found on the face, neck, chest, and arms. Color may vary from red to tan to light brown, and they may vary in number from a few to hundreds. Onset is usually in childhood after sun exposure. They are asymptomatic. Treatment of these lesions is not usually necessary, as they tend to fade during winter months. Cosmetically, undesired lesions can be treated similarly to lentigines (i.e., cryotherapy, hydroquinone, azelaic acid, glycolic acid peels, and laser therapy). These lesions should be differentiated from juvenile lentigines (2 to 10 mm) and solar lentigines (2 to 20 mm), which usually arrive later in life.
CAFÉ-AU-LAIT MACULES
Café-au-lait macules are tan or brown macules ranging in size from 1 to 20 cm, which are present at birth or occur early in life. They are epidermal in origin, representing an increase in melanin in melanocytes and basal keratinocytes. They may be found on any body part, but often are located on the trunk (Figure 4). Ten to 30 percent of the population has an isolated café-au-lait macule.31

Café-au-lait macules are asymptomatic and require treatment for cosmesis only. Laser therapies and surgical excision are effective. More than six café-au-lait lesions (5 mm or larger, prepubertal; and 15 mm or larger, postpubertal) should raise suspicion for an underlying systemic disorder such as tuberous sclerosis, neurofibromatosis, Albright syndrome, or Fanconi anemia.2
Hypopigmented Lesions
VITILIGO
Vitiligo is a disfiguring skin disease resulting in loss of pigmentation. It results from an immune-mediated destruction of melanocytes. Its exact etiology is unknown. Vitiligo affects all skin types and is generally considered a cosmetic condition, but it can cause significant psychological distress, particularly to some black patients.
Vitiligo is found in 1 percent of the general population, affecting males and females equally. Family history of vitiligo is established in 25 to 30 percent of patients.31 Onset is often insidious, but is frequently related to a recent stress, illness, or trauma (e.g., sunburn). Peak onset is in the second and third decades of life, with 50 percent occurring before 20 years of age.31
Lesions in vitiligo consist of unpigmented, sharply defined macules ranging in size from 5 to 50 mm. Some will have a rim of hyperpigmentation or erythema. Common sites of involvement include the face, neck, dorsal hands, genitalia, body folds, and axillae (Figure 5). Perioral, periorbital, periumbilical, and perianal lesions also occur.

Four types of vitiligo exist: generalized, acral/acrofacial, localized, and segmental. Generalized vitiligo involves greater than 10 percent of the body surface area. Acral/acrofacial vitiligo typically involves the face and distal extremities (i.e., the so-called “tip/lip” pattern). Localized vitiligo tends to involve a smaller body surface area and is generally stable in nature. Segmental (i.e., single dermatome or extremity) vitiligo is more often present in children and has a poorer prognosis for treatment.
Treatment of vitiligo depends on the extent of the disease and the pattern of distribution. Lesions of the head and neck tend to be most responsive to treatment, whereas those on the extremities and genitalia tend to be more recalcitrant. Vitiligo treatments are summarized in Table 4.
| Treatment | Examples and comments |
|---|---|
| Sun protection | Hats, long-sleeved shirts, long pants, sunscreen |
| Cosmetic coverage | Concealers (e.g., Dermablend, Covermark) |
| Topical steroids | Topical steroid class II and III (e.g., betamethasone 0.05% [Diprolene], fluocinonide 0.05% [Lidex, brand no longer available in the United States]); head and neck most responsive to treatment |
| Phototherapy | Topical or oral psoralens with psoralen ultraviolet A-range, narrow-band ultraviolet-B therapy |
| Depigmentation | Monobenzone 20% cream (Benoquin) twice daily for six to 18 months |
| Surgical grafting | Mini-graft, punch-graft techniques; for localized, stable disease |
Treatment is multifaceted and may involve sun protection, cosmesis, topical steroids and immune modifiers, topical and oral psoralens and psoralen ultraviolet A-range (PUVA) therapy, narrow-band ultraviolet-B (UV-B) therapy, depigmentation therapy, and surgical grafting techniques.
Sun protection is important for patients with vitiligo. Sunscreens that contain avobenzone (Parsol 1789) or titanium dioxide provide broad-spectrum UV protection and should be used regularly, because affected skin is especially sensitive to sun exposure. Sun-protective clothing (e.g., wide-brimmed hats, long-sleeved shirts, long pants) will limit UV exposure as well. Cosmetic concealers (e.g., Dermablend, Covermark), topical dyes, and sunless self-tanning products (best on skin types II and III) may reduce the disparity in pigmentation to a more acceptable level.
High-potency topical steroids (classes II and III) have been found to be beneficial in facilitating repigmentation (in limited disease), with the face and neck being the most responsive. For more extensive disease, other options (e.g., topical or oral psoralens with PUVA therapy, narrow-band UV-B therapy with or without tacrolimus [Protopic]) may prove beneficial.32–44
Depigmentation therapy with monobenzone 20% cream (Benoquin) is reserved for patients with extensive (i.e., greater than 40 percent body surface area) involvements. Treatment is twice daily for six to 18 months, and patients must be counseled that its effects are irreversible, as melanocytes are permanently destroyed. Major side effects include contact or irritant dermatitis, pruritus, xerosis, and, less commonly, conjunctival melanosis and corneal pigment deposition. Sun protection is a mainstay of post-treatment care.
Patients with stable, localized vitiligo may elect to undergo surgical treatment of medically refractory lesions (e.g., hands, lips, genitalia). Multiple punch and mini-graft treatments are available.45
OTHER HYPOPIGMENTATION DISORDERS
Other disorders commonly associated with hypopigmentation include pityriasis alba, tinea versicolor, postinflammatory hypomelanosis (i.e., loss of melanin), atopic dermatitis, psoriasis, and guttate parapsoriasis. Additionally, it may also result from dermabrasion, chemical peels, and intralesional steroid therapy. A detailed description of these conditions is beyond the scope of this article and are described elsewhere.31 Table 5 provides a summary of common pigmentation disorders seen by family physicians.
| Disorder | Description | Location | Etiology | Treatment |
|---|---|---|---|---|
| Postinflammatory hyperpigmentatin | Irregular, darkly-pigmented macules or patches | Previous sites of injury or inflammation | Trauma, inflammation | Hydroquinone (Eldoquin Forte), azelaic acid (Azelex), retinoids, chemical peels, laser therapy; combination therapy is most effective |
| Melasma | Pigmented, well-defined macules; light brown, brown, or gray in color | Face (63 percent centrofacial, 21 percent malar, 16 percent mandibular), forearms | Pregnancy, oral contraceptives, phenytoin (Dilantin), idiopathic | Sunscreen; combinations of: hydroquinone, retinoids, glycolic acid peels, topical steroids; laser therapy, intense pulsed light therapy for dermal lesions |
| Solar lentigines | 1- to 3-cm macules, well-circumscribed, light yellow to dark brown, variegated color | Face, hands, forearms, chest, back, shins | Acute, chronic ultraviolet light exposure | Hydroquinone, retinoids, chemical peels, laser therapy, cryotherapy |
| Ephelides | 1- to 2-mm, shaply defined macules, red to tan to light brown in color | Childhood onset, face, neck, chest, arms, legs | Sun exposure in susceptible persons (i.e., skin types I to II) | None needed; fades in winter months |
| Café-au-lait macules | Tan to brown patches, 1 to 20 cm, epidermal, present at birth or early childhood | Usually on trunk, but possible anywhere | Increased melanin in melanocytes, basal keratinocytes | Laser therapy, surgical excision; cosmetic treatment |
| Vitiligo | Unpigmented macules and patches, sharply defined, 5 to 50 mm, coalescent | Face, hands, forearms, neck, genitalia, body folds, periorificial | Unknown, possibly immune-mediated | Sunscreens, concealers, dyes, topical steroids, oral psoralens with psoralen ultr]aviolet A-range, narrow-band ultraviolet-B therapy, depigmentation, grafting |